Abstract
Objectives
To examine characteristics and outcomes of T18 and T13 infants receiving intensive surgical and medical treatment compared to those receiving non-intensive treatment in NICUs.
Study design
Retrospective cohort of infants in the Children’s Hospitals National Consortium (CHNC) from 2010 to 2016 categorized into three groups by treatment received: surgical, intensive medical, or non-intensive.
Results
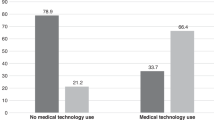
Among 467 infants admitted, 62% received intensive medical treatment; 27% received surgical treatment. The most common surgery was a gastrostomy tube. Survival in infants who received surgeries was 51%; intensive medical treatment was 30%, and non-intensive treatment was 72%. Infants receiving surgeries spent more time in the NICU and were more likely to receive oxygen and feeding support at discharge.
Conclusions
Infants with T13 or T18 at CHNC NICUs represent a select group for whom parents may have desired more intensive treatment. Survival to NICU discharge was possible, and surviving infants had a longer hospital stay and needed more discharge supports.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Nelson KE, Hexem KR, Feudtner C. Inpatient Hospital Care of Children With Trisomy 13 and Trisomy 18 in the United States. Pediatrics 2012;129:869–76.
Acharya K, Leuthner S, Clark R, Nghiem-Rao TH, Spitzer A, Lagatta J. Major anomalies and birth-weight influence NICU interventions and mortality in infants with trisomy 13 or 18. J Perinatol. 2017;37:420–6.
Nelson KE, Rosella LC, Mahant S, Guttmann A. Survival and surgical interventions for children with trisomy 13 and 18. JAMA. 2016;316:420.
Pallotto I, Lantos JD. Treatment decisions for babies with trisomy 13 and 18. HEC Forum. 2017;29:213–22.
Guon J, Wilfond BS, Farlow B, Brazg T, Janvier A. Our children are not a diagnosis: the experience of parents who continue their pregnancy after a prenatal diagnosis of trisomy 13 or 18. Am J Med Genet Part A. 2014;164:308–18.
Leuthner SR, Acharya K. Perinatal counseling following a diagnosis of trisomy 13 or 18: incorporating the facts, parental values, and maintaining choices. Adv Neonatal Care. 2020;20:204–15.
Subramaniam A, Jacobs AP, Tang Y, Neely C, Philips JB, Biggio JR, et al. Trisomy 18: a single-center evaluation of management trends and experience with aggressive obstetric or neonatal intervention. Am J Med Genet. 2016;170:838–46.
Janvier A, Farlow B, Barrington KJ. Parental hopes, interventions, and survival of neonates with trisomy 13 and trisomy 18. Am J Med Genet Part C: Semin Med Genet. 2016;172:279–87.
Winn P, Acharya K, Peterson E, Leuthner S. Prenatal counseling and parental decision-making following a fetal diagnosis of trisomy 13 or 18. J Perinatol. 2018;38:788–96.
Murthy K, Dykes FD, Padula MA, Pallotto EK, Reber KM, Durand DJ, et al. The Children’s Hospitals Neonatal Database: an overview of patient complexity, outcomes and variation in care. J Perinatol. 2014;34:582–6.
Billings KR, Rastatter JC, Lertsburapa K, Schroeder JW Jr. An analysis of common indications for bronchoscopy in neonates and findings over a 10-year period. JAMA Otolaryngol–Head Neck Surg. 2015;141:112–9.
Swanson SK, Schumacher KR, Ohye RG, Zampi JD. Impact of trisomy 13 and 18 on airway anomalies and pulmonary complications after cardiac surgery. J Thorac Cardiovasc Surg. 2020;S0022-5223(20)32473-9.
Fry JT, Matoba N, Datta A, DiGeronimo R, Coghill CH, Natarajan G, et al. Center, gestational age, and race impact end-of-life care practices at regional neonatal intensive care units. J Pediatr. 2020;217:86–91. e1
Graham EM. Infants with trisomy 18 and complex congenital heart defects should not undergo open heart surgery. J Law Med Ethics. 2016;44:286–91.
Acknowledgements
We are indebted to the following institutions that serve the infants and their families, and these institutions also have invested in and continue to participate in the Children’s Hospital’s Neonatal Database (CHND). Jeanette Asselin, Beverly Brozanski, David Durand (ex officio), Francine Dykes (ex officio), Jacquelyn Evans (Executive Director), Theresa Grover, Karna Murthy (Chair), Michael Padula, Eugenia Pallotto, Anthony Piazza, Kristina Reber, and Billie Short are members of the Children’s Hospitals Neonatal Consortium, Inc. For more information, please contact: support@thechnc.org. The site sponsors/contributors for the CHND include:
Palliative Care and Ethics Focus Group of the Children’s Hospital Neonatal Consortium (CHNC)
Anthony Piazza35, Gregory Sysyn36, Carl Coghill37, Ajay Talati38, Anne Hansen39, Tanzeema Houssain39, Karna Murthy40, Gustave Falciglia40, Beth Haberman41, Kristina Reber42, Rashmin Savani43, Theresa Grover44, Girija Natarajan45, Annie Chi46, Yvette Johnson46, Gautham Suresh47, William Engle48, Eugenia Pallotto49, Robert Lyle50, Becky Rogers50, Rachel Chapman51, Jamie Limjoco52, Priscilla Joe53, Jacquelyn Evans54, Michael Padula54, David Munson54, Suzanne Touch55, Beverly Brozanski56, Rakesh Rao57, Amit Mathur57, Victor McKay58, Mark Speziale59, Laurel Moyer59, Billie Short60, Kevin Sullivan61, Con Yee Ling62, Michael Uhing63, Lynne Willett64, Nicole Birge64, Rajan Wadhawan65, Elizabeth Jacobsen-Misbe66, Robert DiGeronimo66, Kyong-Soon Lee67, Michel Mikhael68
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Acharya, K., Leuthner, S.R., Zaniletti, I. et al. Medical and surgical interventions and outcomes for infants with trisomy 18 (T18) or trisomy 13 (T13) at children’s hospitals neonatal intensive care units (NICUs). J Perinatol 41, 1745–1754 (2021). https://doi.org/10.1038/s41372-021-01111-9
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41372-021-01111-9
This article is cited by
-
When external factors limit care options for complex fetal and neonatal diagnoses
Journal of Perinatology (2025)
-
Clinical course and perinatal management of fetuses and newborns affected by trisomy 13 and 18: a retrospective single-centre cohort study
European Journal of Pediatrics (2025)
-
Outcomes of heart surgery in neonates with trisomy 13 and 18: a systematic review with metanalysis
European Journal of Pediatrics (2025)