Abstract
Objective
Preterm infants frequently receive red cell transfusions; however, the effect of transfusions on cognition is unclear. We evaluated the relationship between transfusions and cognitive outcomes in preterm infants enrolled in a randomized trial of erythropoiesis stimulating agents (ESAs).
Study design
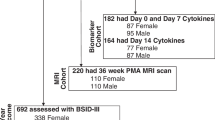
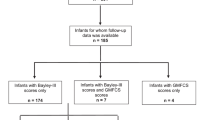
Preterm infants were randomized to ESAs or placebo during initial hospitalization, and transfusions recorded. Children were evaluated using standard developmental tests of cognition at 18–22 months (56 ESA, 24 placebo) and 3.5–4 years (39 ESA, 14 placebo).
Results
Cognitive scores at 18–22 months were inversely correlated with transfusion volume (p = 0.02). Among those receiving ≥1 transfusion, cognitive scores were significantly higher in the ESA-treated group (p = 0.003). At 3.5–4 years, transfusions were not correlated with cognitive scores.
Conclusions
In the placebo group, transfused children had lower cognitive scores than did non-transfused children at 18–22 months. In the ESA group, cognitive scores did not differ by transfusion status, suggesting ESAs might provide neuroprotection.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Jeon G, Sin J. Risk factors of transfusion in anemia of very low birth weight infants. Yonsei Med J. 2013;54:366–73.
Wang Y-C, Chan O-W, Chiang M-C, Yang P-H, Chu S-M, Hsu J-F, et al. Red blood cell transfusion and clinical outcomes in extremely low birth weight preterm infants. Pediatr Neonatol. 2017;58:216–22.
Valieva O, Strandjord T, Mayock D, Juul S. Effects of transfusions in extremely low birth weight infants: a retrospective study. J Pediatr. 2009;155:331–8.
Christensen R. Associations between “early” red blood cell transfusion and severe intraventricular hemorrhage, and between “late” red blood cell transfusion and necrotizing enterocolitis. Semin Perinatol. 2012;36:283–9.
Christensen R, Baer V, Lambert D, Ilstrup S, Eggert L, Henry E. Association, among very-low-birthweight neonates, between red blood cell transfusions in the week after birth and severe intraventricular hemorrhage. Transfusion. 2014;54:104–8.
Baer V, Lambert D, Henry E, Snow G, Butler A, Christensen R. Among very-low-birth-weight neonates is red blood cell transfusion an independent risk factor for subsequently developing a severe intraventricular hemorrhage? Transfusion. 2011;51:1170–8.
Ohlsson A, Aher SM. Early erythropoietin for preventing red blood cell transfusion in preterm and/or low birth weight infants. Cochrane Database Syst Rev. 2014;4:1–84.
Ohls R, Christensen R, Kamath-Rayne B, Rosenberg A, Wiedmeier S, Roohi M, et al. A randomized, masked, placebo-controlled study of darbepoetin alfa in preterm infants. Pediatrics. 2013;132:e119–27.
Ohls R, Kamath-Rayne B, Christensen R, Wiedmeier S, Rosenberg A, Fuller J, et al. Cognitive outcomes of preterm infants randomized to darbepoetin, erythropoietin, or placebo. Pediatrics. 2014;133:1023–30.
Ohls R, Cannon D, Phillips J, Caprihan A, Patel S, Winter S, et al. Preschool assessment of preterm infants treated with darbepoetin and erythropoietin. Pediatrics. 2016;137:1–11.
Carson J, Carless P, Hébert P. Outcomes using lower vs higher hemoglobin thresholds for red blood cell transfusion. JAMA. 2013;309:83–4.
Rohde J, Dimcheff D, Blumberg N, Saint S, Langa K, Kuhn L, et al. Health care–associated infection after red blood cell transfusion. JAMA. 2014;311:1317–26.
Patel N, Avlonitis V, Jones H, Reeves B, Sterne J, Murphy G. Indications for red blood cell transfusion in cardiac surgery: a systematic review and meta-analysis. Lancet Haematol. 2015;2:e543–53.
Murphy G, Pike K, Rogers C, Wordsworth S, Stokes E, Angelini G, et al. Liberal or restrictive transfusion after cardiac surgery. NEJM. 2015;372:997–1008.
Jairath V, Kahan B, Gray A, Doré C, Mora A, James M, et al. Restrictive versus liberal blood transfusion for acute upper gastrointestinal bleeding (TRIGGER): a pragmatic, open-label, cluster randomised feasibility trial. Lancet. 2015;386:137–44.
Fominskiy E, Putzu A, Monaco F, Scandroglio A, Karaskov A, Galas F, et al. Liberal transfusion strategy improves survival in perioperative but not in critically ill patients. A meta-analysis of randomised trials. Br J Anaesth. 2015;115:511–9.
Goobie S, Faraoni D, Zurakowski D, DiNardo J. Association of preoperative anemia with postoperative mortality in neonates. JAMA Pediatr. 2016;170:855–62.
Patel R, Knezevic A, Shenvi N, Hinkes M, Keene S, Roback J, et al. Association of red blood cell transfusion, anemia, and necrotizing enterocolitis in very low-birth-weight infants. JAMA. 2016;315:889–97.
dos Santos A, Guinsburg R, Branco de Almeida B, Procianoy R, Leone C, Marba S, et al. Red blood cell transfusions are independently associated with intra-hospital mortality in very low birth weight preterm infants. J Pediatr. 2011;159:371–6.
Whyte R, Kirpalani H. Low versus high haemoglobin concentration threshold for blood transfusion for preventing morbidity and mortality in very low birth weight infants (review). Cochrane Database Syst Rev. 2011;11:1–55.
Whyte R, Kirpalani H, Asztalos E, Andersen C, Blajchman M, Heddle N, et al. Neurodevelopmental outcome of extremely low birth weight infants randomly assigned to restrictive or liberal hemoglobin thresholds for blood transfusion. Pediatrics. 2009;123:207–13.
Neubauer A, Voss W, Wachtendorf M, Jungmann T. Erythropoietin improves neurodevelopmental outcome of extremely preterm infants. Ann Neurol. 2010;67:657–66.
Kirpalani H, Whyte R, Andersen C, Asztalos E, Heddle N, Blajchman M, et al. The premature infants in need of transfusion (pint) study: a randomized, controlled trial of a restrictive (low) versus liberal (high) transfusion threshold for extremely low birth weight infants. J Pediatr. 2006;149:301–7.
Bell E, Strauss R, Widness J, Mahoney L, Mock D, Seward V, et al. Randomized trial of liberal versus restrictive guidelines for red blood cell transfusion in preterm infants. Pediatrics. 2005;115:1685–91.
Nopoulous P, Conrad A, Bell E, Strauss R, Widness J, Magnotta V, et al. Long-term outcome of brain structure in premature infants: effects of liberal vs restricted red blood cell transfusions. Arch Pediatr Adolesc Med. 2011;165(May):443–50.
Kirpalani H, Bell EF, Hintz SR, Tan S, Schmidt B, Chaudhary AS, et al. Higher or lower hemoglobin transfusion thresholds for preterm infants. N Engl J Med. 2020;383:2639–51.
Franz AR, Engel C, Bassler D, Rudiger M, Thorne UH, Maier RF, et al. Effects of liberal vs restrictive transfusion thresholds on survival and neurocognitive outcomes in extremely low-birth-weight infants: the ETTNO randomized clinical trial. JAMA. 2020;324:560–70.
Fauchere J, Koller B, Tschopp A, Dame C, Ruegger C, Bucher H. Safety of early high-dose recombinant erythropoietin for neuroprotection in very preterm infants. J Pediatr. 2015;167:52–7.
Rangarajan V, Juul S. Erythropoietin: emerging role of erythropoietin in neonatal neuroprotection. Pediatr Neurol. 2014;51:481–8.
Leuchter R, Gui L, Poncet A, Hagmann C, Lodygensky G, Martin E, et al. Association between early administration of high-dose erythropoietin in preterm infants and brain MRI abnormality at term-equivalent age. JAMA. 2014;312:817–24.
O’Gorman R, Bucher H, Held U, Koller B, Huppi P, Hagmann C, et al. Tract-based spatial statistics to assess the neuroprotective effect of early erythropoietin on white matter development in preterm infants. Brain. 2015;138:388–97.
Dani C, Poggi C, Gozzini E, Leonardi V, Serent A, Abbate R, et al. Red blood cell transfusions can induce proinflammatory cytokines in preterm infants. Transfusion. 2017;57:1304–10.
Acknowledgements
The authors wish to thank the research coordinators and bedside nurses involved in the original randomized study. We also wish to thank Sarah Peceny and Sean Gonzales for subject coordination, and Michael Steffen, Ron Yeo, and Richard Campbell for developmental follow-up and statistical assistance. We are indebted to the parents for their willingness to allow their children to participate in this study. Finally, we wish to acknowledge US taxpayers for providing the funding to support the National Institutes of Health and this study.
Funding
Supported by grants from the NIH NICHD (R01 HD059856), the University of New Mexico Clinical Translational Science Center (UL1 TR000041), the University of Utah Center for Clinical and Translational Sciences (UL1TR001067), Thrasher Research Fund, and the University of New Mexico Department of Pediatrics.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shah, P., Cannon, D.C., Lowe, J.R. et al. Effect of blood transfusions on cognitive development in very low birth weight infants. J Perinatol 41, 1412–1418 (2021). https://doi.org/10.1038/s41372-021-00997-9
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41372-021-00997-9
This article is cited by
-
Association of blood component transfusions with neurodevelopmental impairment in preterm infants by gestational age
Pediatric Research (2025)
-
Three studies needed to inform the design of the U-BET (umbilical cord blood for extremely low-gestational-age transfusions) clinical trial
Journal of Perinatology (2025)
-
Neurodevelopmental outcomes after red cell transfusion exposure in male versus female extremely preterm infants
Pediatric Research (2025)
-
New frontiers in neonatal red blood cell transfusion research
Journal of Perinatology (2023)