Abstract
Objective
Determine short-term outcomes following peritoneal drain (PD), laparotomy (LAP) after PD (PD-LAP), and LAP in extremely low birth weight (ELBW) infants with spontaneous intestinal perforation (SIP).
Study design
ELBW infants with SIP were identified using the Children’s Hospitals Neonatal Database. Mortality and length of stay (LOS) were compared among groups.
Results
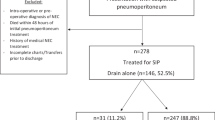
Of 729 SIP infants from 6/2010-12/2016, 383(53%) received PD, 61(8%) PD-LAP, and 285(39%) LAP. PD infants had lower GA at birth, at SIP diagnosis and upon admission than PD-LAP or LAP; and higher sepsis rates than LAP. Bivariate analysis and Kaplan-Meier survival estimates suggested PD had increased mortality vs. PD-LAP and LAP (27%, 11.5%, and 15.8% respectively, p < 0.001). However, surgical approach was not significantly associated with mortality in multivariable analysis accounting for GA and illness severity. LOS did not differ by surgical approach.
Conclusions
In ELBW infants with SIP, mortality, and LOS are independent of the initial surgical approach.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
All data relevant to the study is included in the article. Requests for additional material can be made to Amy Hair at abhair@bcm.edu.
References
Elgendy MM, Othman HF, Heis F, Qattea I, Aly H. Spontaneous intestinal perforation in premature infants: a national study. J Perinatol. 2021;41:1122–8.
Hwang H, Murphy JJ, Gow KW, Magee JF, Bekhit E, Jamieson D. Are localized intestinal perforations distinct from necrotizing enterocolitis? J Pediatr Surg. 2003;38:763–7.
Neu J, Walker WA. Necrotizing enterocolitis. N. Engl J Med. 2011;364:255–64.
Gollin G, Abarbanell A, Baerg JE. Peritoneal drainage as definitive management of intestinal perforation in extremely low-birth-weight infants. J Pediatr Surg. 2003;38:1814–7.
Quiroz HJ, Rao K, Brady AC, Hogan AR, Thorson CM, Perez EA, et al. Protocol-driven surgical care of Necrotizing Enterocolitis and spontaneous intestinal perforation. J Surg Res. 2020;255:396–404.
Lure AC, Du X, Black EW, Irons R, Lemas DJ, Taylor JA, et al. Using machine learning analysis to assist in differentiating between necrotizing enterocolitis and spontaneous intestinal perforation: A novel predictive analytic tool. J Pediatr Surg. 2021;56:1703–10.
Dübbers M, Holtkamp G, Cernaianu G, Bludau M, Fischer J, Keller T, et al. Primary anastomosis as a valid alternative for extremely low birth weight infants with spontaneous intestinal perforation. Eur J Pediatr. 2021;180:1529–35.
Blakely ML, Tyson JE, Lally KP, Hintz SR, Eggleston B, Stevenson DK, et al. Initial Laparotomy versus Peritoneal drainage in extremely low birthweight infants with surgical necrotizing enterocolitis or isolated intestinal perforation: a multicenter randomized clinical trial. Ann Surg. 2021;274:e370–e80.
Fatemizadeh R, Mandal S, Gollins L, Shah S, Premkumar M, Hair A. Incidence of spontaneous intestinal perforations exceeds necrotizing enterocolitis in extremely low birth weight infants fed an exclusive human milk-based diet: A single center experience. J Pediatr Surg. 2021;56:1051–6.
Wadhawan R, Oh W, Hintz SR, Blakely ML, Das A, Bell EF, et al. Neurodevelopmental outcomes of extremely low birth weight infants with spontaneous intestinal perforation or surgical necrotizing enterocolitis. J Perinatol. 2014;34:64–70.
Shah TA, Meinzen-Derr J, Gratton T, Steichen J, Donovan EF, Yolton K, et al. Hospital and neurodevelopmental outcomes of extremely low-birth-weight infants with necrotizing enterocolitis and spontaneous intestinal perforation. J Perinatol. 2012;32:552–8.
Zozaya C, Shah J, Pierro A, Zani A, Synnes A, Lee S, et al. Neurodevelopmental and growth outcomes of extremely preterm infants with necrotizing enterocolitis or spontaneous intestinal perforation. J Pediatr Surg. 2021;56:309–16.
Shah J, Singhal N, da Silva O, Rouvinez-Bouali N, Seshia M, Lee SK, et al. Intestinal perforation in very preterm neonates: risk factors and outcomes. J Perinatol. 2015;35:595–600.
Murthy K, Yanowitz TD, DiGeronimo R, Dykes FD, Zaniletti I, Sharma J, et al. Short-term outcomes for preterm infants with surgical necrotizing enterocolitis. J Perinatol. 2014;34:736–40.
Olsen IE, Groveman SA, Lawson ML, Clark RH, Zemel BS. New intrauterine growth curves based on United States data. Pediatrics. 2010;125:e214–24.
Culbreath K, Keefe G, Edwards EM, Morrow KA, Soll RF, Jaksic T, et al. Morbidity associated with laparotomy-confirmed spontaneous intestinal perforation: A prospective multicenter analysis. J Pediatr Surg. 2022;57:981–5.
Sampah MES, Hackam DJ. Prenatal immunity and influences on Necrotizing Enterocolitis and associated neonatal disorders. Front Immunol. 2021;12:650709.
Ehrenkranz RA, Dusick AM, Vohr BR, Wright LL, Wrage LA, Poole WK. Growth in the neonatal intensive care unit influences neurodevelopmental and growth outcomes of extremely low birth weight infants. Pediatrics. 2006;117:1253–61.
Tappenden KA. Intestinal adaptation following resection. JPEN J Parenter Enter Nutr. 2014;38:23S–31S.
Gosselin KB, Duggan C. Enteral nutrition in the management of pediatric intestinal failure. J Pediatr. 2014;165:1085–90.
Section on Breastfeeding. Breastfeeding and the use of human milk. Pediatrics. 2012;129:e827–41.
Acknowledgements
Data for use in this study were supplied by Children’s Hospitals Neonatal Consortium, Inc. (CHNC). Any analysis, interpretation, or conclusion based on these data is solely that of the authors, and CHNC specifically disclaims responsibility for any such analysis, interpretation, or conclusion. We’d like to acknowledge additional members of the CHND Surgical NEC Focus Group, not otherwise listed as a contributing author, who participated in part in this project, including Michael Padula, Allison Rose, Lynn Fuchs, Carla Snider, Kera McNelis, Hala Chaaban, Hannah Hightower, Bonny Jasani and Catherine Hunter. We’d also like to thank the CHNC leadership and executive committee without whom this work would not have been possible: Jeanette Asselin (ex officio), David Durand (ex officio), Francine Dykes (ex officio), Karna Murthy (Chair), Michael Padula, Eugenia Pallotto, Theresa Grover, Beverly Brozanski, and Anthony Piazza, Kristina Reber, Joanne Lagatta, Joan Smith, Lamia Soghier, Billie Short, and Jacquelyn Evans are members of the Children’s Hospitals Neonatal Consortium, Inc. For more information, please contact: support@thechnc.org. Finally, we are indebted to the following institutions that serve infants and their families, and these institutions also have invested in and continue to participate in the Children’s Hospital’s Neonatal Database (CHND). The site sponsors/contributors for the CHND are also included: 1. Children’s Healthcare of Atlanta Egleston, Atlanta, GA (Anthony Piazza). 2. Children’s Healthcare of Atlanta at Scottish Rite, Atlanta, GA (Gregory Sysyn). 3. Dell Children’s Hospital, Austin, TX (Ashley Lucke, Molly Pont). 4. Children’s Hospital of Alabama, Birmingham, AL (Carl Coghill, Allison Black). 5. Children’s Hospital Boston, Boston, MA (Anne Hansen). 6. Levine Children’s Hospital, Charlotte, NC (Eugenia Pallotto). 7. Ann and Robert H. Lurie Children’s Hospital of Chicago, Chicago, IL (Gustave Falciglia). 8. Cincinnati Children’s Hospital, Cincinnati, OH (Beth Haberman). 9. Cleveland Clinic Children’s Hospital, Cleveland, OH (Hany Aly, Tetyana Nesterenko). 10. Nationwide Children’s Hospital, Columbus, OH (Thomas Bartman). 11. Children’s Health Center, Dallas, TX (Lina Chalak, Sushmita Yallapragada). 12. Children’s Hospital Colorado, Denver, CO (Danielle Smith, Stephanie Bourque). 13. Children’s Hospital of Michigan, Detroit, MI (Girija Natarajan). 14. Cook Children’s Health Care System, Fort Worth, TX (Annie Chi). 15. Connecticut Children’s Hospital, Hartford, CT (Annmarie Golioto). 16. Texas Children’s Hospital, Houston, TX (Kristina Reber). 17. Riley Children’s Hospital, Indianapolis, IN (Rebecca Rose). 18. University of Iowa Children’s Hospital, Iowa City, IA (Julie Lindower). 19. Children’s Mercy Hospitals and Clinics, Kansas City, MO (Julie Weiner). 20. Arkansas Children’s Hospital, Little Rock, AR (Laura Carroll). 21. Children’s Hospital Los Angeles, Los Angeles, CA (Rachel Chapman). 22. American Family Children’s Hospital, Madison, WI (Nina Menda). 23. Le Bonheur Children’s Hospital, Memphis, TN (Mark Weems). 24. Children’s Hospital Wisconsin, Milwaukee, WI (Joanne Lagatta). 25. Children’s Hospital of Minnesota, Minneapolis, MN, (Ann Downey). 26. UCSF Benioff Children’s Hospital, Oakland, CA (Priscilla Joe). 27. Oklahoma Children’s Hospital, Oklahoma City, OK (Patricia Williams, Trent Tipple). 28. Omaha Children’s Hospital, Omaha, NE (Nicole Birge). 29. Children’s Hospital of Orange County, Orange, CA (Michel Mikhael). 27. Advent Health for Children, Orlando, FL (Narendra Dereddy, Rajan Wadhawan). 28. Nemours Children’s Hospital, Orlando, FL (Aaron Weiss). 29. The Children’s Hospital of Philadelphia, Philadelphia, PA (Michael Padula). 30. St. Christopher’s Hospital for Children, Philadelphia, PA (Vilmaris Quinones). 31. Phoenix Children’s Hospital, Phoenix, AZ (Pam Griffiths). 32. Children’s Hospital of Pittsburgh of UPMC, Pittsburgh, PA (Toby Yanowitz). 33. Mayo Eugenia Litta Children’s Hospital, Rochester, MN (Ellen Bendel-Stenzel). 34. Primary Children’s Hospital, Salt Lake City, UT (Con Yee Ling). 35. Rady Children’s Hospital, San Diego, CA (Mark Speziale). 36. Seattle Children’s Hospital, Seattle, WA (Elizabeth Jacobson, Robert DiGeronimo). 37. St. Louis Children’s Hospital, St Louis, MO (Beverly Brozanski, Rakesh Rao). 38. All Children’s Hospital, St. Petersburg, FL (Linda Van Marter). 39. Hospital for Sick Children, Toronto, ON (Kyong-Soon Lee). 40. Children’s National Medical Center, Washington, DC (Billie Short). 41. Nemours Children’s Hospital, Wilmington, DE (Kevin Sullivan). 42. Brenner Children’s Hospital, Winston-Salem, NC (Cherrie Welch).
Author information
Authors and Affiliations
Consortia
Contributions
ABH, KMS, IA, MP, and TY contributed to the conception and design of the study. All authors contributed to the data acquisition and provided critical input during the Children’s Hospitals Neonatal Consortium NEC focus group meetings. IZ conducted data analysis. ABH wrote the first draft of the manuscript. TY helped to critically draft and revise the manuscript. All authors helped revise the manuscript and have approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics
IRB approval was obtained at each participating site prior to entering data into CHND. For analysis of de-identified data, the Stanley Manne Research Center (2011-14673) reviewed and approved this work. The study was performed in accordance with the Declaration of Helsinki.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hair, A.B., Sullivan, K.M., Ahmad, I. et al. Initial surgery for spontaneous intestinal perforation in extremely low birth weight infants is not associated with mortality or in-hospital morbidities. J Perinatol 44, 1746–1754 (2024). https://doi.org/10.1038/s41372-024-02037-8
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41372-024-02037-8
This article is cited by
-
Meconium obstruction of prematurity in tiny babies – towards developing an international consensus
Journal of Perinatology (2025)