Abstract
Objective
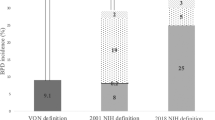
To compare three bronchopulmonary dysplasia (BPD) definitions against hospital outcomes in a referral-based population.
Study design
Data from the Children’s Hospitals Neonatal Consortium were classified by 2018 NICHD, 2019 NRN, and Canadian Neonatal Network (CNN) BPD definitions. Multivariable models evaluated the associations between BPD severity and death, tracheostomy, or length of stay, relative to No BPD references.
Results
Mortality was highest in 2019 NRN Grade 3 infants (aOR 225), followed by 2018 NICHD Grade 3 (aOR 145). Infants with lower BPD grades rarely died (<1%), but Grade 2 infants had aOR 7–21-fold higher for death and 23–56-fold higher for tracheostomy.
Conclusions
Definitions with 3 BPD grades had better discrimination and Grade 3 2019 NRN had the strongest association with outcomes. No/Grade 1 infants rarely had severe outcomes, but Grade 2 infants were at risk. These data may be useful for counseling families and determining therapies for infants with BPD.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Northway WHJ, Rosan RC, Porter DY. Pulmonary disease following respirator therapy of hyaline-membrane disease—bronchopulmonary dysplasia. N Engl J Med. 1967;276:357–68.
Shennan AT, Dunn MS, Ohlsson A, Lennox K, Hoskins EM. Abnormal pulmonary outcomes in premature infants: prediction from oxygen requirement in the neonatal period. Pediatrics. 1988;82:527–32.
Abman SH. Bronchopulmonary dysplasia: “a vascular hypothesis”. Am J Respir Crit Care Med. 2001;164:1755–6.
Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001;163:1723–9.
Poindexter BB, Feng R, Schmidt B, Aschner JL, Ballard RA, Hamvas A, et al. Comparisons and limitations of current definitions of bronchopulmonary dysplasia for the prematurity and respiratory outcomes program. Ann Am Thorac Soc. 2015;12:1822–30.
Ramaswamy VV, More K, Roehr CC, Bandiya P, Nangia S. Efficacy of noninvasive respiratory support modes for primary respiratory support in preterm neonates with respiratory distress syndrome: systematic review and network meta-analysis. Pediatr Pulmonol. 2020. https://doi.org/10.1002/ppul.25011.
Jain D, Bancalari E. New developments in respiratory support for preterm infants. Am J Perinatol. 2019;36:S13–S17.
Fernandez-Alvarez JR, Mahoney L, Gandhi R, Rabe H. Optiflow vs Vapotherm as extended weaning mode from nasal continuous positive airway pressure in preterm infants ≤28 weeks gestational age. Pediatr Pulmonol. 2020. https://doi.org/10.1002/ppul.24936.
Higgins RD, Jobe AH, Koso-Thomas M, Bancalari E, Viscardi RM, Hartert TV, et al. Bronchopulmonary dysplasia: executive summary of a workshop. J Pediatr. 2018;197:300–8.
Jensen EA, Dysart K, Gantz MG, McDonald S, Bamat NA, Keszler M et al. The diagnosis of bronchopulmonary dysplasia in very preterm infants: an evidence-based approach. Am J Respir Crit Care Med. 2019. https://doi.org/10.1164/rccm.201812-2348OC.
Isayama T, Lee SK, Yang J, Lee D, Daspal S, Dunn M, et al. Revisiting the definition of bronchopulmonary dysplasia: effect of changing panoply of respiratory support for preterm neonates. JAMA Pediatr. 2017;171:271–9.
Murthy K, Dykes FD, Padula MA, Pallotto EK, Reber KM, Durand DJ, et al. The Children’s Hospitals Neonatal database: an overview of patient complexity, outcomes and variation in care. J Perinatol. 2014;34:582–6.
Olsen IE, Groveman SA, Lawson ML, Clark RH, Zemel BS. New intrauterine growth curves based on United States data. Pediatrics. 2010;125:e214–24.
McKinney RL, Schmidhoefer JJ, Balasco AL, Machan JT, Hirway P, Keszler M. Severe bronchopulmonary dysplasia: outcomes before and after the implementation of an inpatient multidisciplinary team. J Perinatol. 2020. https://doi.org/10.1038/s41372-020-00863-0.
Abman SH, Collaco JM, Shepherd EG, Keszler M, Cuevas-Guaman M, Welty SE, et al. Interdisciplinary care of children with severe bronchopulmonary dysplasia. J Pediatr. 2017;181:12–28.e1.
Jackson W, Hornik CP, Messina JA, Guglielmo K, Watwe A, Delancy G, et al. In-hospital outcomes of premature infants with severe bronchopulmonary dysplasia. J Perinatol. 2017;37:853–6.
Ekhaguere O, Patel S, Kirpalani H. Nasal intermittent mandatory ventilation versus nasal continuous positive airway pressure before and after invasive ventilatory support. Clin Perinatol. 2019;46:517–36.
Lemyre B, Davis PG, De Paoli AG, Kirpalani H. Nasal intermittent positive pressure ventilation (NIPPV) versus nasal continuous positive airway pressure (NCPAP) for preterm neonates after extubation. Cochrane Database Syst Rev. 2017;2:CD003212.
Cummings JJ, Polin RA. Noninvasive respiratory support. Pediatrics. 2016; 137. https://doi.org/10.1542/peds.2015-3758.
Zhang H, Dysart K, Kendrick DE, Li L, Das A, Hintz SR, et al. Prolonged respiratory support of any type impacts outcomes of extremely low birth weight infants. Pediatr Pulmonol. 2018;53:1447–55.
Dylag AM, Kopin HG, O’Reilly MA, Wang H, Davis SD, Ren CL, et al. Early neonatal oxygen exposure predicts pulmonary morbidity and functional deficits at 1 year. J Pediatr. 2020;223:20–28.e2.
Ha AW, Sudhadevi T, Ebenezer DL, Fu P, Berdyshev EV, Ackerman SJ, et al. Neonatal therapy with PF543, a sphingosine kinase 1 inhibitor, ameliorates hyperoxia-induced airway remodeling in a murine model of bronchopulmonary dysplasia. Am J Physiol Lung Cell Mol Physiol. 2020;319:L497–L512.
Chen S, Wu Q, Zhong D, Li C, Du L. Caffeine prevents hyperoxia-induced lung injury in neonatal mice through NLRP3 inflammasome and NF-κB pathway. Respir Res. 2020;21:140.
Ehrenkranz RA, Walsh MC, Vohr BR, Jobe AH, Wright LL, Fanaroff AA, et al. Validation of the National Institutes of Health consensus definition of bronchopulmonary dysplasia. Pediatrics. 2005;116:1353–60.
Walsh MC, Yao Q, Gettner P, Hale E, Collins M, Hensman A, et al. Impact of a physiologic definition on bronchopulmonary dysplasia rates. Pediatrics. 2004;114:1305–11.
Stoll BJ, Hansen NI, Bell EF, Walsh MC, Carlo WA, Shankaran S, et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993–2012. JAMA. 2015;314:1039–51.
Funding
The Children’s Hospitals Neonatal Consortium (501-c3 organization) supported the statistical analyses presented in this manuscript.
Author information
Authors and Affiliations
Contributions
Author contributions to this manuscript are as follows: study design, data analysis, and preparation of the manuscript (SVR, JML); data analysis and manuscript review (JWL, ACC, JM, KTL, RSR, MM, EW, JWI, RJD, SY, BEH, MAP, NFP, KM, LDN, CHC, RCS, WET, and WAE); Statistical analyses and manuscript review (IZ).
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
De-identified data analyses were approved by the Institutional Review Board of Stanley Manne Research Institute affiliated with the Ann and Robert H. Lurie Children’s Hospital of Chicago. All participating centers obtained regulatory oversight to participate in the CHNC.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Vyas-Read, S., Logan, J.W., Cuna, A.C. et al. A comparison of newer classifications of bronchopulmonary dysplasia: findings from the Children’s Hospitals Neonatal Consortium Severe BPD Group. J Perinatol 42, 58–64 (2022). https://doi.org/10.1038/s41372-021-01178-4
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41372-021-01178-4
This article is cited by
-
Assessing the role of tracheostomy placement in bronchopulmonary dysplasia with pulmonary hypertension
Journal of Perinatology (2024)
-
Finding treasure in the journey: a single center quality improvement bundle to reduce bronchopulmonary dysplasia
Journal of Perinatology (2024)
-
Leveraging transcriptomics to develop bronchopulmonary dysplasia endotypes: a concept paper
Respiratory Research (2023)
-
Hyperinflation and its association with successful transition to home ventilator devices in infants with chronic respiratory failure and severe bronchopulmonary dysplasia
Journal of Perinatology (2023)
-
Artificial intelligence in bronchopulmonary dysplasia- current research and unexplored frontiers
Pediatric Research (2023)