Abstract
Objective
To develop machine learning models predicting extubation failure in low birthweight neonates using large amounts of clinical data.
Study design
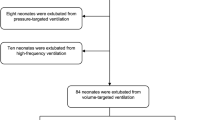
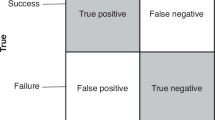
Retrospective cohort study using MIMIC-III, a large single-center, open-source clinical dataset. Logistic regression and boosted-tree (XGBoost) models using demographics, medications, and vital sign and ventilatory data were developed to predict extubation failure, defined as reintubation within 7 days.
Results
1348 low birthweight (≤2500 g) neonates who received mechanical ventilation within the first 7 days were included, of which 350 (26%) failed a trial of extubation. The best-performing model was a boosted-tree model incorporating demographics, vital signs, ventilator parameters, and medications (AUROC 0.82). The most important features were birthweight, last FiO2, average mean airway pressure, caffeine use, and gestational age.
Conclusions
Machine learning models identified low birthweight ventilated neonates at risk for extubation failure. These models will need to be validated across multiple centers to determine generalizability of this tool.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The datasets described in the manuscript are publicly accessible (https://physionet.org/content/mimiciii/1.4/). The models described are available upon request to the corresponding author.
References
Stoll BJ, Hansen NI, Bell EF, Shankaran S, Laptook AR, Walsh MC, et al. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics. 2010;126:443–56.
Consortium on Safe Labor, Hibbard JU, Wilkins I, Sun L, Gregory K, Haberman S, et al. Respiratory morbidity in late preterm births. JAMA. 2010;304:419–25.
Chavez TA, Lakshmanan A, Figueroa L, Iyer N, Stavroudis TA, Garingo A, et al. Resource utilization patterns using non-invasive ventilation in neonates with respiratory distress syndrome. J Perinatol. 2018;38:850–6.
Berger J, Mehta P, Bucholz E, Dziura J, Bhandari V. Impact of early extubation and reintubation on the incidence of bronchopulmonary dysplasia in neonates. Am J Perinatol. 2014;31:1063–72.
Williams E, Dassios T, Arnold K, Hickey A, Greenough A. Prolonged ventilation and postnatal growth of preterm infants. J Perinat Med. 2019;48:82–6.
Robbins M, Trittmann J, Martin E, Reber KM, Nelin L, Shepherd E. Early extubation attempts reduce length of stay in extremely preterm infants even if re-intubation is necessary. J Neonatal Perinat Med. 2015;8:91–7.
Vliegenthart RJS, van Kaam AH, Aarnoudse-Moens CSH, van Wassenaer AG, Onland W. Duration of mechanical ventilation and neurodevelopment in preterm infants. Arch Dis Child Fetal Neonatal Ed. 2019;104:F631–5.
Jensen EA, DeMauro SB, Kornhauser M, Aghai ZH, Greenspan JS, Dysart KC. Effects of multiple ventilation courses and duration of mechanical ventilation on respiratory outcomes in extremely low-birth-weight infants. JAMA Pediatr. 2015;169:1011–7.
Chawla S, Natarajan G, Shankaran S, Carper B, Brion LP, Keszler M, et al. Markers of successful extubation in extremely preterm infants, and morbidity after failed extubation. J Pediatr. 2017;189:113–9.e2.
Shalish W, Kanbar L, Kovacs L, Chawla S, Keszler M, Rao S, et al. The impact of time interval between extubation and reintubation on death or bronchopulmonary dysplasia in extremely preterm infants. J Pediatr. 2019;205:70–76.e2.
Shalish W, Latremouille S, Papenburg J, Sant’Anna GM. Predictors of extubation readiness in preterm infants: a systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed. 2019;104:F89–97.
Dimitriou G, Greenough A, Endo A, Cherian S, Rafferty G. Prediction of extubation failure in preterm infants. Arch Dis Child Fetal Neonatal Ed. 2002;86:F32–5.
Szymankiewicz M, Vidyasagar D, Gadzinowski J. Predictors of successful extubation of preterm low-birth-weight infants with respiratory distress syndrome. Pediatr Crit Care Med. 2005;6:44–9.
Gupta D, Greenberg RG, Sharma A, Natarajan G, Cotten M, Thomas R, et al. A predictive model for extubation readiness in extremely preterm infants. J Perinatol. 2019;39:1663–9.
Silva MGF, Gregório ML, de Godoy MF. Does heart rate variability improve prediction of failed extubation in preterm infants? J Perinat Med. 2019;47:252–7.
Precup D, Robles-Rubio CA, Brown KA, Kanbar L, Kaczmarek J, Chawla S, et al. Prediction of extubation readiness in extreme preterm infants based on measures of cardiorespiratory variability. Conf Proc IEEE Eng Med Biol Soc. 2012;2012:5630–3.
Kaczmarek J, Chawla S, Marchica C, Dwaihy M, Grundy L, Sant’Anna GM. Heart rate variability and extubation readiness in extremely preterm infants. Neonatology. 2013;104:42–8.
Beam AL, Kohane IS. Big data and machine learning in health care. JAMA. 2018;319:1317–8.
Shalish W, Kanbar LJ, Rao S, Robles-Rubio CA, Kovacs L, Chawla S, et al. Prediction of Extubation readiness in extremely preterm infants by the automated analysis of cardiorespiratory behavior: study protocol. BMC Pediatr. 2017;17:167.
Mueller M, Almeida JS, Stanislaus R, Wagner CL. Can machine learning methods predict extubation outcome in premature infants as well as clinicians? J Neonatal Biol. 2013;2. https://doi.org/10.4172/2167-0897.1000118.
Daunhawer I, Kasser S, Koch G, Sieber L, Cakal H, Tütsch J, et al. Enhanced early prediction of clinically relevant neonatal hyperbilirubinemia with machine learning. Pediatr Res. 2019;86:122–7.
Turova V, Sidorenko I, Eckardt L, Rieger-Fackeldey E, Felderhoff-Müser U, Alves-Pinto A, et al. Machine learning models for identifying preterm infants at risk of cerebral hemorrhage. PLoS ONE. 2020;15:e0227419.
Podda M, Bacciu D, Micheli A, Bellù R, Placidi G, Gagliardi L. A machine learning approach to estimating preterm infants survival: development of the Preterm Infants Survival Assessment (PISA) predictor. Sci Rep. 2018;8:13743.
Mikhno A, Ennett CM. Prediction of extubation failure for neonates with respiratory distress syndrome using the MIMIC-II clinical database. Conf Proc IEEE Eng Med Biol Soc. 2012;2012:5094–7.
Collins GS, Reitsma JB, Altman DG, Moons KGM. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD). Circulation. 2015;131:211–9.
Johnson A, Pollard T, Mark R. MIMIC-III Clinical Database (version 1.4). PhysioNet. 2016. Available from: https://doi.org/10.13026/C2XW26.
Johnson AEW, Pollard TJ, Shen L, Lehman LH, Feng M, Ghassemi M, et al. MIMIC-III, a freely accessible critical care database. Sci Data. 2016;3:160035.
Goldberger AL, Amaral LA, Glass L, Hausdorff JM, Ivanov PC, Mark RG, et al. PhysioBank, PhysioToolkit, and PhysioNet: components of a new research resource for complex physiologic signals. Circulation. 2000;101:E215–20.
Giaccone A, Jensen E, Davis P, Schmidt B. Definitions of extubation success in very premature infants: a systematic review. Arch Dis Child Fetal Neonatal Ed. 2014;99:F124–7.
Chen T, Guestrin C. XGBoost: a scalable tree boosting system. In: Proceedings of the 22nd ACM SIGKDD International Conference on Knowledge Discovery and Data Mining. New York, NY, USA: Association for Computing Machinery; 2016. p. 785–94.
Lundberg SM, Erion G, Chen H, DeGrave A, Prutkin JM, Nair B, et al. From local explanations to global understanding with explainable AI for trees. Nat Mach Intell. 2020;2:56–67.
Keller RL, Feng R, DeMauro SB, Ferkol T, Hardie W, Rogers EE, et al. Bronchopulmonary dysplasia and perinatal characteristics predict 1-year respiratory outcomes in newborns born at extremely low gestational age: a prospective cohort study. J Pediatr. 2017;187:89–97.e3.
Lodha A, Seshia M, McMillan DD, Barrington K, Yang J, Lee SK, et al. Association of early caffeine administration and neonatal outcomes in very preterm neonates. JAMA Pediatr. 2015;169:33–8.
Acknowledgements
The authors would like to thank the 2019 course directors of HST 953 Collaborative Data Science in Medicine at the Massachusetts Institute of Technology for their guidance and support in working with the MIMIC-III database.
Funding
ALB is funded by the NIH NHBLI (K01HL141771).
Author information
Authors and Affiliations
Contributions
AN designed the study, performed initial and subsequent analyses, and drafted the initial manuscript. JCL conceptualized and designed the study, provided supervision, participated in the initial and subsequent analyses, interpreted the data, and drafted the initial manuscript. KSB conceptualized and designed the study, participated in the initial and subsequent analyses, interpreted the data, and revised the manuscript. ALB conceptualized and designed the study, provided supervision, participated in the initial and subsequent analyses, and revised the manuscript. GL and JL participated in the initial analyses and revised the manuscript. All authors gave final approval to be published and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Natarajan, A., Lam, G., Liu, J. et al. Prediction of extubation failure among low birthweight neonates using machine learning. J Perinatol 43, 209–214 (2023). https://doi.org/10.1038/s41372-022-01591-3
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41372-022-01591-3
This article is cited by
-
Association between the respiratory severity score and extubation success in severe bronchopulmonary dysplasia
Journal of Perinatology (2026)
-
Validation of a novel Bayesian predictive algorithm for detection of carbon dioxide retention using retrospective neonatal ICU data
Journal of Perinatology (2026)