Abstract
Objective
To evaluate acute stress disorder (ASD) symptoms and their predictors in Neonatal Intensive Care Unit (NICU) mothers.
Study design
In this cross-sectional study, 119 mothers (~72% Medicaid) completed surveys during the first month of their infants’ hospitalizations. Correlations and structural equation models (SEMs) evaluated relations among mothers’ childhood trauma history, infant health appraisals, objective infant health, and ASD.
Result
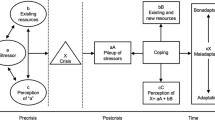
ASD symptoms (~55%) and childhood trauma (~33%) were prevalent. ASD was correlated with childhood trauma, infant health, and infant health appraisals. All SEMs had good fit, indicating that (a) infant health appraisals partially mediated relations between childhood trauma and ASD, and (b) infant health appraisals fully mediated relations between objective infant health and ASD.
Conclusion
ASD symptoms are prevalent among NICU mothers regardless of infant health severity. Recognition of childhood trauma history and appraisals of infant health is critical for trauma-informed care.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
World Health Organization (WHO). https://www.who.int/mental_health/maternal-child/maternal_mental_health/en/.
Lefkowitz DS, Baxt C, Evans JR. Prevalence and correlates of posttraumatic stress and postpartum depression in parents of infants in the neonatal intensive care unit (NICU). J Clin Psychol Med Settings 2010;17:230–7. https://doi.org/10.1007/s10880-010-9202-7.
Misund AR, Nerdrum P, Diseth TH Mental health in women experiencing preterm birth. BMC Pregnancy Childbirth. 2014;14. https://doi.org/10.1186/1471-2393-14-263.
Shaw RJ, Deblois T, Ikuta L, Ginzburg K, Fleisher B, Koopman C. Acute stress disorder among parents of infants in the neonatal intensive care nursery. Psychosomatics. 2006;47:206–12. https://doi.org/10.1176/appi.psy.47.3.206.
Shaw RJ, Bernard RS, Deblois T, Ikuta LM, Ginzburg K, Koopman C. the relationship between acute stress disorder and posttraumatic stress disorder in the neonatal intensive care unit. Psychosomatics. 2009;50:131–7. https://doi.org/10.1176/appi.psy.50.2.131.
Premature Birth. Center for Disease Control (CDC) and Prevention. https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pretermbirth.htm. Published 2019.
Diagnostic and statistical manual of mental disorders: DSM-5. 5th ed. Arlington, VA: American Psychiatric Association; 2013.
Holzman C, Eyster J, Kleyn M, et al. Maternal weathering and risk of preterm delivery. Am J Public Health. 2009;99:1864–71. https://doi.org/10.2105/ajph.2008.151589.
Love C, David RJ, Rankin KM, Collins JW. Exploring weathering: effects of lifelong economic environment and maternal age on low birth weight, small for gestational age, and preterm birth in African-American and White Women. Am J Epidemiol. 2010;172:127–34. https://doi.org/10.1093/aje/kwq109.
Roque ATF, Lasiuk GC, Radünz V, Hegadoren K. Scoping review of the mental health of parents of infants in the NICU. J Obstet, Gynecol Neonatal Nurs. 2017;46:576–87. https://doi.org/10.1016/j.jogn.2017.02.005.
Hynan MT, Mounts KO, Vanderbilt DL. Screening parents of high-risk infants for emotional distress: rationale and recommendations. J Perinatol. 2013;33:748–53. https://doi.org/10.1038/jp.2013.72.
Sanders MR, Hall SL. Trauma-informed care in the newborn intensive care unit: promoting safety, security and connectedness. J Perinatol. 2017;38:3–10. https://doi.org/10.1038/jp.2017.124.
National Perinatal Association. Psychologists in the NICU. http://www.nationalperinatal.org/psychologists.
Kazak AE, Kassam-Adams N, Schneider S, Zelikovsky N, Alderfer MA, Rourke M. An integrative model of pediatric medical traumatic stress. J Pediatr Psychol 2005;31:343–55. https://doi.org/10.1093/jpepsy/jsj054.
Schetter CD. Psychological science on pregnancy: stress processes, biopsychosocial models, and emerging research issues. Annu Rev Psychol. 2011;62:531–58. https://doi.org/10.1146/annurev.psych.031809.130727.
Feeley N, Zelkowitz P, Cormier C, Charbonneau L, Lacroix A, Papageorgiou A. Posttraumatic stress among mothers of very low birthweight infants at 6 months after discharge from the neonatal intensive care unit. Appl Nurs Res. 2011;24:114–7. https://doi.org/10.1016/j.apnr.2009.04.004.
Felitti VJ, Anda RF The relationship of adverse childhood experiences to adult medical disease, psychiatric disorders and sexual behavior: implications for healthcare. The Impact of Early Life Trauma on Health and Disease. 2010:77–87. https://doi.org/10.1017/cbo9780511777042.010.
Smith MV, Gotman N, Yonkers KA. Early childhood adversity and pregnancy outcomes. Matern Child Health J. 2016;20:790–8. https://doi.org/10.1007/s10995-015-1909-5.
Witt WP, Cheng ER, Wisk LE, et al. Preterm birth in the United States: the impact of stressful life events prior to conception and maternal age. Am J Public Health. 2014;104:S73–S80. https://doi.org/10.2105/ajph.2013.301688.
Choi KW, Sikkema KJ. Childhood maltreatment and perinatal mood and anxiety disorders: A systematic review. Trauma Violence Abus. 2016;17:427–53. https://doi.org/10.1177/1524838015584369.
Hughes K, Bellis MA, Hardcastle KA, et al. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lancet Public Health. 2017;2:e356–e366. https://doi.org/10.1016/S2468-2667(17)30118-4.
Barr P. Acute traumatic stress in neonatal intensive care unit parents: relation to existential emotion-based personality predispositions. J Loss Trauma. 2010;15:106–22. https://doi.org/10.1080/15325020903373128.
Greene MM, Rossman B, Patra K, Kratovil AL, Janes JE, Meier PP. Depression, anxiety, and perinatal-specific posttraumatic distress in mothers of very low birth weight infants in the neonatal intensive care unit. J Dev Behav Pediatrics. 2015;36:362–70. https://doi.org/10.1097/dbp.0000000000000174.
Aftyka A, Rybojad B, Rozalska-Walaszek I, Rzoñca P, Humeniuk E. Post-traumatic stress disorder in parents of children hospitalized in the neonatal intensive care unit (NICU): Medical and demographic risk factors. Psychiatr Danubina. 2014;26:347–52.
Vanderbilt D, Bushley T, Young R, Frank DA. Acute posttraumatic stress symptoms among urban mothers with newborns in the neonatal intensive care unit: a preliminary study. J Dev BehavPediatrics. 2009;30:50–5. https://doi.org/10.1097/dbp.0b013e318196b0de.
Aftyka A, Rybojad B, Rosa W, Wróbel A, Karakuła-Juchnowicz H. Risk factors for the development of post-traumatic stress disorder and coping strategies in mothers and fathers following infant hospitalisation in the neonatal intensive care unit. J Clin Nurs. 2017;26:4436–45. https://doi.org/10.1111/jocn.13773.
Chang H-P, Chen J-Y, Huang Y-H, et al. Factors associated with post-traumatic symptoms in mothers of preterm infants. Arch Psychiatr Nurs. 2016;30:96–101. https://doi.org/10.1016/j.apnu.2015.08.019.
Kim WJ, Lee E, Kim KR, Namkoong K, Park ES, Rha D-W. Progress of PTSD symptoms following birth: A prospective study in mothers of high-risk infants. J Perinatol. 2015;35:575–9. https://doi.org/10.1038/jp.2015.9.
Patel RM, Rysavy MA. Global variation in neonatal intensive care: does it matter? J Pediatrics 2016;177:6–7. https://doi.org/10.1016/j.jpeds.2016.06.019.
Bruce MA. Systematic and conceptual review of posttraumatic stress in childhood cancer survivors and their parents. Clin Psychol Rev. 2006;26:233–56. https://doi.org/10.1016/j.cpr.2005.10.002.
Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of Childhood Abuse and Household Dysfunction to Many of the Leading Causes of Death in Adults. Am J Prev Med 1998;14:245–58. https://doi.org/10.1016/s0749-3797(98)00017-8.
Byrne BM Structural Equation Modeling with EQS and EQS/Windows. Thousand Oaks, CA: Sage; 1994.
Weiss DS, Marmar CR. The impact of event scale-revised. In: Wilson JP, Keane TM, eds. Assessing psychological trauma and PTSD. New York, NY: The Guilford Press; 2006. p. 399–411.
Weiss DS The impact of event scale: Revised. In: Wilson JP, Tang CS-kum, eds. Cross-Cultural Assessment of Psychological Trauma and PTSD. Boston, MA: Springer; 2007:219–38.
Medicaid. Retrieved from: https://www.benefits.gov/benefit/1643.
Harsha SS SNAPPE-II (Score for Neonatal Acute Physiology with Perinatal Extension-II) in Predicting Mortality and Morbidity in NICU. Journal Of Clinical And Diagnostic Research. 2015. https://doi.org/10.7860/jcdr/2015/14848.6677.
Pai ALH, Patiño-Fernández AM, Mcsherry M, et al. The psychosocial assessment tool: psychometric properties of a screener for psychosocial distress in families of children newly diagnosed with cancer. J Pediatr Psychol. 2007;33:50–62.
Tabachnick BG, Fidell LS Using Multivariate Statistics, 5th Ed. Boston, MA: Pearson Education; 2007.
IBM Corp. IBM SPSS Statistics for Windows, Version 24.0. Armonk, NY: IBM Corp; 2016.
Hu LT, Bentler PM Evaluating model fit. In: Hoyle RH, ed. Structural equation modeling: concepts, issues, and applications. Thousand Oaks, CA: Sage; 2000:76–99.
Kline RB Principles and practice of structural equation modeling. New York, NY: The Guilford Press; 2016.
Callahan JL, Borja SE, Hynan MT. Modification of the perinatal PTSD questionnaire to enhance clinical utility. J Perinatol. 2006;26:533–9. https://doi.org/10.1038/sj.jp.7211562.
Acknowledgements
We would first like to acknowledge the NICU families who agreed to participate in this study during a scary and stressful time in their lives. In addition, we would like to acknowledge the VCU Medical Team who supported this study and its clinical implications, including nursing, physicians, speech language pathologists, physical therapists, occupational therapist, social work and chaplaincy.
Author information
Authors and Affiliations
Contributions
ABW contributed to study design, data collection, data analysis, and manuscript write-up. KDH-M contributed to study design, participant recruitment, communication with medical team, and manuscript edits. ABP-A contributed to data collection and manuscript edits. SG contributed to data analysis and manuscript edits. RW contributed to data collection and manuscript edits. PBP contributed to data analysis and manuscript edits. BR contributed to study design and manuscript edits. AW contributed to study design, data collection, and manuscript edits.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethics approval and consent to participate
All participants provided informed consent to participate in the study. Virginia Commonwealth University’s International Review Board approved this study (Protocol #: HM20011668).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Williams, A.B., Hendricks-Muñoz, K.D., Parlier-Ahmad, A.B. et al. Posttraumatic stress in NICU mothers: modeling the roles of childhood trauma and infant health. J Perinatol 41, 2009–2018 (2021). https://doi.org/10.1038/s41372-021-01103-9
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41372-021-01103-9
This article is cited by
-
The effect of paternal anxiety on mother-infant bonding in neonatal intensive care
BMC Pregnancy and Childbirth (2024)
-
Factors associated with posttraumatic stress and anxiety among the parents of babies admitted to neonatal care: a systematic review
BMC Pregnancy and Childbirth (2024)