Abstract
Objective
To determine the association between prenatal ultrasound (US) and magnetic resonance imaging (MRI) characteristics in right congenital diaphragmatic hernia (RCDH) with postnatal outcome.
Study design
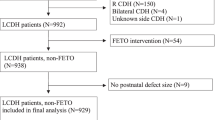
CDH Study Group data were reviewed for all RCDH infants (n = 156) born between 2015 and 2019. Prenatal US and MRI lung size measurements were correlated with survival, extracorporeal life support (ECLS), and defect size.
Result
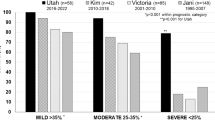
Overall survival was 64.1%. ECLS was required in 40.4%. US and MRI-based prenatal assessment of pulmonary hypoplasia does not predict survival. Prenatal measurement of lung size using either US or MRI correlates with ECLS use. Only MRI-based measures of lung size are associated with defect size.
Conclusion
Image-based prenatal predictors of survival, ECLS, and defect size are of limited value in RCDH. Extrapolation of prenatal survival and morbidity indicators from left to right-sided CDH is not appropriate. There is an urgent need to develop RCDH prenatal prediction models.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The data that supports the findings of this study are available from the corresponding author upon reasonable request.
References
Lally KP. Congenital diaphragmatic hernia. Curr Opin Pediatr. 2002;14:486–90.
Moreno-Alvarez O, Cruz-Martinez R, Hernandez-Andrade E, Done E, Gomez O, Deprest J, et al. Lung tissue perfusion in congenital diaphragmatic hernia and association with the lung-to-head ratio and intrapulmonary artery pulsed Doppler. Ultrasound Obstet Gynecol. 2010;35:578–82.
Clark RH, Hardin WD Jr, Hirschl RB, Jaksic T, Lally KP, Langham MR Jr, et al. Current surgical management of congenital diaphragmatic hernia: a report from the Congenital Diaphragmatic Hernia Study Group. J Pediatr Surg. 1998;33:1004–9.
Partridge EA, Peranteau WH, Herkert L, Rendon N, Smith H, Rintoul NE, et al. Right- versus left-sided congenital diaphragmatic hernia: a comparative outcomes analysis. J Pediatr Surg. 2016;51:900–2.
Burgos CM, Frenckner B, Luco M, Harting MT, Lally PA, Lally KP, et al. Right versus left congenital diaphragmatic hernia—What’s the difference? J Pediatr Surg. 2017;S0022-3468:30649–8. https://doi.org/10.1016/j.jpedsurg.2017.10.027. Online ahead of print.
Skari H, Bjornland K, Haugen G, Egeland T, Emblem R. Congenital diaphragmatic hernia: a meta-analysis of mortality factors. J Pediatr Surg. 2000;35:1187–97.
Skari H, Bjornland K, Frenckner B, Friberg LG, Heikkinen M, Hurme T, et al. Congenital diaphragmatic hernia in Scandinavia from 1995 to 1998: Predictors of mortality. J Pediatr Surg. 2002;37:1269–75.
Fisher JC, Jefferson RA, Arkovitz MS, Stolar CJ. Redefining outcomes in right congenital diaphragmatic hernia. J Pediatr Surg. 2008;43:373–9.
Midrio P, Gobbi D, Baldo V, Gamba P. Right congenital diaphragmatic hernia: an 18-year experience. J Pediatr Surg. 2007;42:517–21.
Mesas Burgos C, Hammarqvist-Vejde J, Frenckner B, Conner P. Differences in outcomes in prenatally diagnosed congenital diaphragmatic hernia compared to postnatal detection: a single-center experience. Fetal Diagn Ther. 2016;39:241–7.
Slavotinek AM, Warmerdam B, Lin AE, Shaw GM. Population-based analysis of left- and right-sided diaphragmatic hernias demonstrates different frequencies of selected additional anomalies. Am J Med Genet A. 2007;143A:3127–36.
Schaible T, Kohl T, Reinshagen K, Brade J, Neff KW, Stressig R, et al. Right- versus left-sided congenital diaphragmatic hernia: postnatal outcome at a specialized tertiary care center. Pediatr Crit Care Med. 2012;13:66–71.
Duess JW, Zani-Ruttenstock EM, Garriboli M, Puri P, Pierro A, Hoellwarth ME. Outcome of right-sided diaphragmatic hernia repair: a multicentre study. Pediatr Surg Int. 2015;31:465–71.
Hedrick HL, Danzer E, Merchant AM, Bebbington MW, Zhao H, Flake AW, et al. Liver position and lung-to-head ratio for prediction of extracorporeal membrane oxygenation and survival in isolated left congenital diaphragmatic hernia. Am J Obstet Gynecol. 2007;197:422 e421–4.
Metkus AP, Filly RA, Stringer MD, Harrison MR, Adzick NS. Sonographic predictors of survival in fetal diaphragmatic hernia. J Pediatr Surg. 1996;31:148–51. discussion 151-142.
Jani J, Nicolaides KH, Keller RL, Benachi A, Peralta CF, Favre R, et al. Observed to expected lung area to head circumference ratio in the prediction of survival in fetuses with isolated diaphragmatic hernia. Ultrasound Obstet Gynecol. 2007;30:67–71.
Bebbington M, Victoria T, Danzer E, Moldenhauer J, Khalek N, Johnson M, et al. Comparison of ultrasound and magnetic resonance imaging parameters in predicting survival in isolated left-sided congenital diaphragmatic hernia. Ultrasound Obstet Gynecol. 2014;43:670–4.
Madenci AL, Sjogren AR, Treadwell MC, Ladino-Torres MF, Drongowski RA, Kreutzman J, et al. Another dimension to survival: predicting outcomes with fetal MRI versus prenatal ultrasound in patients with congenital diaphragmatic hernia. J Pediatr Surg. 2013;48:1190–7.
Russo FM, Eastwood MP, Keijzer R, Al-Maary J, Toelen J, Van Mieghem T, et al. Lung size and liver herniation predict need for extracorporeal membrane oxygenation but not pulmonary hypertension in isolated congenital diaphragmatic hernia: systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2017;49:704–13.
DeKoninck P, Gomez O, Sandaite I, Richter J, Nawapun K, Eerdekens A, et al. Right-sided congenital diaphragmatic hernia in a decade of fetal surgery. BJOG. 2015;122:940–6.
Victoria T, Danzer E, Oliver ER, Edgar JC, Iyoob S, Partridge EA, et al. Right congenital diaphragmatic hernias: is there a correlation between prenatal lung volume and postnatal survival, as in isolated left diaphragmatic hernias? Fetal Diagn Ther. 2018;43:12–8.
Berdan EA, Saltzman DA. Right- versus left-sided congenital diaphragmatic hernia-can we trust the data? Pediatr Crit Care Med. 2012;13:103–4.
Hedrick HL, Crombleholme TM, Flake AW, Nance ML, von Allmen D, Howell LJ, et al. Right congenital diaphragmatic hernia: Prenatal assessment and outcome. J Pediatr Surg. 2004;39:319–23. discussion 319-23.
Harting MT, Lally KP. The Congenital Diaphragmatic Hernia Study Group registry update. Semin Fetal Neonatal Med. 2014;19:370–5.
Lally KP, Lasky RE, Lally PA, Bagolan P, Davis CF, Frenckner BP, et al. Standardized reporting for congenital diaphragmatic hernia-an international consensus. J Pediatr Surg. 2013;48:2408–15.
Peralta CF, Cavoretto P, Csapo B, Vandecruys H, Nicolaides KH. Assessment of lung area in normal fetuses at 12–32 weeks. Ultrasound Obstet Gynecol. 2005;26:718–24.
Rypens F, Metens T, Rocourt N, Sonigo P, Brunelle F, Quere MP, et al. Fetal lung volume: estimation at MR imaging-initial results. Radiology. 2001;219:236–41.
Shieh HF, Barnewolt CE, Wilson JM, Zurakowski D, Connolly SA, Estroff JA, et al. Percent predicted lung volume changes on fetal magnetic resonance imaging throughout gestation in congenital diaphragmatic hernia. J Pediatr Surg. 2017;52:933–7.
Oluyomi-Obi T, Kuret V, Puligandla P, Lodha A, Lee-Robertson H, Lee K, et al. Antenatal predictors of outcome in prenatally diagnosed congenital diaphragmatic hernia (CDH). J Pediatr Surg. 2017;52:881–8.
Ferguson DM. Congenital Diaphragmatic Hernia Study G. Hepatopulmonary fusion: A rare variant of congenital diaphragmatic hernia. J Pediatr Surg. 2020;55:1903–7.
Kilian AK, Schaible T, Hofmann V, Brade J, Neff KW, Busing KA. Congenital diaphragmatic hernia: predictive value of MRI relative lung-to-head ratio compared with MRI fetal lung volume and sonographic lung-to-head ratio. AJR Am J Roentgenol. 2009;192:153–8.
Kastenholz KE, Weis M, Hagelstein C, Weiss C, Kehl S, Schaible T, et al. Correlation of observed-to-expected MRI fetal lung volume and ultrasound lung-to-head ratio at different gestational times in fetuses with congenital diaphragmatic hernia. AJR Am J Roentgenol. 2016;206:856–66.
Russo FM, Cordier AG, Basurto D, Salazar L, Litwinska E, Gomez O, et al. Fetal endoscopic tracheal occlusion reverses the natural history of right-sided congenital diaphragmatic hernia: European multicenter experience. Ultrasound Obstet Gynecol. 2021;57:378–85.
Jancelewicz T, Langham MR, Jr., Brindle ME, Stiles ZE, Lally PA, Dong L, et al. Survival benefit associated with the use of extracorporeal life support for neonates with congenital diaphragmatic hernia. Ann Surg. 2022;275:e256–63.
Pinton A, Boubnova J, Becmeur F, Kuhn P, Senat MV, Stirnemann J, et al. Is laterality of congenital diaphragmatic hernia a reliable prognostic factor? French national cohort study. Prenat Diagn. 2020;40:949–57.
Chock VY, Danzer E, Chung S, Noh CY, Ebanks AH, Harting MT, et al. In-hospital morbidities for neonates with congenital diaphragmatic hernia: the impact of defect size and laterality. J Pediatr. 2022;240:94–101.e6.
Perrone EE, Abbasi N, Cortes MS, Umar U, Ryan G, Johnson A, et al. Prenatal assessment of congenital diaphragmatic hernia at north american fetal therapy network centers: A continued plea for standardization. Prenat Diagn. 2021;41:200–6.
Abbasi N, Cortes MS, Ruano R, Johnson A, Morgan T, Coleman B, et al. Variability in antenatal prognostication of fetal diaphragmatic hernia across the North American Fetal Therapy Network (NAFTNet). Prenat Diagn. 2020;40:342–50.
Acknowledgements
The authors have no conflicts of interest to disclose. This information has not been presented, is not published elsewhere, and is not under any simultaneous consideration.
Author information
Authors and Affiliations
Consortia
Contributions
Study conception and design: ED, MTH, KPL, EEP, KPVM; Data acquisition: PAL, AHE; Analysis and data interpretation: ED, SC, VYC, CYN, KPVM; Drafting of the manuscript: ED, VYC, SC, KPVM; Critical revision: ED, VYC, SC, CYN, PAL, MTH, KPL, EEP, AHE, KPVM.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Danzer, E., Chock, V.Y., Chung, S. et al. Image-based prenatal predictors of postnatal survival, extracorporeal life support, and defect size in right congenital diaphragmatic hernia. J Perinatol 42, 1202–1209 (2022). https://doi.org/10.1038/s41372-022-01470-x
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41372-022-01470-x
This article is cited by
-
Comparison of current to past outcomes in congenital diaphragmatic hernia using MRI observed-to-expected total fetal lung volume
Journal of Perinatology (2024)
-
Prenatal MRI assessment of mediastinal shift angle as a feasible and effective risk stratification tool in isolated right-sided congenital diaphragmatic hernia
European Radiology (2023)