Abstract
Objective
Describe survival and decannulation following infant tracheostomy based on indication for tracheostomy placement.
Study design
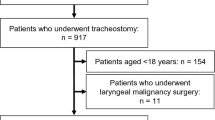
Retrospective cohort study of infants who received tracheostomy at a single pediatric hospital over a twelve-year period. Primary and secondary indications were categorized into pulmonary, anatomic, cardiac, neurologic/musculoskeletal, and others.
Results
A total of 378 infants underwent tracheostomy; 323 had sufficient data to be included in analyses of post-discharge outcomes. Overall mortality was 26.3%; post-operative and post-discharge mortality differed across primary indications (P = 0.03 and P = 0.005). Among survivors, 69.3% decannulated at a median age of 3.0 years (IQR 2.3, 4.5 years). Decannulation among survivors varied across primary indications (P = 0.002), ranging from 17% to 75%. In multivariable analysis, presence of a neurologic or musculoskeletal indication for tracheostomy was a significant negative predictor of future decannulation (aOR 0.10 [95% CI 0.02–0.44], P = 0.003).
Conclusions
Early childhood outcomes vary across indications for infant tracheostomy.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Lewis CW, Carron JD, Perkins JA, Sie KCY, Feudtner C. Tracheotomy in pediatric patients: a national perspective. Arch Otolaryngol - Head Neck Surg. 2003;129:523–9.
Berry JG, Graham RJ, Roberson DW, Rhein L, Graham DA, Zhou J, et al. Patient characteristics associated with in-hospital mortality in children following tracheotomy. Arch Dis Child. 2010;95:703–10.
Tantinikorn W, Alper CM, Bluestone CD, Casselbrant ML. Outcome in pediatric tracheotomy. Am J Otolaryngol - Head Neck Med Surg. 2003;24:131–7.
Overman AE, Liu M, Kurachek SC, Shreve MR, Maynard RC, Mammel MC, et al. Tracheostomy for infants requiring prolonged mechanical ventilation: 10 years’ experience. Pediatrics. 2013;131:e1491–6.
Lee JH, Smith PB, Quek MBH, Laughon MM, Clark RH, Hornik CP. Risk factors and in-hospital outcomes following tracheostomy in infants. J Pediatr. 2016;173:39–44.e1.
Strang AR, Briddell JW, Barth PC, Shah UK, Chidekel A. Risk factor analysis for mortality among infants requiring tracheostomy. Pediatr Pulmonol. 2018;53:1115–21.
Funamura JL, Yuen S, Kawai K, Gergin O, Adil E, Rahbar R, et al. Characterizing mortality in pediatric tracheostomy patients. Laryngoscope. 2017;127:1701–6.
Akangire G, Taylor JB, McAnany S, Noel-MacDonnell J, Lachica C, Sampath V, et al. Respiratory, growth, and survival outcomes of infants with tracheostomy and ventilator dependence. Pediatr Res. 2020.
Wood W, Wang CS, Mitchell RB, Shah GB, Johnson RF. A longitudinal analysis of outcomes in tracheostomy placement among preterm infants. Laryngoscope. 2021;131:417–22.
Ioana Cristea A, Carroll AE, Davis SD, Swigonski NL, Ackerman VL. Outcomes of children with severe bronchopulmonary dysplasia who were ventilator dependent at home. Pediatrics. 2013;132:727.
Edwards JD, Kun SS, Keens TG. Outcomes and causes of death in children on home mechanical ventilation via tracheostomy: an institutional and literature review. J Pediatr. 2010;157:955–9.e2.
Peŕez-Ruiz E, Caro P, Peŕez-Frías J, Cols M, Barrio I, Torrent A, et al. Paediatric patients with a tracheostomy: a multicentre epidemiological study. Eur Respir J. 2012;40:1502–7.
Berry JG, Graham DA, Graham RJ, Zhou J, Putney HL, O’Brien JE, et al. Predictors of clinical outcomes and hospital resource use of children after tracheotomy. Pediatrics. 2009;124:563–72.
Funamura JL, Durbin-Johnson B, Tollefson TT, Harrison J, Senders CW. Pediatric tracheotomy: indications and decannulation outcomes. Laryngoscope. 2014;8:1952–8.
Ogilvie LN, Kozak JK, Chiu S, Adderley RJ, Kozak FK. Changes in pediatric tracheostomy 1982-2011: a Canadian tertiary children’s hospital review. J Pediatr Surg. 2014;49:1549–53.
McPherson ML, Shekerdemian L, Goldsworthy M, Minard CG, Nelson CS, Stein F, et al. A decade of pediatric tracheostomies: indications, outcomes, and long-term prognosis. Pediatr Pulmonol. 2017;52:946–53.
Chia AZH, Ng ZM, Pang YX, Ang AHC, Chow CCT, Teoh OH, et al. Epidemiology of pediatric tracheostomy and risk factors for poor outcomes: an 11-year single-center experience. Otolaryngol - Head Neck Surg (U S). 2020;162:121–8.
Fierro J, Piccione J, Lorch S. Clinical factors influencing time to decannulation in children with tracheostomy and ventilator dependence secondary to bronchopulmonary dysplasia. J Pediatr. 2021;228:31–5.
Demauro SB, D’Agostino JA, Bann C, Bernbaum J, Gerdes M, Bell EF, et al. Developmental outcomes of very preterm infants with tracheostomies. J Pediatr. 2014;164:1303–10.e2.
Naeye RL, Burt LS, Wright DL, Blanc WA, Tatter D. Neonatal mortality, the male disadvantage. Pediatrics. 1971;48:902–6.
Kent AL, Wright IMR, Abdel-Latif ME, Bowen J, Bajuk B, Vincent T. Mortality and adverse neurologic outcomes are greater in preterm male infants. Pediatrics. 2012;129:124–31.
O’Driscoll DN, McGovern M, Greene CM, Molloy EJ. Gender disparities in preterm neonatal outcomes. Acta Paediatr Int J Paediatr 2018;107:1494–9.
Salley J, Kou YF, Shah GB, Mitchell RB, Johnson RF. Survival analysis and decannulation outcomes of infants with tracheotomies. Laryngoscope. 2020;130:2319–24.
Sakai M, Kou YF, Shah GB, Johnson RF. Tracheostomy demographics and outcomes among pediatric patients ages 18 years or younger—United States 2012. Laryngoscope. 2019;129:1706–11.
Cheng J, Lioy J, Sobol S. Effect of tracheostomy timing in premature infants. Int J Pediatr Otorhinolaryngol. 2013;77:1873–6.
De Trey L, Niedermann E, Ghelfi D, Gerber A, Gysin C. Pediatric tracheotomy: a 30-year experience. J Pediatr Surg. 2013;48:1470–5.
Donda K, Agyemang CO, Adjetey NA, Agyekum A, Princewill N, Ayensu M, et al. Tracheostomy trends in preterm infants with bronchopulmonary dysplasia in the United States: 2008–2017. Pediatr Pulmonol. 2021;56:1008–17.
Tsao KJ, Johnson A. Fetal tracheal occlusion for congenital diaphragmatic hernia. Semin Perinatol.2020;44:151164.
Grover TR, Rintoul NE, Hedrick HL. Extracorporeal membrane oxygenation in infants with congenital diaphragmatic hernia. Semin Perinatol.2018;42:96–103.
Krishnan U, Feinstein JA, Adatia I, Austin ED, Mullen MP, Hopper RK, et al. Evaluation and management of pulmonary hypertension in children with bronchopulmonary dysplasia. J Pediatr. 2017;188:24–34.e1.
Seale AN, Daubeney PEF. Pulmonary vein stenosis - novel strategies for a challenging and resistant condition? J Thorac Cardiovasc Surg.2016;151:618–20.
Acknowledgements
We would like to thank Mr. Edward Hopkins for participating in the design of the study. We would also like to thank Mr. Albert Kim for contributing to the collection of data and Drs. Krysten North, Elizabeth Cottrill, Summer Elshenawy, and Bridget Depresico for performing interim analyses of the data.
Author information
Authors and Affiliations
Contributions
LS carried out the initial analyses, drafted the initial paper, and reviewed and revised the paper. JL and SBD conceptualized and designed the study, supervised and coordinated data collection, supervised data analyses, and reviewed and revised the paper. INJ conceptualized and designed the study and reviewed and revised the paper. KM and JS collected data and reviewed and revised the paper. All authors approved the final paper as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics statement
The authors declare no competing interests This study was approved by the Children’s Hospital of Philadelphia Institutional Review Board (IRB) and was granted a waiver of informed consent for retrospective review of existing clinical data. This study was performed in accordance with the Declaration of Helinski.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Sillers, L., Lioy, J., Moran, K. et al. Survival and decannulation across indications for infant tracheostomy: a twelve-year single-center cohort study. J Perinatol 42, 72–78 (2022). https://doi.org/10.1038/s41372-021-01181-9
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41372-021-01181-9
This article is cited by
-
Long-term feeding outcomes after infant tracheostomy
Journal of Perinatology (2025)
-
Risk of death at home or on hospital readmission after discharge with pediatric tracheostomy
Journal of Perinatology (2023)