Abstract
Objective
To assess if infants with neonatal abstinence syndrome (NAS) are smaller at birth and have decreased growth parameters between birth and discharge from the neonatal intensive care unit (NICU).
Methods
Retrospective data analysis of term/late-preterm neonates with NAS at a single-center NICU between September 2006 and May 2018. Growth parameters (weight, length, HC) were measured at birth and discharge. Z scores and percentiles were calculated using WHO standard growth curves.
Results
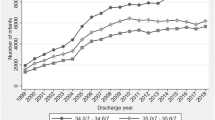
A total of 864 infants ≥35 weeks were admitted for NAS. At birth, median percentiles were weight 30%, HC 23%, and length 37%; these decreased significantly (p < 0.001) at discharge to 12%, 6.5%, and 13%, respectively. The percentage of infants <3rd percentile increased significantly (p < 0.001) in all growth parameters from birth to discharge.
Conclusion
Infants with NAS are smaller at birth and have significant growth retardation in all growth parameters at discharge. An ongoing long-term growth follow-up study will discern the impact of growth restriction in NAS infants.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
O’Donnell M, Nassar N, Leonard H, Hagan R, Mathews R, Patterson Y. et al. Increasing prevalence of neonatal withdrawal syndrome: population study of maternal factors and child protection involvement. Pediatrics. 2009;123:e614–21. https://doi.org/10.1542/peds.2008-2888.
Corr TE, Schaefer EW, Paul IM. Growth during the first year in infants affected by neonatal abstinence syndrome. BMC Pediatr. 2018;18:343. https://doi.org/10.1186/s12887-018-1327-0.
Martinez A, Kastner B, Taeusch HW. Hyperphagia in neonates withdrawing from methadone. Arch Dis Child Fetal Neonatal Ed. 1999;80:F178–82. https://doi.org/10.1136/fn.80.3.f178.
Lee SM, Kim N, Namgung R, Park M, Park K, Jeon J. Prediction of postnatal growth failure among very low birth weight infants. Sci Rep. 2018;8:3729. https://doi.org/10.1038/s41598-018-21647-9.
Towers CV, Hyatt BW, Visconti KC, Chernicky L, Chattin K, Fortner KB. Neonatal head circumference in newborns with neonatal abstinence syndrome. Pediatrics. Jan 2019;143. https://doi.org/10.1542/peds.2018-0541.
Serra AE, Lemon LS, Mokhtari NB, Parks WT, Catov JM, Venkataram R. et al. Delayed villous maturation in term placentas exposed to opioid maintenance therapy: a retrospective cohort study. Am J Obstet Gynecol. 2017;216:418.e1–5. https://doi.org/10.1016/j.ajog.2016.12.016.
Ong KK, Preece MA, Emmett PM, Ahmed ML, Dunger DB, Team AS. Size at birth and early childhood growth in relation to maternal smoking, parity and infant breast-feeding: longitudinal birth cohort study and analysis. Pediatr Res. 2002;52:863–7. https://doi.org/10.1203/00006450-200212000-00009.
Corsi DJ, Hsu H, Fell DB, Wen SW, Walker M. Association of maternal opioid use in pregnancy with adverse perinatal outcomes in Ontario, Canada, from 2012 to 2018. JAMA Netw Open. 2020;3:e208256. https://doi.org/10.1001/jamanetworkopen.2020.8256.
Jones HE, Kaltenbach K, Heil SH, Stine SM, Coyle MG, Arria AM. et al. Neonatal abstinence syndrome after methadone or buprenorphine exposure. N. Engl J Med. 2010;363:2320–31. https://doi.org/10.1056/NEJMoa1005359.
Kraft WK, Adeniyi-Jones SC, Chervoneva I, Greenspan JS, Abatemarco D, Kaltenbach K. et al. Buprenorphine for the treatment of the neonatal abstinence syndrome. N. Engl J Med. 2017;376:2341–8. https://doi.org/10.1056/NEJMoa1614835.
Dryden C, Young D, Campbell N, Mactier H. Postnatal weight loss in substitute methadone-exposed infants: implications for the management of breast feeding. Arch Dis Child Fetal Neonatal Ed. 2012;97:F214–6. https://doi.org/10.1136/adc.2009.178723.
Steward DK, Pridham KF. Nutritional influences on the growth of extremely low birth weight infants. Newborn Infant Nurs Rev. 2002;2:159–65.
Zedler BK, Mann AL, Kim MM, Amick HR, Joyce AR, Murrelle EL. et al. Buprenorphine compared with methadone to treat pregnant women with opioid use disorder: a systematic review and meta-analysis of safety in the mother, fetus and child. Addiction. 2016;111:2115–28. https://doi.org/10.1111/add.13462.
Shipton D, Mactier H, Dryden C, Tappin D. Substitute methadone prescribing in pregnancy is associated with impaired fetal head growth. Arch Dis Child Fetal Neonatal Ed. 2011;96:Fa45.
Hytinantti T, Kahila H, Renlund M, Jarvenpaa AL, Halmesmaki E, Kivitie-Kallio S. Neonatal outcome of 58 infants exposed to maternal buprenorphine in utero. Acta Paediatr. 2008;97:1040–4. https://doi.org/10.1111/j.1651-2227.2008.00838.x.
Karlberg J, Albertsson-Wikland K. Growth in full-term small-for-gestational-age infants: from birth to final height. Pediatr Res. 1995;38:733–9. https://doi.org/10.1203/00006450-199511000-00017.
Hales CN, Barker DJ. Type 2 (non-insulin-dependent) diabetes mellitus: the thrifty phenotype hypothesis. Diabetologia . 1992;35:595–601. https://doi.org/10.1007/BF00400248.
Wisner KL, Bogen DL, Sit D, McShea M, Hughes C, Rizo D. et al. Does fetal exposure to SSRIs or maternal depression impact infant growth?. Am J Psychiatry. 2013;170:485–93. https://doi.org/10.1176/appi.ajp.2012.11121873.
Hart BJ, Viswanathan S, Jadcherla SR. Persistent feeding difficulties among infants with fetal opioid exposure: mechanisms and clinical reasoning. J Matern Fetal Neonatal Med. 2019;32:3633–9. https://doi.org/10.1080/14767058.2018.1469614.
Ben XM. Nutritional management of newborn infants: practical guidelines. World J Gastroenterol. 2008;14:6133–9. https://doi.org/10.3748/wjg.14.6133.
Bogen DL, Hanusa BH, Baker R, Medoff-Cooper B, Cohlan B. Randomized clinical trial of standard- versus high-calorie formula for methadone-exposed infants: a feasibility study. Hosp Pediatr. 2018;8:7–14. https://doi.org/10.1542/hpeds.2017-0114.
Ehrenkranz RA, Dusick AM, Vohr BR, Wright LL, Wrage LA, Poole WK. Growth in the neonatal intensive care unit influences neurodevelopmental and growth outcomes of extremely low birth weight infants. Pediatrics. 2006;117:1253–61. https://doi.org/10.1542/peds.2005-1368.
Takeuchi A, Yorifuji T, Takahashi K, Nakamura M, Kageyama M, Kubo T. et al. Neurodevelopment in full-term small for gestational age infants: a nationwide Japanese population-based study. Brain Dev. 2016;38:529–37. https://doi.org/10.1016/j.braindev.2015.12.013.
Yeoh SL, Eastwood J, Wright IM, Morton R, Melhuish E, Ward M. et al. Cognitive and motor outcomes of children with prenatal opioid exposure: a systematic review and meta-analysis. JAMA Netw Open. 2019;2:e197025. https://doi.org/10.1001/jamanetworkopen.2019.7025.
Grossman MR, Lipshaw MJ, Osborn RR, Berkwitt AK. A novel approach to assessing infants with neonatal abstinence syndrome. Hosp Pediatr. 2018;8:1–6. https://doi.org/10.1542/hpeds.2017-0128.
Patrick SW, Burke JF, Biel TJ, Auger KA, Goyal NK, Cooper WO. Risk of hospital readmission among infants with neonatal abstinence syndrome. Hosp Pediatr. 2015;5:513–9. https://doi.org/10.1542/hpeds.2015-0024.
Author information
Authors and Affiliations
Contributions
MTF conceptualized and designed the study, searched the literature, extracted and analyzed the data, and drafted the initial paper. Ms. JS and DF extracted and analyzed the data, critically reviewed and revised the paper. ML, DC, SA-J, and JG critically reviewed the data analysis, critically reviewed and revised the paper. ZHA conceptualized and designed the study, searched the literature, analyzed the data, critically reviewed and revised the paper. All authors approved the final paper as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Favara, M.T., Smith, J., Friedman, D. et al. Growth failure in infants with neonatal abstinence syndrome in the neonatal intensive care unit. J Perinatol 42, 313–318 (2022). https://doi.org/10.1038/s41372-021-01183-7
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41372-021-01183-7
This article is cited by
-
Outpatient tapering of buprenorphine in opioid use disorder pregnancies may improve neonatal outcomes
Journal of Perinatology (2025)