Abstract
Objective
To assess if the adjusted odds of low composite cognitive Bayley-III scores changed after implementing a single-institution quality improvement (QI) project designed to decrease discharge Z-scores for weight, body mass index (BMI), and weight-for-length, but not length or fronto-occipital circumference (FOC) in infants 23–28 weeks gestational age (GA).
Methods
Compare Bayley-III outcomes at ≥18 months corrected age (postnatal age adjusted for prematurity) in infants tested before (Epoch-1) and after (Epoch-2) QI implementation.
Results
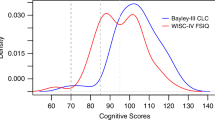
Bayley testing was available in 134/156 infants (86%) in Epoch-1 and 139/175 (79%) in Epoch-2. There was no change in frequency of low (<85) cognitive score (p = 0.5) or in median cognitive scores (80 in Epoch-1 vs. 85 Epoch-2, p = 0.35). The adjusted odds of low cognitive scores was not different between Epochs.
Conclusion
No change in cognitive outcome at ≥18 months corrected age was observed after implementing a QI project designed to reduce discharge weight-for-length disproportion in very preterm infants.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Agarwal PK, Shi L, Rajadurai VS, Zheng Q, Yang PH, Khoo PC, et al. Factors affecting neurodevelopmental outcome at 2 years in very preterm infants below 1250 grams: a prospective study. J Perinatol. 2018;38:1093–100.
Belfort MB, Rifas-Shiman SL, Sullivan T, Collins CT, McPhee AJ, Ryan P, et al. Infant growth before and after term: effects on neurodevelopment in preterm infants. Pediatrics. 2011;128:e899–906.
Asztalos EV, Church PT, Riley P, Fajardo C, Shah PS, Canadian Neonatal N, et al. Neonatal factors associated with a good neurodevelopmental outcome in very preterm infants. Am J Perinatol. 2017;34:388–96.
Bauer SE, Schneider L, Lynch SK, Malleske DT, Shepherd EG, Nelin LD. Factors associated with neurodevelopmental impairment in bronchopulmonary dysplasia. J Pediatr. 2020;218:22–7 e2.
Belfort MB, Kuban KC, O’Shea TM, Allred EN, Ehrenkranz RA, Engelke SC, et al. Weight status in the first 2 years of life and neurodevelopmental impairment in extremely low gestational age newborns. J Pediatr. 2016;168:30–5 e32.
Cormack BE, Harding JE, Miller SP, Bloomfield FH. The influence of early nutrition on brain growth and neurodevelopment in extremely preterm babies: a narrative review. Nutrients. 2019;11:2029.
Ehrenkranz RA, Dusick AM, Vohr BR, Wright LL, Wrage LA, Poole WK. Growth in the neonatal intensive care unit influences neurodevelopmental and growth outcomes of extremely low birth weight infants. Pediatrics. 2006;117:1253–61.
Georgieff MK, Ramel SE, Cusick SE. Nutritional influences on brain development. Acta Paediatr. 2018;107:1310–21.
Nash A, Dunn M, Asztalos E, Corey M, Mulvihill-Jory B, O’Connor DL. Pattern of growth of very low birth weight preterm infants, assessed using the WHO Growth Standards, is associated with neurodevelopment. Appl Physiol Nutr Metab. 2011;36:562–9.
Duncan AF, Heyne RJ, Morgan JS, Ahmad N, Rosenfeld CR. Elevated systolic blood pressure in preterm very-low-birth-weight infants ≤ 3 years of life. Pediatr Nephrol. 2011;26:1115–21.
Frankfurt JA, Duncan AF, Heyne RJ, Rosenfeld CR. Renal function and systolic blood pressure in very-low-birth-weight infants 1-3 years of age. Pediatr Nephrol. 2012;27:2285–91.
Duncan AF, Frankfurt JA, Heyne RJ, Rosenfeld CR. Biomarkers of adiposity are elevated in preterm very-low-birth-weight infants at 1, 2 and 3 Y of age. Pediadtr Res. 2017;81:780–6.
Wickland J, Heyne R, Brown LS, Turer CB, Rosenfeld CR. Preterm very-low-birthweight (PT-VLBW) infants continue to exhibit high systolic blood pressure (SBP) and altered renal function at preadolescence. Presentation at AAP 94th Perinatal and developmental medicine symposium, Snow Mass, CO, June, 2019.
Meyers JM, Tan S, Bell EF, Duncan AF, Guillet R, Stoll BJ, et al. Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Neurodevelopmental outcomes among extremely premature infants with linear growth restriction. J Perinatol. 2019;39:193–202.
Belfort MB, Gillman MW, Buka SL, Casey PH, McCormick MC. Preterm infant linear growth and adiposity gain: trade-offs for later weight status and intelligence quotient. J Pediatr. 2013;163:1564–9 e2.
Rozé JC, Darmaun D, Boquien CY, Flamant C, Picaud JC, Savagner C, et al. The apparent breastfeeding paradox in very preterm infants: relationship between breast feeding, early weight gain and neurodevelopment based on results from two cohorts, EPIPAGE and LIFT. BMJ Open. 2012;2:e000834.
Franz AR, Pohlandt F, Bode H, Mihatsch WA, Sander S, Kron M, et al. Intrauterine, early neonatal, and postdischarge growth and neurodevelopmental outcome at 5.4 years in extremely preterm infants after intensive neonatal nutritional support. Pediatrics. 2009;123:e101–9.
Neubauer V, Fuchs T, Griesmaier E, Kager K, Pupp-Peglow U, Kiechl-Kohlendorfer U. Poor postdischarge head growth is related to a 10% lower intelligence quotient in very preterm infants at the chronological age of five years. Acta Paediatr. 2016;105:501–7.
Neubauer V, Griesmaier E, Pehböck-Walser N, Pupp-Peglow U, Kiechl-Kohlendorfer U. Poor postnatal head growth in very preterm infants is associated with impaired neurodevelopment outcome. Acta Paediatr. 2013;102:883–8.
Pavageau L, Whitham J, Rosenfeld CR, Heyne RJ, Brown LS, Brion LP. Valid serial length measurements in preterm infants permit characterization of growth patterns. J Perinatol. 2018;38:1694–70.
Brion LP, Rosenfeld CR, Heyne RJ, Brown SL, Lair CS, Burchfield PJ, et al. Adjustable feedings plus accurate serial length measurements decrease discharge weight-length disproportion in very preterm infants: quality improvement project. J Perinatol. 2019;39:1131–9.
Brion LP, Heyne R, Brown LS, Lair CS, Edwards A, Burchfield PJ, et al. Zinc deficiency limiting head growth to discharge in extremely low gestational age infants with insufficient linear growth: a cohort study. J Perinatol. 2020;40:1694–704.
Brion LP, Rosenfeld CR, Heyne R, Brown LS, Lair CS, Heyne E, et al. Association of age of initiation and type and of complementary foods with body mass index and weight-length at twelve months of age in preterm infants. J Perinatol. 2020;40:1394–404.
Albers CA, Grieve AJ. Bayley scales of infant and toddler development, 3rd edition. J Psychoeduc Assess. 2007;25:180–90.
Olsen IE, Groveman SA, Lawson ML, Clark RH, Zemel BS. New intrauterine growth curves based on United States data. Pediatrics 2010;125:e214–24.
Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001;163:1723–9.
Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. 1978;92:529–34.
Kliegman RM, Walsh MC. Neonatal necrotizing enterocolitis: pathogenesis, classification, and spectrum of illness. Curr Probl Pediatr. 1987;17:213–88.
WHO Multicentre Growth Reference Study Group. WHO Child Growth Standards based on length/height, weight and age. Acta Paediatr. 2006;450:76.
Olsen IE, Lawson ML, Ferguson AN, Cantrell R, Grabich SC, Zemel BS, et al. BMI curves for preterm infants. Pediatrics. 2015;135:e572–81.
Albers CA, Grieve AJ. Test Review: Bayley, N. Bayley Scales of Infant and Toddler Development–Third Edition. San Antonio, TX: Harcourt Assessment. J Psychoeducational Assess. 2007;25:180–90.
Duncan AF, Bann C, Boatman C, Hintz SR, Vaucher YE, Vohr BR, et al. Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Do currently recommended Bayley-III cutoffs overestimate motor impairment in infants born <27 weeks gestation? J Perinatol. 2015;35:516–21.
Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996;49:1373–9.
Schreiber-Gregory D. Multicollinearity: what is it, why should we care, and how can it be controlled? Paper 1404–2017. http://support.sas.com/resources/papers/proceedings17/1404-2017.pdf. Accessed 20 Feb 2021.
Underwood MA. Human milk for the premature infant. Pediatr Clin North Am. 2013;60:189–207.
American Academy of Pediatrics Section on Breastfeeding. Breastfeeding and the use of human milk. Pediatrics 2012;129:e827–41.
Patra K, Hamilton M, Johnson TJ, Greene M, Dabrowski E, Meier PP, et al. NICU human milk dose and 20-month neurodevelopmental outcome in very low birth weight infants. Neonatology. 2017;112:330–6.
Fenton TR, Cormack B, Goldberg D, Nasser R, Alshaikh B, Eliasziw M, et al. “Extrauterine growth restriction” and “postnatal growth failure” are misnomers for preterm infants. J Perinatol. 2020;40:704–14.
Simon L, Théveniaut C, Flamant C, Frondas-Chauty A, Darmaun D, Rozé JC. In preterm infants, length growth below expected growth during hospital stay predicts poor neurodevelopment at 2 years. Neonatology. 2018;114:135–41.
Ramel SE, Demerath EW, Gray HL, Younge N, Boys C, Georgieff MK. The relationship of poor linear growth velocity with neonatal illness and two-year neurodevelopment in preterm infants. Neonatology. 2012;102:19–24.
Brion LP, Heyne R, Lair CS. Role of zinc in neonatal growth and brain growth: review and scoping review. Pediatr Res. 2020. https://doi.org/10.1038/s41390-020-01181-z. correction https://doi.org/10.1038/s41390-021-01425-6.
Acknowledgements
Preliminary data were published, presented or both as follows: Reis J, Tolentino-Plata K, Heyne R, Rosenfeld CR, Brion LP. Does Reducing Weight-For-Length Disproportion at Discharge in Preterm Neonates Affect Neurodevelopmental Outcomes? Presentation at 41st Western Conference on Perinatal Research, Renaissance Esmeralda Resort, Indian Wells, California, January 9, 2020. Reis J, Tolentino-Plata K, Heyne R, Rosenfeld CR, Caraig M, Brion LP. Does Reducing Weight-For-Length Disproportion at Discharge in Preterm Neonates Affect Neurodevelopmental Outcomes? Accepted for poster presentation at PAS, Philadelphia, PA, 5/2/2020; canceled for COVID-19/SARS-Cov-2; presented online at Virtual Regional Neonatal Research Conference 5/26/2020. Reis J, Tolentino-Plata K, Heyne R, Brown LS, Rosenfeld CR, Caraig M, Burchfield PJ, Brion LP. A Quality Improvement (QI) Project Designed to Reduce Weight-For-Length (WtFL) Disproportion at Hospital Discharge in Extremely Low Gestational Age Neonates (ELGANs) Did Not Affect Cognitive Neurodevelopmental Outcomes. Submitted to Annual PAS Meeting 2021.
Funding
George L. MacGregor Professorship (CRR) and Children’s Medical Center Clinical Advisory Committee (CCRAC)—Senior Investigator Research Award—New Direction (LPB).
Author information
Authors and Affiliations
Contributions
JDR, RH, CRR, and LPB conceptualized and designed the study. JDR wrote the first draft of the manuscript. KTP conducted the Bayley score assessments. MC was the research coordinator for the QI project. PJB collected and entered data into the NICU database. LSB conducted statistical analyses. All authors participated in the interpretation of the data, critically reviewed the revisions, and approved the final manuscript as submitted.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical approval
The original QI project, including follow-up, received approval by the Institutional Review Board (IRB) of the University of Texas Southwestern Medical Center, Parkland Health and Hospital Systems and Children’s Medical Center. Informed consent was obtained for all infants in the study who had follow-up at the Thrive clinic.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Reis, J.D., Tolentino-Plata, K., Heyne, R. et al. Quality improvement project designed to reduce disproportionate growth in extremely low gestational age neonates: cognitive neurodevelopmental outcome at 18–41 months. J Perinatol 41, 1050–1058 (2021). https://doi.org/10.1038/s41372-021-01047-0
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41372-021-01047-0
This article is cited by
-
A validated NICU database: recounting 50 years of clinical growth, quality improvement and research
Pediatric Research (2024)
-
Double-blinded randomized controlled trial of optimizing nutrition in preterm very low birth weight infants: Bayley scores at 18–38 months of age
Journal of Perinatology (2023)