Abstract
Objective
We investigated if volume guarantee (VG) ventilation in babies with hypoxic-ischemic encephalopathy (HIE) during interhospital transport decreases tidal volumes and prevents hypocapnia.
Study design
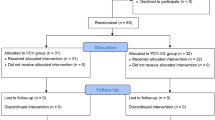
We computationally collected and analyzed ventilator data of babies ventilated with synchronized intermittent mandatory ventilation (SIMV) with VG (n = 28) or without VG (n = 8).
Result
The expiratory tidal volume of ventilator inflations was lower with SIMV-VG (median [IQR]: 4.9 [4.6–5.3] mL/kg) than with SIMV only (median [IQR]: 7.1 [5.3–8.0] mL/kg, p = 0.01). Babies receiving SIMV-VG had lower peak inflating pressures (median: 10.7 cmH2O, versus 17.5 cmH2O, p = 0.01). There was no significant difference in minute ventilation or in pCO2. Babies with strong spontaneous breathing had a mean PIP < 10 cmH2O but this did not result in adverse events or worsening of acidosis.
Conclusions
The use of VG ventilation in babies with HIE reduces tidal volumes and frequently results in very low inflating pressures without affecting pCO2.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Douglas-Escobar M, Weiss MD. Hypoxic-ischemic encephalopathy: a review for the clinician. JAMA Pediatr. 2015;169:397–403.
Liu L, Oza S, Hogan D, Chu Y, Perin J, Zhu J, et al. Global, regional, and national causes of under-5 mortality in 2000-15: an updated systematic analysis with implications for the Sustainable Development Goals. Lancet. 2016;388:3027–35.
Kurinczuk JJ, White-Koning M, Badawi N. Epidemiology of neonatal encephalopathy and hypoxic-ischaemic encephalopathy. Early Hum Dev. 2010;86:329–38.
Jacobs SE, Berg M, Hunt R, Tarnow-Mordi WO, Inder TE, Davis PG. Cooling for newborns with hypoxic-ischemic encephalopathy. Cochrane Database Syst Rev. 2013;1:CD003311.
Natarajan G, Pappas A, Shankaran S. Outcomes in childhood following therapeutic hypothermia for neonatal hypoxic-ischemic encephalopathy (HIE). Semin Perinatol. 2016;40:549–55.
Szakmar E, Jermendy A, El-Dib M. Respiratory management during therapeutic hypothermia for hypoxic-ischemic encephalopathy. J Perinatol. 2019;39:763–73.
Pfister RH, Bingham P, Edwards EM, Horbar JD, Kenny MJ, Inder T, et al. The Vermont Oxford Neonatal Encephalopathy Registry: rationale, methods, and initial results. BMC Pediatr. 2012;12:84.
Szakmar E, Kovacs K, Meder U, Bokodi G, Szell A, Somogyvari Z, et al. Asphyxiated neonates who received active therapeutic hypothermia during transport had higher rates of hypocapnia than controls. Acta Paediatr. 2018;107:1902–8.
Nadeem M, Murray D, Boylan G, Dempsey EM, Ryan CA. Blood carbon dioxide levels and adverse outcome in neonatal hypoxic-ischemic encephalopathy. Am J Perinatol. 2010;27:361–5.
Pappas A, Shankaran S, Laptook AR, Langer JC, Bara R, Ehrenkranz RA, et al. Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Hypocarbia and adverse outcome in neonatal hypoxic-ischemic encephalopathy. J Pediatr. 2011;158:752–8.
Lopez Laporte MA, Wang H, Sanon PN, Barbosa Vargas S, Maluorni J, Rampakakis E, et al. Association between hypocapnia and ventilation during the first days of life and brain injury in asphyxiated newborns treated with hypothermia. J Matern Fetal Neonatal Med. 2019;32:1312–20.
Klinger G, Beyene J, Shah P, Perlman M. Do hyperoxaemia and hypocapnia add to the risk of brain injury after intrapartum asphyxia? Arch Dis Child Fetal Neonatal Ed. 2005;90:49–52.
Greisen G, Munck H, Lou H. Severe hypocarbia in preterm infants and neurodevelopmental deficit. Acta Paediatr Scand. 1987;76:401–4.
Fritz KI, Zubrow A, Mishra OP, Delivoria-Papadopoulos M. Hypercapnia-induced modifications of neuronal function in the cerebral cortex of newborn piglets. Pediatr Res. 2005;57:299–304.
Gupta A, Keszler M. Survey of ventilation practices in the neonatal intensive care units of the United States and Canada: use of volume targeted ventilation and barriers to its use. Am J Perinatol. 2019;36:484–9.
Klingenberg C, Wheeler KI, McCallion N, Morley CJ, Davis PG. Volume-targeted versus pressure-limited ventilation in neonates. Cochrane Database Syst Rev. 2017;10:CD003666.
Peng W, Zhu H, Shi H, Liu E. Volume-targeted ventilation is more suitable than pressure-limited ventilation for preterm infants: a systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed. 2014;99:F158–65.
Bhat P, Chowdhury O, Shetty S, Hannam S, Rafferty GF, Peacock J, et al. Volume-targeted versus pressure-limited ventilation in infants born at or near term. Eur J Pediatr. 2016;175:89–95.
Keszler M, Abubakar K. Volume guarantee: stability of tidal volume and incidence of hypocarbia. Pediatr Pulmonol. 2004;38:240–5.
Keszler M. Volume-targeted ventilation: one size does not fit all. Evidence-based recommendations for successful use. Arch Dis Child Fetal Neonatal Ed. 2019;104:F108–12.
Azzopardi DV, Strohm B, Edwards AD, Dyet L, Halliday HL, Juszczak E, et al. Moderate hypothermia to treat perinatal asphyxial encephalopathy. N Engl J Med. 2009;361:1349–58.
Iyer NP, Mhanna MJ. Non-invasively derived respiratory severity score and oxygenation index in ventilated newborn infants. Pediatr Pulmonol. 2013;48:364–9.
Dassios T, Austin T. Respiratory function parameters in ventilated newborn infants undergoing whole body hypothermia. Acta Paediatr. 2014;103:157–61.
Herrera CM, Herrera CM, Gerhardt T, Claure N, Everett R, Musante G, et al. Effects of volume-guaranteed synchronized intermittent mandatory ventilation in preterm infants recovering from respiratory failure. Pediatrics. 2002;110:529–33.
Acknowledgements
We thank to Roland Hotz, Rainer Kühner, and the engineers of Acutronic for their help to export data from the Fabian ventilator. We thank to Dr Amanda Ogilvy-Stuart for her advice and comments on the paper.
Author information
Authors and Affiliations
Contributions
GB designed the study, wrote the computer programs to analyze ventilator data, performed the data analysis, and drafted the paper. LL, AB, and ZS performed the neonatal transfers and collected the clinical data. CJM helped with interpreting the findings. All authors revised and approved the final paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Lantos, L., Berenyi, A., Morley, C. et al. Volume guarantee ventilation in neonates treated with hypothermia for hypoxic-ischemic encephalopathy during interhospital transport. J Perinatol 41, 528–534 (2021). https://doi.org/10.1038/s41372-020-00823-8
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41372-020-00823-8