Abstract
Objective
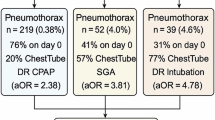
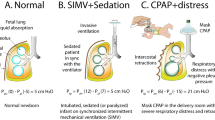
We previously reported an increase in pneumothorax after implementing delivery room (DR) continuous positive airway pressure (CPAP) for labored breathing or persistent cyanosis in ≥35-week gestational age (GA) neonates unexposed to DR-positive pressure ventilation (DR-PPV). We hypothesized that pneumothorax would decrease after de-implementing DR-CPAP in those unexposed to DR-PPV or DR-O2 supplementation (DR-PPV/O2).
Study design
In a retrospective cohort excluding DR-PPV the primary outcome was DR-CPAP-related pneumothorax (1st chest radiogram, 1st day of life). In a subgroup treated by the resuscitation team and admitted to the NICU, the primary outcome was DR-CPAP-associated pneumothorax (1st radiogram, no prior PPV) without DR-PPV/O2.
Results
In the full cohort, occurrence of DR-CPAP-related pneumothorax decreased after the intervention (11.0% vs 6.0%, P < 0.001). In the subgroup, occurrence of DR-CPAP-associated pneumothorax decreased after the intervention (1.4% vs. 0.06%, P < 0.001).
Conclusion
The occurrence of CPAP-associated pneumothorax decreased after avoiding DR-CPAP in ≥35-week GA neonates without DR-PPV/O2.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Gregory GA, Kitterman JA, Phibbs RH, Tooley WH, Hamilton WK. Treatment of the idiopathic respiratory-distress syndrome with continuous positive airway pressure. N. Engl J Med. 1971;284:1333–40.
Avery ME, Tooley WH, Keller JB, Hurd SS, Bryan MH, Cotton RB, et al. Is chronic lung disease in low birth weight infants preventable? A survey of eight centers. Pediatrics 1987;79:26–30.
Hamalek LP, Morley C. Continuous positive airway pressure during neonatal resuscitation. Clin Perinatol. 2006;33:83–98.
Subramaniam P, Ho JJ, Davis PG. Prophylactic nasal continuous positive airway pressure for preventing morbidity and mortality in very preterm infants. Cochrane Database Syst Rev. 2016;6:CD001243.
Morley CJ, Davis PG, Doyle LW, Brion LP, Hascoet JM, Carlin JB. COIN Trial Investigators. Nasal CPAP or intubation at birth for very preterm infants. N. Engl J Med. 2008;358:700–8.
Perlman JM, Wyllie J, Kattwinkel J, Atkins DL, Chameides L, Goldsmith JP, et al. Neonatal resuscitation: 2010 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Pediatrics 2010;126:e1319–e1344.
Kattwinkel J, Perlman JM, Aziz K, Colby C, Fairchild K, Gallagher J, et al. Neonatal Resuscitation: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Pediatrics 2010;126:e1400–e1413.
Tamura M, Wada M, Ishikawa G, Kusakawa I, Goishi K, Sugiura T, et al. JRC Guidelines 2010 English version: NCPR; Neonatal Cardiopulmonary Resuscitation. Secondary JRC Guidelines 2010. https://www.japanresuscitationcouncil.org/wp-content/uploads/2016/02/20121011_NCPR. Accessed 04/06/2021.
Richmond S, Wyllie J. European Resuscitation Council Guidelines for Resuscitation 2010 Section 7. Resuscitation of babies at birth. Resuscitation. 2010;81:1389–99.
Hishikawa K, Goishi K, Fujiwara T, Kaneshige M, Ito Y, Sago H. Pulmonary air leak associated with CPAP at term birth resuscitation. Arch Dis Child Fetal Neonatal Ed. 2015;100:F382–F387.
Smithhart W, Wyckoff MH, Kapadia V, Jaleel M, Kakkilaya V, Brown LS, et al. Delivery room continuous positive airway pressure and pneumothorax. Pediatrics 2019;144:e20190756.
Jaleel MA, Smithhart W, Brion LP. Re: delivery room continuous positive airway pressure and pneumothorax. https://pediatrics.aappublications.org/content/144/3/e20190756/tab-e-letters#re-delivery-room-continuous-positive-airway-pressure-and-pneumothorax, Accessed 10/25/2019.
Clevenger L, Britton JR. Delivery room continuous positive airway pressure and early pneumothorax in term newborn infants. J Neonatal Perinat Med. 2017;10:157–61.
Claessen CC, Strand ML. Understanding the risks and benefits of delivery room CPAP for term infants. Pediatrics 2019;144:e20191720.
Duong HH, Mirea L, Shah PS, Yang J, Lee SK, Sankaran K. Pneumothorax in neonates: trends, predictors and outcomes. J Neonatal Perinat Med. 2014;7:29–38.
Gerhardt T, Bancalari E. Chestwall compliance in full-term and premature infants. Acta Paediatr Scand. 1980;69:359–64.
Poets CF, Rüdiger M. Mask CPAP during neonatal transition: too much of a good thing for some term infants? Arch Dis Child Fetal Neonatal Ed. 2015;100:F378–9.
Spillane NT, Chivily C, Andrews T. Short term outcomes in term and late preterm neonates admitted to the well-baby nursery after resuscitation in the delivery room. J Perinatol. 2019;39:983–9.
Fatemizadah R, Lohmann P, Fernandez CJ. Delivery Room CPAP in Late-Preterm and Term Infants: Jury’s Still Out. Comment, https://pediatrics.aappublications.org/content/144/3/e20190756/tab-e-letters#delivery-room-cpap-in-late-preterm-and-term-infants-jury%E2%80%99s-still-out, Accessed 09/23/2019.
Osman AM, El-Farrash RA, Mohammed EH. Early rescue Neopuff for infants with transient tachypnea of newborn: a randomized controlled trial. J Matern Fetal Neonatal Med. 2019;32:597–603.
Moresco L, Romantsik O, Calevo MG, Bruschettini M. Non-invasive respiratory support for the management of transient tachypnea of the newborn. Cochrane Database Syst Rev. 2020;4:CD013231.
Pandita A, Murki S, Oleti TP, Tandur B, Kiran S, Narkhede S, et al. Effect of nasal continuous positive airway pressure on infants with meconium aspiration syndrome: a randomized clinical trial. JAMA Pediatr. 2018;172:161–5.
Buckmaster AG, Arnolda G, Wright IM, Foster JP, Henderson-Smart DJ. Continuous positive airway pressure therapy for infants with respiratory distress in non tertiary care centers: a randomized, controlled trial [published correction appears in Pediatrics. Pediatrics. 2007;120:509–18.
Manley BJ, Arnolda GRB, Wright IMR, Owen LS, Foster JP, Huang L, et al. HUNTER trial investigators. nasal high-flow therapy for newborn infants in special care nurseries. N Engl J Med. 2019;380:2031–40.
Celebi MY, Alan S, Kahvecioglu D, Cakir U, Yildiz D, Erdeve O, et al. Impact of prophylactic continuous positive airway pressure on transient tachypnea of the newborn and neonatal intensive care admission in newborns delivered by elective cesarean section. Am J Perinatol. 2016;33:99–106.
Kimia AA, Savova G, Landschaft A, Harper MB. An introduction to natural language processing: how you can get more from those electronic notes you are generating. Pediatr Emerg Care. 2015;31:536–41.
Scheid LM, Brown LS, Clark C, Rosenfeld CR. Data electronically extracted from the electronic health record require validation. J Perinatol. 2019;39:468–74.
Penfold RB, Zhang F. Use of interrupted time series analysis in evaluating health care quality improvements. Acad Pediatr. 2013;13:S38–44.
Olsen IE, Groveman SA, Lawson ML, Clark RH, Zemel BS. New intrauterine growth curves based on United States data. Pediatrics 2010;125:e214–224.
Hishikawa K, Fujinaga H, Ito Y. Increased dead space in face mask continuous positive airway pressure in neonates. Pediatr Pulmonol. 2017;52:107–11.
Hishikawa K, Fujinaga H, Fujiwara T, Goishi K, Kaneshige M, Sago H, et al. Respiratory stabilization after delivery in term infants after the update of the Japan resuscitation council guidelines in 2010. Neonatology 2016;110:1–7.
LeVan JM, Wyckoff MH, Ahn C, Heyne R, Sánchez PJ, Chalak L, et al. Change in care among nonenrolled patients during and after a randomized trial. Pediatrics 2013;132:e960–970.
LeVan JM, Brion LP, Wrage LA, Gantz MG, Wyckoff MH, Sánchez PJ, et al. Eunice Kennedy shriver NICHD neonatal research network. change in practice after the surfactant, positive pressure and oxygenation randomised trial. Arch Dis Child Fetal Neonatal Ed. 2014;99:F386–90.
Goldman RD. Spontaneous pneumothorax in children. Can Fam Physician. 2020;66:737–8.
Chiruvolu A, Claunch KM, Garcia AJ, Petrey B, Hammonds K, Mallett LH. Effect of continuous positive airway pressure versus nasal cannula on late preterm and term infants with transient tachypnea of the newborn. J Perinatol. 2021;41:1675–80.
Author information
Authors and Affiliations
Contributions
Dr. Stocks drafted the initial manuscript and collected data. Drs Smithhart, Wyckoff, Jaleel, Kapadia, Kakkilaya and Nelson conceptualized and designed the study. Dr. Brenan planned methods of analysis. Dr. Mangona reviewed the chest radiograms of neonates with questionable pneumothorax; she was blinded to delivery room therapy. Ms. Burchfield and Ms. Thomas collected dated. Brion conceptualized and designed the project, collected, and analyzed the data. Mr. Clark worked at optimizing algorithms to extract data on pneumothorax (with Dr. Stocks) as well as DR-CPAP, DR-PPV and DR-O2 (with Dr. Brenan) from the electronic medical record system and extracted data for the full cohort. Mr. Brown analyzed the data using statistical tools. All authors participated in the interpretation of the data, critically reviewed the revisions, approved the final manuscript as submitted and agree to be accountable for all aspects of the work. Preliminary results were published as a comment in Pediatrics17 and as an abstract to the Annual Meeting of the Pediatric Academy Societies: Stocks E, Jaleel M, Smitthart W, Burchfield P, Thomas A, Mangona, KLM, Kapadia V, Wyckoff MH, Kakkilaya V, Weaver J, Brion LP. Reduction in Delivery Room (DR) Continuous Positive Airway Pressure (CPAP)-Associated Pneumothorax in Term and Late-Preterm Neonates. Accepted for oral presentation at PAS, Philadelphia, PA, 5/2/2020; cancelled for COVID-19/SARS-Cov-2; presented online at Virtual Regional Neonatal Research Conference 6/16/2020. The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This project was initially approved as quality improvement by the University of Texas Southwestern Medical Center Institutional Review Board and by Parkland Health and Hospital Systems. The entire project including the retrospective full cohort as described was later approved as a research project. The need for informed consent was waived for the entire project.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Stocks, E.F., Jaleel, M., Smithhart, W. et al. Decreasing delivery room CPAP-associated pneumothorax at ≥35-week gestational age. J Perinatol 42, 761–768 (2022). https://doi.org/10.1038/s41372-022-01334-4
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41372-022-01334-4
This article is cited by
-
A validated NICU database: recounting 50 years of clinical growth, quality improvement and research
Pediatric Research (2025)
-
Pneumothorax in a term newborn
Journal of Perinatology (2024)
-
Respiratory Disorders in Neonates Born by Elective Cesarean Section
Current Treatment Options in Pediatrics (2023)