Abstract
Background
The optimal timing for discontinuation of nasogastric (NG) tube in premature infants transitioning to oral feeding is not known.
Objective
To determine whether early removal of NG-tube is appropriate in low-risk premature infants.
Methods
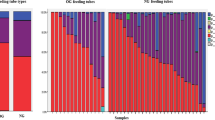
Prospectively collected data of premature infants started on oral feeds at ≤34 weeks gestation were reviewed. Infants were categorized into ‘early’ or ‘late’ NG-removal groups based on the proportion of oral intake in the preceding 2-days, i.e., 60–79% or 80–100% of the total volume, respectively.
Results
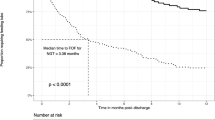
In total 50 infants in early group vs. 43 in late group. Both groups had similar oral intake and weight change in the subsequent 2-days post-NG removal. The days from NG-removal to target oral volume, and to hospital discharge trended shorter in early vs. late group.
Conclusions
Discontinuing NG-tube when the oral feeding competency reaches ~75% of prescribed feeding volume is safe and appropriate in low-risk premature infants.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Newborn AAoPCoFa. Hospital discharge of the high-risk neonate. Pediatrics. 2008;122:1119–26.
Jadcherla SR, Wang M, Vijayapal AS, Leuthner SR. Impact of prematurity and co-morbidities on feeding milestones in neonates: a retrospective study. J Perinatol. 2010;30:201–8.
Pickler RH, Reyna BA, Wetzel PA, Lewis M. Effect of four approaches to oral feeding progression on clinical outcomes in preterm infants. Nurs Res Pract. 2015;2015:716828.
Walsh MC, Bell EF, Kandefer S, Saha S, Carlo WA, D’angio CT, et al. Neonatal outcomes of moderately preterm infants compared to extremely preterm infants. Pedia Res. 2017;82:297–304.
Lainwala S, Kosyakova N, Power K, Hussain N, Moore JE, Hagadorn JI, et al. Delayed achievement of oral feedings is associated with adverse neurodevelopmental outcomes at 18 to 26 months follow-up in preterm infants. Am J Perinatol. 2019. https://doi.org/10.1055/s-0039-1681059. [Epub ahead of print]
Lau C, Smith EO, Schanler RJ. Coordination of suck-swallow and swallow respiration in preterm infants. Acta Paediatr. 2003;92:721–7.
Kirk AT, Alder SC, King JD. Cue-based oral feeding clinical pathway results in earlier attainment of full oral feeding in premature infants. J Perinatol. 2007;27:572–8.
Kamitsuka MD, Nervik PA, Nielsen SL, Clark RH. Incidence of nasogastric and gastrostomy tube at discharge is reduced after implementing an oral feeding protocol in premature (< 30 weeks) infants. Am J Perinatol. 2017;34:606–13.
Davidson E, Hinton D, Ryan-Wenger N, Jadcherla S. Quality improvement study of effectiveness of cue-based feeding in infants with bronchopulmonary dysplasia in the neonatal intensive care unit. J Obstet Gynecol Neonatal Nurs. 2013;42:629–40.
Greenspan JS, Wolfson MR, Holt WJ, Shaffer TH. Neonatal gastric intubation: differential respiratory effects between nasogastric and orogastric tubes. Pedia Pulmonol. 1990;8:254–8.
Bohnhorst B, Cech K, Peter C, Doerdelmann M. Oral versus nasal route for placing feeding tubes: no effect on hypoxemia and bradycardia in infants with apnea of prematurity. Neonatology. 2010;98:143–9.
Shiao SY, Youngblut JM, Anderson GC, DiFiore JM, Martin RJ. Nasogastric tube placement: effects on breathing and sucking in very-low-birth-weight infants. Nurs Res. 1995;44:82–88.
Peter CS, Wiechers C, Bohnhorst B, Silny J, Poets CF. Influence of nasogastric tubes on gastroesophageal reflux in preterm infants: a multiple intraluminal impedance study. J Pediatr. 2002;141:277–9.
Murthy SV, Funderburk A, Abraham S, Epstein M, DiPalma J, Aghai ZH. Nasogastric feeding tubes may not contribute to gastroesophageal reflux in preterm infants. Am J Perinatol. 2018;35:643–7.
Rogers SP, Hicks PD, Hamzo M, Veit LE, Abrams SA. Continuous feedings of fortified human milk lead to nutrient losses of fat, calcium and phosphorous. Nutrients. 2010;2:230–40.
Petersen SM, Greisen G, Krogfelt KA. Nasogastric feeding tubes from a neonatal department yield high concentrations of potentially pathogenic bacteria- even 1 d after insertion. Pediatr Res. 2016;80:395–400.
Jadcherla SR, Dail J, Malkar MB, McClead R, Kelleher K, Nelin L. Impact of process optimization and quality improvement measures on neonatal feeding outcomes at an all-referral neonatal intensive care unit. JPEN J Parent Enter Nutr. 2016;40:646–55.
Lau C. Development of infant oral feeding skills: what do we know? Am J Clin Nutr. 2016;103:616S–621S.
Latal-Hajnal B, von Siebenthal K, Kovari H, Bucher HU, Largo RH. Postnatal growth in VLBW infants: significant association with neurodevelopmental outcome. J Pediatr. 2003;143:163–70.
Fucile S, Phillips S, Bishop K, Jackson M, Yuzdepski T, Dow K. Identification of a pivotal period in the oral feeding progression of preterm infants. Am J Perinatol. 2019;36:530–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Viswanathan, S., Jadcherla, S. Transitioning from gavage to full oral feeds in premature infants: When should we discontinue the nasogastric tube?. J Perinatol 39, 1257–1262 (2019). https://doi.org/10.1038/s41372-019-0446-2
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41372-019-0446-2
This article is cited by
-
Turkish neonatal nurses’ knowledge regarding the enteral feeding in preterm infants: a descriptive, cross-sectional study
BMC Nursing (2025)
-
Oral-feeding guidelines for preterm neonates in the NICU: a scoping review
Journal of Perinatology (2021)