Abstract
Objective
The objective of this study is to discern patterns of serum sodium in a broad cohort of extremely low birth weight (ELBW) infants and associate those patterns with hospital outcomes.
Study Design
Retrospective cohort study of ELBW infants from 323 neonatal intensive care units (NICUs) discharged from 2004 to 2014. We included patients who survived at least 7 days and had daily sodium levels available, and categorized infants by their minimum and maximum sodium levels.
Results
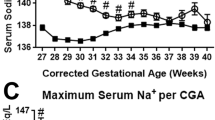
We identified 26,871 infants of whom 12,428 met inclusion criteria. Only 1964 (15.8%) maintained eunatremia for the first week. We found most dysnatremias to be associated with increased overall mortality compared with eunatremic patients including moderate hyponatremia (12.9% vs. 8.6%, p < 0.05) and severe hypernatremia (34.8% vs. 8.6%, p < 0.001). Most of these associations were maintained after regression modeling for mortality.
Conclusion
Sodium fluctuations occurring within the first week of life are associated with increased mortality.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Van Marter LJ, Leviton A, Allred EN, Pagano M, Kuban KC. Hydration during the first days of life and the risk of bronchopulmonary dysplasia in low birth weight infants. J Pediatr. 1990;116:942–9.
Costarino AT, Gruskay JA, Corcoran L, Polin RA, Baumgart S. Sodium restriction versus daily maintenance replacement in very low birth weight premature neonates: a randomized, blind therapeutic trial. J Pediatr. 1992;120:99–106.
Tammela OK, Koivisto ME. Fluid restriction for preventing bronchopulmonary dysplasia? Reduced fluid intake during the first weeks of life improves the outcome of low-birth-weight infants. Acta Paediatr. 1992;81:207–12.
Oh W, Poindexter BB, Perritt R, Lemons JA, Bauer CR, Ehrenkranz RA, et al. Association between fluid intake and weight loss during the first ten days of life and risk of bronchopulmonary dysplasia in extremely low birth weight infants. J Pediatr. 2005;147:786–90.
Bell EF, Warburton D, Stonestreet BS, Oh W. Effect of fluid administration on the development of symptomatic patent ductus arteriosus and congestive heart failure in premature infants. N Engl J Med. 1980;302:598–604.
Bell EF, Warburton D, Stonestreet BS, Oh W. High-volume fluid intake predisposes premature infants to necrotising enterocolitis. Lancet. 1979;2:90.
Oh W. Fluid and electrolyte management of very low birth weight infants. Pediatr Neonatol. 2012;53:329–33.
Hartnoll G. Basic principles and practical steps in the management of fluid balance in the newborn. Semin Neonatol. 2003;8:307–13.
Dalton J, Dechert RE, Sarkar S. Assessment of association between rapid fluctuations in serum sodium and intraventricular hemorrhage in hypernatremic preterm infants. Am J Perinatol. 2015;32:795–802.
Baraton L, Ancel PY, Flamant C, Orsonneau JL, Darmaun D, Roze JC. Impact of changes in serum sodium levels on 2-year neurologic outcomes for very preterm neonates. Pediatrics. 2009;124:e655–61.
Walker MW, Clark RH, Spitzer AR. Elevation in plasma creatinine and renal failure in premature neonates without major anomalies: terminology, occurrence and factors associated with increased risk. J Perinatol. 2011;31:199–205.
Baumgart S, Langman CB, Sosulski R, Fox WW, Polin RA. Fluid, electrolyte, and glucose maintenance in the very low birth weight infant. Clin Pediatr. 1982;21:199–206.
Fanaroff AA, Wald M, Gruber HS, Klaus MH. Insensible water loss in low birth weight infants. Pediatrics. 1972;50:236–45.
Gawlowski Z, Aladangady N, Coen PG. Hypernatraemia in preterm infants born at less than 27 weeks gestation. J Paediatr Child Health. 2006;42:771–4.
Elliott HC, Holley HL. Serum sodium and potassium values in 400 normal human subjects, determined by the Beckman flame photometer. Am J Clin Pathol. 1951;21:831–5.
Burtis CA, Ashwood ER, Bruns DE, eds. Tietz Textbook of Clinical Chemistry and Molecular Diagnostics. 5th ed. St. Louis, Missouri: Elsevier Saunders; 2011.
Spath C, Sjostrom ES, Ahlsson F, Agren J, Domellof M. Sodium supply influences plasma sodium concentration and the risk of hyper- and hyponatremia in extremely preterm infants. Pediatr Res. 2017;81:455–60.
Al-Dahhan J, Haycock GB, Nichol B, Chantler C, Stimmler L. Sodium homeostasis in term and preterm neonates: III. Effect of salt supplementation. Arch Dis Child. 1984;59:945–50.
Al-Dahhan J, Jannoun L, Haycock GB. Effect of salt supplementation of newborn premature infants on neurodevelopmental outcome at 10–13 years of age. Arch Dis Child Fetal Neonatal Ed. 2002;86:F120–3.
Kim YJ, Lee JA, Oh S, Choi CW, Kim EK, Kim HS, et al. Risk factors for late-onset hyponatremia and its influence on neonatal outcomes in preterm infants. J Korean Med Sci. 2015;30:456–62.
Acknowledgements
We thank Dr. Roy Haas for his contribution with initial data analysis. We thank Dr. Reese Clark for his critical feedback on this manuscript. The view(s) expressed herein are those of the author(s) and do not reflect the official policy or position of Brooke Army Medical Center, the U.S. Army Medical Department, the U.S. Army Office of the Surgeon General, the Department of the Air Force and Army, Department of Defense, or the U.S. Government.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Monnikendam, C.S., Mu, T.S., Aden, J.K. et al. Dysnatremia in extremely low birth weight infants is associated with multiple adverse outcomes. J Perinatol 39, 842–847 (2019). https://doi.org/10.1038/s41372-019-0359-0
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41372-019-0359-0
This article is cited by
-
Early fluid status and severe intraventricular hemorrhage or death in extremely preterm infants
Pediatric Nephrology (2025)
-
Maintenance intravenous fluid therapy in infants with sepsis and hyponatremia: a clinical trial
BMC Pediatrics (2024)
-
Thermoregulation, incubator humidity, and skincare practices in appropriate for gestational age ultra-low birth weight infants: need for more evidence
World Journal of Pediatrics (2024)
-
Neurodevelopmental consequences of early plasma sodium changes in very preterm infants
Pediatric Research (2022)
-
Association of early dysnatremia with mortality in the neonatal intensive care unit: results from the AWAKEN study
Journal of Perinatology (2022)