Abstract
Objective
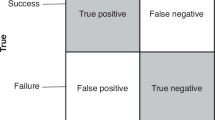
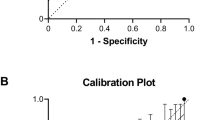
To develop an estimator for predicting successful extubation for an individual preterm infant.
Study design
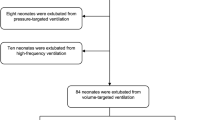
This was a retrospective study that included infants with birth weights ≤1250 g, who were admitted to a tertiary NICU over a 7-year period, received mechanical ventilation and had an elective extubation attempt within 60 days of age. Perinatal and periextubation characteristics were compared in the successful and failed extubation groups.
Results
Of 621 screened infants, 312 were included. Extubation succeeded in 73% and failed in 27%. Adjusted factors associated with successful extubation included greater gestational age, chronologic age, pre-extubation pH and lower pre-extubation FiO2, along with lower “peak” respiratory severity score in the first 6 h of age.
Conclusions
We used readily available demographic and clinical data to create an extubation readiness estimator that provides the probability of extubation success for an individual preterm infant (http://elasticbeanstalk-us-east-2-676799334712.s3-website.us-east-2.amazonaws.com/).
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Stoll BJ, Hansen NI, Bell EF, Walsh MC, Carlo WA, Shankaran S, et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates. 1993–2012. JAMA. 2015;314:1039–51.
Walsh MC, Morris BH, Wrage LA, Vohr BR, Pool WK, Tyson JE, et al. Extremely low birthweight neonates with protracted ventilation: mortality and 18-month neurodevelopmental outcomes. J Pediatr. 2005;146:798–804.
Sant’Anna GM, Keszler M. Weaning infants from mechanical ventilation. Clin Perinatol. 2012;39:543–62.
Miller JD, Carlo WA. Pulmonary complications of mechanical ventilation in neonates. Clin Perinatol. 2008;35:273–81. x-xi
Jensen EA, DeMauro SB, Kornhauser M, Aghai ZH, Greenspan JS, Dysart KC. Effects of multiple ventilation courses and duration of mechanical ventilation on respiratory outcomes in extremely low-birth-weight infants. JAMA Pediatr. 2015;169:1011–7.
Berger J, Mehta P, Bucholz E, Dziura J, Bhandari V. Impact of early extubation and reintubation on the incidence of bronchopulmonary dysplasia in neonates. Am J Perinatol. 2014;31:1063–72.
Chawla S, Natarajan G, Shankaran S, Carper B, Brion LP, Keszler M, et al. Markers of successful extubation in extremely preterm infants, and morbidity after failed extubation. J Pediatr. 2017;189:113–.e112.
Giaccone A, Jensen E, Davis P, Schmidt B. Definitions of extubation success in very premature infants: a systematic review. Arch Dis Child Fetal Neonatal Ed. 2014;99:F124–127.
Hermeto F, Martins BM, Ramos JR, Bhering CA, Sant’Anna GM. Incidence and main risk factors associated with extubation failure in newborns with birth weight <1250 grams. J Pediatr. 2009;85:397–402.
Kirpalani H, Millar D, Lemyre B, Yoder BA, Chiu A, Roberts RS. A trial comparing noninvasive ventilation strategies in preterm infants. N Engl J Med. 2013;369:611–20.
Epstein SK, Ciubotaru RL, Wong JB. Effect of failed extubation on the outcome of mechanical ventilation. Chest. 1997;112:186–92.
Baisch SD, Wheeler WB, Kurachek SC, Cornfield DN. Extubation failure in pediatric intensive care incidence and outcomes. Pedia Crit Care Med. 2005;6(May):312–8.
Manley BJ, Doyle LW, Owen LS, Davis PG. Extubating extremely preterm infants: predictors of success and outcomes following failure. J Pediatr. 2016;173:45–9.
Shalish W, Latremouille S, Papenburg J, Sant’Anna GM. Predictors of extubation readiness in preterm infants: a systematic review and meta-analysis [published online ahead of print March 8]. Arch Dis Child Fetal Neonatal Ed. 2019;104:F89–97. https://doi.org/10.1136/archdischild-2017-313878.
Al-Mandari H, Shalish W, Dempsey E, Keszler M, Davis PG, Sant’Anna G. International survey on periextubation practices in extremely preterm infants. Arch Dis Child Fetal Neonatal Ed. 2015;100:F428–431.
Tapia-Rombo CA, De León-Gómez N, Ballesteros-Del-Olmo JC, Ruelas-Vargas C, Cuevas-Urióstegui ML, Castillo-Pérez JJ. Predictors factors for the extubation failure in two or more times among preterm newborn. Rev Invest Clin. 2010;62:412–23.
Hiremath GM, Mukhopadhyay K, Narang A. Clinical risk factors associated with extubation failure in ventilated neonates. Indian Pediatr. 2009;46:887–90.
Bohn DJ, James I, Filler RM, Ein SH, Wesson DE, Shandling B, et al. The relationship between PaCO2 and ventilation parameters in predicting survival in congenital diaphragmatic hernia. J Pediatr Surg. 1984;19:666–71.
Ballard RA, Truog WE, Cnaan A, Martin RJ, Ballard PL, Merrill JD, et al. Inhaled nitric oxide in preterm infants undergoing mechanical ventilation. N Engl J Med. 2006;355:343–53.
Ballard JL, Khoury JC, Wedig K, Wang L, Eilers-Walsman BL, Lipp R. New Ballard Score, expanded to include extremely premature infants. J Pediatr. 1991;119:417–23.
Finer NN, Carlo WA, Walsh MC, Rich W, Gantz MG, Laptook AR, SUPPORT Study Group of the Eunice Kennedy Shriver NICHD Neonatal Research Network et al. Early CPAP versus surfactant in extremely preterm infants. N Engl J Med. 2010;362:1970–9.
Manley BJ, Owen LS, Doyle LW, Andersen CC, Cartwright DW, Pritchard MA, et al. High-flow nasal cannulae in very preterm infants after extubation. N Engl J Med. 2013;369:1425–33.
Dimitriou G, Fouzas S, Vervenioti A, Tzifas S, Mantagos S. Prediction of extubation outcome in preterm infants by composite extubation indices. Pediatr Crit Care Med. 2011;12:e242–249.
Kavvadia V, Greenough A, Dimitriou G. Prediction of extubation failure in preterm neonates. Eur J Pediatr. 2000;159:227–31.
Kamlin CO, Davis PG, Morley CJ. Predicting successful extubation of very low birthweight infants. Arch Dis Child Fetal Neonatal Ed. 2006;91:F180–183.
Chawla S, Natarajan G, Gelmini M, Kazzi SN. Role of spontaneous breathing trial in predicting successful extubation in premature infants. Pediatr Pulmonol. 2013;48:443–8.
Gillespie LM, White SD, Sinha SK, Donn SM. Usefulness of the minute ventilation test in predicting successful extubation in newborn infants: a randomized controlled trial. J Perinatol. 2003;23:205–7.
Mueller M, Almeida JS, Stanislaus R, Wagner CL. Can machine learning methods predict extubation outcome in premature infants as well as clinicians? J Neonatal Biol. 2013;2:1000118.
Vento G, Tortorolo L, Zecca E, Rosano A, Matassa PG, Papacci P, et al. Spontaneous minute ventilation is a predictor of extubation failure in extremely-low-birth-weight infants. J Matern Fetal Neonatal Med. 2004;15:147–54.
Kaczmarek J, Chawla S, Marchica C, Dwaihy M, Grundy L, Sant’Anna GM. Heart rate variability and extubation readiness in extremely preterm infants. Neonatology. 2013;104:42–48.
Laughon MM, Langer JC, Bose CL, Smith PB, Ambalavanan L, Kennedy KA, et al. Prediction of bronchopulmonary dysplasia by postnatal age in extremely premature infants. Am J Respir Crit Care Med. 2011;183:1715–22.
Kuzniewicz MW, Puopolo KM, Fischer A, Walsh EM, Li S, Newman TB, et al. A quantitative, risk-based approach to the management of neonatal early-onset sepsis. JAMA Pediatr. 2017;171:365–71.
Ferguson KN, Roberts CT, Manley BJ, Davis PG. Interventions to improve rates of successful extubation in preterm infants: a systematic review and meta-analysis. JAMA Pediatr. 2017;171:165–74.
Blackstone EH. Breaking down barriers: helpful breakthrough statistical methods you need to understand better. J Thorac Cardiovasc Surg. 2001;122(Sep):430–9.
Brunelli A, Rocco G. Internal validation of risk models in lung resection surgery: bootstrap versus training-and-test sampling. J Thorac Cardiovasc Surg. 2006;131(Jun):1243–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Gupta, D., Greenberg, R.G., Sharma, A. et al. A predictive model for extubation readiness in extremely preterm infants. J Perinatol 39, 1663–1669 (2019). https://doi.org/10.1038/s41372-019-0475-x
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41372-019-0475-x
This article is cited by
-
Accuracy of lung ultrasound in predicting successful extubation in preterm infants born ≤ 25 weeks
Journal of Perinatology (2025)
-
AI models in clinical neonatology: a review of modeling approaches and a consensus proposal for standardized reporting of model performance
Pediatric Research (2025)
-
Predictive model development for premature infant extubation outcomes: development and analysis
Pediatric Research (2025)
-
Association between the respiratory severity score and extubation success in severe bronchopulmonary dysplasia
Journal of Perinatology (2025)
-
Predictors of successful extubation from volume-targeted ventilation in extremely preterm neonates
Journal of Perinatology (2024)