Abstract
Objective
The objective of this study is to determine the resuscitation choices at 22–24 weeks gestation, related to whether mothers received antenatal counseling and the timing relative to delivery.
Study design
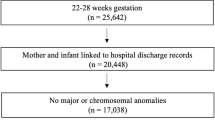
A retrospective chart review was performed of infants inborn at 22–24 weeks, over a 5-year period. Infants were excluded if they had major birth defects, were still hospitalized, or the consult occurred before 22 weeks.
Result
Of 121 infants born at 220–246 weeks, 91 were born to mothers who received a neonatology consult. For 80 infants resuscitated after consult, the median time between consult and delivery was 51.7 h (range: 0.1–366.3 h). For 11 infants who received comfort care after consult, the median time between consult and delivery was 20.0 h (range: 0.8–64.4 h).
Conclusions
After receiving counseling on the morbidity and mortality of delivery at 22–24 weeks, most parents chose resuscitation. Overall, 12–24 h between consult and delivery, parents were more likely to choose comfort care.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Singh J, Fanaroff J, Andrews B, Caldarelli L, Lagatta J, Plesha-Troyke S, et al. Resuscitation in the “gray zone” of viability: determining physician preferences and predicting infant outcomes. Pediatrics. 2007;120:519–26.
Younge N, Goldstein RF, Bann CM, Hintz SR, Patel RM, Smith PB, et al. Survival and neurodevelopmental outcomes among periviable infants. N Engl J Med. 2017;376:617–28.
Tyson JE, Parikh NA, Langer J, Green C, Higgins RD. Intensive care for extreme prematurity—moving beyond gestational age. N Engl J Med. 2008;358:1672–81.
Cummings J. Antenatal counseling regarding resuscitation and intensive care before 25 weeks of gestation. Pediatrics. 2015;136:588–95.
Partridge JC, Dickey BJ. Decision-making in neonatal intensive care: interventions on behalf of preterm infants. NeoReviews. 2009;10:e270–9.
Raju TN, Mercer BM, Burchfield DJ, Joseph GF Jr. Periviable birth: executive summary of a joint workshop by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, Society for Maternal-Fetal Medicine, American Academy of Pediatrics, and American College of Obstetricians and Gynecologists. Am J Obstet Gynecol. 2014;210:406–17.
American College of Obstetricians and Gynecologists, Society for Maternal-Fetal Medicine. Obstetric care consensus No. 6: periviable birth. Obstet Gynecol. 2017;130:e187.
Kaempf JW, Tomlinson MW, Campbell B, Ferguson L, Stewart VT. Counseling pregnant women who may deliver extremely premature infants: medical care guidelines, family choices, and neonatal outcomes. Pediatrics. 2009;123:1509–15.
Kukora S, Gollehon N, Laventhal N. Antenatal palliative care consultation: implications for decision-making and perinatal outcomes in a single-centre experience. Arch Dis Child Fetal Neonatal Ed. 2017;102:F12–6.
Griswold KJ, Fanaroff JM. An evidence-based overview of prenatal consultation with a focus on infants born at the limits of viability. Pediatrics. 2010;125:e931–7.
Janvier A, Lorenz JM, Lantos JD. Antenatal counselling for parents facing an extremely preterm birth: limitations of the medical evidence. Acta Paediatr. 2012;101:800–4.
Guillén Ú, Suh S, Munson D, Posencheg M, Truitt E, Zupancic JA, et al. Development and pretesting of a decision-aid to use when counseling parents facing imminent extreme premature delivery. J Pediatr. 2012;160:382–7.
Rysavy MA, Li L, Bell EF, Das A, Hintz SR, Stoll BJ, et al. Between-hospital variation in treatment and outcomes in extremely preterm infants. N Engl J Med. 2015;372:1801–11.
Acknowledgements
The authors wish to thank Bonnie Siner, RN, and Nancy Newman, RN, for their work in collecting institutional data, and Drs. Michelle Walsh and Jonathan Fanaroff for their review of the paper.
Funding
The only funding source to disclose is the institutional Clinical and Translational Science Award (CTSC, UL1TR002548), for use of REDCap.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Osborne, A., Fish, R. & C. Voos, K. Antenatal counseling in the gray zone of viability. J Perinatol 40, 1797–1801 (2020). https://doi.org/10.1038/s41372-020-00818-5
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41372-020-00818-5