Abstract
Objective
Evaluate the association between results of the room air (RA) challenge and death, respiratory morbidity, and neurodevelopmental impairment (NDI) at 2 years' corrected age.
Study design
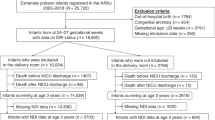
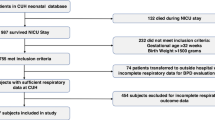
Cohort study of infants born <27 weeks’ gestational age who underwent a RA challenge to determine BPD diagnosis at 36 weeks postmenstrual age.
Results
Of 1022 infants eligible for the RA challenge, 554 underwent testing and 223 passed. Test result was not associated with death or serious respiratory morbidities [adjusted relative risk (aRR) 1.01, 95% confidence interval (CI) 0.65–1.56] or death or moderate/severe NDI (aRR 1.06, 95% CI 0.81–1.39) at 2 years.
Conclusion
Results of the RA challenge were not associated with differences in respiratory or neurodevelopmental morbidity at 2 years, suggesting the RA challenge does not add prognostic value in contemporary extremely preterm infants.
ClinicalTrials.gov ID
Generic Database: NCT00063063.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
Data reported in this paper may be requested through a data use agreement. Further details are available at https://neonatal.rti.org/index.cfm?fuseaction=DataRequest.Home.
References
Stoll BJ, Hansen NI, Bell EF, Walsh MC, Carlo WA, Shankaran S, et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993-2012. JAMA. 2015;314:1039–51.
Horbar JD, Edwards EM, Greenberg LT, Morrow KA, Soll RF, Buus-Frank ME, et al. Variation in performance of neonatal intensive care units in the United States. JAMA Pediatr. 2017;171:e164396.
Vohr BR, Wright LL, Dusick AM, Mele L, Verter J, Steichen JJ, et al. Neurodevelopmental and functional outcomes of extremely low birth weight infants in the National Institute of Child Health and Human Development Neonatal Research Network, 1993-1994. Pediatrics. 2000;105:1216–26.
Schmidt B, Roberts RS, Davis PG, Doyle LW, Asztalos EV, Opie G, et al. Prediction of late death or disability at age 5 years using a count of 3 neonatal morbidities in very low birth weight infants. J Pediatr. 2015;167:982–6.e2.
Poindexter BB, Feng R, Schmidt B, Aschner JL, Ballard RA, Hamvas A, et al. Comparisons and limitations of current definitions of bronchopulmonary dysplasia for the prematurity and respiratory outcomes program. Ann Am Thorac Soc. 2015;12:1822–30.
Hines D, Modi N, Lee SK, Isayama T, Sjors G, Gagliardi L, et al. Scoping review shows wide variation in the definitions of bronchopulmonary dysplasia in preterm infants and calls for a consensus. Acta Paediatr. 2017;106:366–74.
Walsh MC, Yao Q, Gettner P, Hale E, Collins M, Hensman A, et al. Impact of a physiologic definition on bronchopulmonary dysplasia rates. Pediatrics. 2004;114:1305–11.
Carlo WA, Finer NN, Walsh MC, Rich W, Gantz MG, Laptook AR, et al. Target ranges of oxygen saturation in extremely preterm infants. N Engl J Med. 2010;362:1959–69.
Walsh MC, Wilson-Costello D, Zadell A, Newman N, Fanaroff A. Safety, reliability, and validity of a physiologic definition of bronchopulmonary dysplasia. J Perinatol. 2003;23:451–6.
Natarajan G, Pappas A, Shankaran S, Kendrick DE, Das A, Higgins RD, et al. Outcomes of extremely low birth weight infants with bronchopulmonary dysplasia: impact of the physiologic definition. Early Hum Dev. 2012;88:509–15.
Arora P, Dahlgren A, Dawson S, Leuthner J, Lagatta J. Room air challenge predicts duration of supplemental respiratory support for infants with bronchopulmonary dysplasia. J Perinatol. 2021;41:772–8.
Jensen EA, Dysart K, Gantz MG, McDonald S, Bamat NA, Keszler M, et al. The diagnosis of bronchopulmonary dysplasia in very preterm infants: an evidence-based approach. Am J Respir Crit Care Med. 2019;200:751–59
Schmidt B, Whyte RK, Asztalos EV, Moddemann D, Poets C, Rabi Y, et al. Effects of targeting higher vs lower arterial oxygen saturations on death or disability in extremely preterm infants: a randomized clinical trial. JAMA. 2013;309:2111–20.
Group BIUKC, Group BIAC, Group BINZC, Stenson BJ, Tarnow-Mordi WO, Darlow BA. et al. Oxygen saturation and outcomes in preterm infants. N Engl J Med. 2013;368:2094–104.
Darlow BA, Marschner SL, Donoghoe M, Battin MR, Broadbent RS, Elder MJ, et al. Randomized controlled trial of oxygen saturation targets in very preterm infants: two year outcomes. J Pediatr. 2014;165:30–5.e2.
Australia B-I, United Kingdom Collaborative G, Tarnow-Mordi W, Stenson B, Kirby A, Juszczak E, et al. Outcomes of two trials of oxygen-saturation targets in preterm infants. N Engl J Med. 2016;374:749–60.
Askie LM, Darlow BA, Finer N, Schmidt B, Stenson B, Tarnow-Mordi W, et al. Association between oxygen saturation targeting and death or disability in extremely preterm infants in the neonatal oxygenation prospective meta-analysis collaboration. JAMA. 2018;319:2190–201.
Foglia EE, Carper B, Gantz M, DeMauro SB, Lakshminrusimha S, Walsh M, et al. Association between policy changes for oxygen saturation alarm settings and neonatal morbidity and mortality in infants born very preterm. J Pediatr. 2019;209:17–22.e2.
ClinicalTrials.gov. Generic Database of Very Low Birth Weight Infants (GDB). https://clinicaltrials.gov/ct2/show/NCT00063063.
Bayley N. Bayley scales of infant and toddler development. San Antonio, TX: Harcort Assessment, Inc; 2006.
Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol. 1997;39:214–23.
Bell MJ, Ternberg JL, Feigin RD, Keating JP, Marshall R, Barton L, et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann Surg. 1978;187:1–7.
Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. 1978;92:529–34.
Manja V, Lakshminrusimha S, Cook DJ. Oxygen saturation target range for extremely preterm infants: a systematic review and meta-analysis. JAMA Pediatr. 2015;169:332–40.
Huizing MJ, Villamor-Martinez E, Vento M, Villamor E. Pulse oximeter saturation target limits for preterm infants: a survey among European neonatal intensive care units. Eur J Pediatr. 2017;176:51–6.
Coste F, Ferkol T, Hamvas A, Cleveland C, Linneman L, Hoffman J, et al. Ventilatory control and supplemental oxygen in premature infants with apparent chronic lung disease. Arch Dis Child Fetal Neonatal Ed. 2015;100:F233–7.
Kotecha SJ, Edwards MO, Watkins WJ, Henderson AJ, Paranjothy S, Dunstan FD, et al. Effect of preterm birth on later FEV1: a systematic review and meta-analysis. Thorax. 2013;68:760–6.
Martinez FD. Early-life origins of chronic obstructive pulmonary disease. N Engl J Med. 2016;375:871–8.
Wong PM, Lees AN, Louw J, Lee FY, French N, Gain K, et al. Emphysema in young adult survivors of moderate-to-severe bronchopulmonary dysplasia. Eur Respir J. 2008;32:321–8.
Vollsaeter M, Clemm HH, Satrell E, Eide GE, Roksund OD, Markestad T, et al. Adult respiratory outcomes of extreme preterm birth. A regional cohort study. Ann Am Thorac Soc. 2015;12:313–22.
Levin JC, Sheils CA, Gaffin JM, Hersh CP, Rhein LM, Hayden LP. Lung function trajectories in children with post-prematurity respiratory disease: identifying risk factors for abnormal growth. Respir Res. 2021;22:143.
Stern DA, Morgan WJ, Wright AL, Guerra S, Martinez FD. Poor airway function in early infancy and lung function by age 22 years: a non-selective longitudinal cohort study. Lancet. 2007;370:758–64.
Karmaus W, Mukherjee N, Janjanam VD, Chen S, Zhang H, Roberts G, et al. Distinctive lung function trajectories from age 10 to 26 years in men and women and associated early life risk factors—a birth cohort study. Respir Res. 2019;20:98.
Wang X, Dockery DW, Wypij D, Fay ME, Ferris BG Jr. Pulmonary function between 6 and 18 years of age. Pediatr Pulmonol. 1993;15:75–88.
Jordan BK, McEvoy CT. Trajectories of lung function in infants and children: setting a course for lifelong lung health. Pediatrics. 2020;146:e20200417.
Kurihara C, Zhang L, Mikhael M. Newer bronchopulmonary dysplasia definitions and prediction of health economics impacts in very preterm infants. Pediatr Pulmonol. 2021;56:409–17.
Acknowledgements
The authors would like to acknowledge Dr. Michele Walsh for her intellectual contribution to the conception of the study. The National Institutes of Health and the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) provided grant support for the Neonatal Research Network for the Generic Database and the Follow-up Study. NICHD staff provided input into the study design, conduct, analysis, and manuscript drafting; NCATS cooperative agreements provided infrastructure support to the NRN. While NICHD staff had input into the study design, conduct, analysis, and manuscript drafting, the comments and views of the authors do not necessarily represent the views of NICHD, the National Institutes of Health, the Department of Health and Human Services, or the U.S. Government. Data collected at participating sites of the NICHD Neonatal Research Network were transmitted to RTI International, the data coordinating center (DCC) for the network, which stored, managed and analyzed the data included in this study. On behalf of the NRN, RTI International had full access to all the data in the study and take responsibility for the integrity of the data and accuracy of the data analysis. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. We are indebted to our medical and nursing colleagues and the infants and their parents who agreed to take part in this study. The following investigators, in addition to those listed as authors, participated in this study: NRN Steering Committee Chair: Richard A. Polin, MD, Division of Neonatology, College of Physicians and Surgeons, Columbia University, (2011–present). Alpert Medical School of Brown University and Women & Infants Hospital of Rhode Island (UG1 HD27904)—Abbot R. Laptook, MD; Martin Keszler, MD; Betty R. Vohr, MD; Angelita M. Hensman, PhD RNC-NIC; Elisa Vieira, BSN RN; Lucille St. Pierre, BS; Robert T. Burke, MD MPH; Barbara Alksninis, RNC PNP; Andrea Knoll; Mary L. Keszler, MD; Teresa M. Leach, MEd CAES; Elisabeth C. McGowan, MD; Victoria E. Watson, MS CAS. Case Western Reserve University, Rainbow Babies & Children’s Hospital (UG1 HD21364)—Nancy S. Newman, RN; Deanne E. Wilson-Costello, MD; Bonnie S. Siner, RN; Elizabeth Roth, MS. Children’s Mercy Hospital (UG1 HD68284)—William E. Truog, MD; Eugenia K. Pallotto, MD MSCE; Howard W. Kilbride MD; Cheri Gauldin, RN BS CCRC; Anne Holmes RN MSN MBA-HCM CCRC; Kathy Johnson RN, CCRC; Allison Scott, BSN RNC-NIC; Prabhu S. Parimi, MD; Lisa Gaetano, RN MSN. Cincinnati Children’s Hospital Medical Center, University Hospital, and Good Samaritan Hospital (UG1 HD27853, UL1 TR77)—Stephanie L. Merhar, MD MS; Brenda B. Poindexter, MD MS; Kurt Schibler, MD; Kimberly Yolton, PhD; Tanya E. Cahill, MD; Teresa L. Gratton, PA; Cathy Grisby, BSN CCRC; Devan Hayes, BS; Kristin Kirker, CRC; David Russell, JD; Sara Stacey, BA; Sandra Wuertz, RN BSN CLC. Duke University School of Medicine, University Hospital, University of North Carolina, Duke Regional Hospital, and WakeMed Health & Hospitals (UG1 HD40492, UL1 TR1117)—C. Michael Cotten, MD MHS; Ronald N. Goldberg, MD; Ricki F. Goldstein, MD; William F. Malcolm, MD; Patricia L. Ashley, MD; Deesha Mago-Shah, MD; Joanne Finkle, RN JD; Kimberley A. Fisher, PhD FNP-BC IBCLC; Kathryn E. Gustafson, PhD; Matthew M. Laughon, MD MPH; Carl L. Bose, MD; Janice Bernhardt, MS RN; Gennie Bose, RN; Janice Wereszczak, CPNP-AC/PC; Diane Warner, MD MPH; Jennifer Talbert, MS RN; Stephen D. Kicklighter, MD; Alexandra Bentley, MD; Laura Edwards, MD; Ginger Rhodes-Ryan, ARNP MSN, NNP-BC; Donna White, RN-BC BSN. Emory University, Children’s Healthcare of Atlanta, Grady Memorial Hospital, and Emory University Hospital Midtown (UG1 HD27851, UL1 TR454)—Ravi M. Patel, MD MSc; David P. Carlton, MD; Ira Adams-Chapman, MD (deceased); Ellen C. Hale, BS RN CCRC; Yvonne Loggins, RN; Diane Bottcher, RN; Sheena L. Carter, PhD; Salathiel Kendrick-Allwood, MD; Maureen Mulligan LaRossa, RN; Judith Laursen, RN; Colleen Mackie, RRT; Amy Sanders, PsyD; Gloria Smikle, PNP; Lynn Wineski, NNP. Eunice Kennedy Shriver National Institute of Child Health and Human Development—Andrew A. Bremer, MD PhD; Rosemary D. Higgins, MD; Stephanie Wilson Archer, MA. Indiana University, University Hospital, Methodist Hospital, Riley Hospital for Children, and Wishard Health Services (UG1 HD27856, UL1 TR6)—Gregory M. Sokol, MD; Brenda B. Poindexter, MD MS; Heidi Harmon, MD MS; Lu Ann Papile, MD; Susan Gunn, NNP CCRC; Abbey C. Hines, PsyD; Jeffery Joyce, CCRC (deceased); Carolyn Lytle, MD MPH; Dianne E. Herron, RN CCRC; Lucy Smiley, CCRC. McGovern Medical School at The University of Texas Health Science Center at Houston, Children’s Memorial Hermann Hospital, and Memorial Hermann Southwest Hospital (U10 HD21373, UG1 HD87229)—Jon E. Tyson, MD MPH; Amir M. Khan, MD; Kathleen A. Kennedy, MD MPH; Barbara J. Stoll, MD; Ricardo A. Mosquera, MD MS; Andrea F. Duncan, MD MS; Elizabeth Allain, Nora I. Alaniz, BS; PhD; Julie Arldt-McAlister, MSN APRN; Fatima Boricha, MD; Katrina Burson, RN, BSN, Allison G. Dempsey, PhD; Carmen Garcia, RN BSN; Donna J. Hall, RN; Janice John, CPNP; Patrick Jones, MD MA; M. Layne Lillie, RN BSN; Karen Martin, RN; Carrie M. Mason, MA LPA; Georgia E. McDavid, RN; Shannon L. McKee, EdS; Michelle Poe, PhD RN, Kimberly Rennie, PhD; Tina Reddy, MD; Shawna Rodgers, RNC-NIC BSN; Daniel K. Sperry, RN; Emily Stephens, BSN RNC-NIC; Sharon L. Wright, MT (ASCP). Nationwide Children’s Hospital, The Abigail Wexner Research Institute at Nationwide Children’s Hospital, Center for Perinatal Research, The Ohio State University College of Medicine, The Ohio State University Wexner Medical Center, and Riverside Methodist Hospital (UG1 HD68278)—Pablo J. Sánchez, MD; Leif D. Nelin, MD; Jonathan L. Slaughter, MD MPH; Sudarshan R. Jadcherla, MD; Nathalie L. Maitre, MD PhD; Christopher Timan, MD; Keith O. Yeates, MD PhD; Patricia Luzader, RN; Julie Gutentag, RN BSN; Jennifer L. Grothause, BA RN BSN; Melanie Stein, RRT BBS; Rox Ann Sullivan, RN BSN; Cole D. Hague, BA MS; Helen Carey, PT DHSc PCS; Michelle Chao, BS; Stephanie Burkhardt, BS MPH; Margaret Sullivan, BS; Lina Yossef-Salameh, MD; Mary Ann Nelin, MD; Erna Clark, BA; Julie C. Shadd, BSN RD; Courtney Park, RN BSN; Courtney Cira, BS; Erin Fearns; Kristi Small, BS; Sarah A. Keim, PhD MA MS; Christine A. Fortney, RN PhD; Aubrey Fowler, BS, Jacqueline McCool; Lindsay Pietruszewski, PT DPT; Jessica Purnell, BS CCRC; Kyrstin Warnimont, BS; Laura Marzec, MD; Bethany Miller, RN BSN; Demi R. Beckford, MHS; Hallie Baugher, BS MSN; Julia Newton, MPH; Katelyn Levengood, PT DPT; Nancy Batterson, OT/L; Brittany DeSantis, BS. RTI International (UG1 HD36790)—Abhik Das, PhD; Carla M. Bann, PhD; Dennis Wallace, PhD; Jeanette O’Donnell Auman, BS; Margaret Crawford, BS; Jenna Gabrio, BS MPH; Jamie E. Newman, PhD MPH; Lindsay Parlberg, BS; Carolyn M. Petrie Huitema, MS; Kristin M. Zaterka-Baxter, RN BSN. Stanford University, El Camino Hospital, and Lucile Packard Children’s Hospital (UG1 HD27880, UL1 TR93)—Krisa P. Van Meurs, MD; Valerie Chock, MD MS Epi; David K. Stevenson, MD; Susan R. Hintz, MD MS Epi; M. Bethany Ball, BS CCRC; Marian M. Adams, MD; Barbara Bentley, PsychD MSEd; Maria Elena DeAnda, PhD; Anne M. DeBattista, RN PNP PhD; Beth Earhart, PhD; Lynne C. Huffman, MD; Casey E. Krueger, PhD; Ryan E. Lucash, PhD; Melinda S. Proud, RCP; Elizabeth N. Reichert, MA CCRC; Heather Taylor, PhD; Hali E. Weiss, MD; R. Jordan Williams, MD. University of Alabama at Birmingham Health System and Children’s Hospital of Alabama (UG1 HD34216)—Waldemar A. Carlo, MD; Namasivayam Ambalavanan, MD; Myriam Peralta-Carcelen, MD MPH; Kirstin J. Bailey, PhD; Fred J. Biasini, PhD; Stephanie A. Chopko, PhD; Monica V. Collins, RN BSN MaEd; Shirley S. Cosby, RN BSN; Kristy A. Domnanovich, PhD; Chantel J. Jno-Finn, PT DPT; Morissa Ladinsky, MD; Mary Beth Moses, PT MS PCS; Tara E. McNair, RN BSN; Vivien A. Phillips, RN BSN; Julie Preskitt, MSOT MPH; Richard V. Rector, PhD; Kimberlly Stringer, MD MPH; Sally Whitley, MA OTR-L FAOTA; Sheree York Chapman, PT DPT PCS. University of California—Los Angeles, Mattel Children’s Hospital, Santa Monica Hospital, Los Robles Hospital and Medical Center, and Olive View Medical Center (UG1 HD68270)—Uday Devaskar, MD; Meena Garg, MD; Isabell B. Purdy, PhD CPNP; Teresa Chanlaw, MPH; Rachel Geller, RN BSN. University of Iowa, Mercy Medical Center, and Sanford Health (UG1 HD53109, UL1 TR442)—Edward F. Bell, MD; Tarah T. Colaizy, MD MPH; John A. Widness, MD; Jane E. Brumbaugh, MD; Heidi M. Harmon, MD; Karen J. Johnson, RN BSN; Mendi L. Schmelzel, RN MSN; Jacky R. Walker, RN; Claire A. Goeke, RN; Sarah E. Faruqui, RN MSN; Diane L. Eastman, RN CPNP MA; Michelle L. Baack, MD; Laurie A. Hogden, MD; Megan M. Henning, RN; Chelsey Elenkiwich, BSN RN; Megan Broadbent, RN BSN; Sarah Van Muyden, BSN RN; Dan L. Ellsbury, MD; Donia B. Bass, RNC-NIC; Tracy L. Tud, RN. University of New Mexico Health Sciences Center (UG1 HD53089, UL1 TR41)—Kristi L. Watterberg, MD; Janell Fuller, MD; Robin K. Ohls, MD; Conra Backstrom Lacy, RN; Carol Hartenberger, BSN MPH; Sandra Sundquist Beauman, MSN RNC; Mary Ruffner Hanson, RN BSN; Jean R. Lowe, PhD; Elizabeth Kuan, RN BSN. University of Pennsylvania, Hospital of the University of Pennsylvania, Pennsylvania Hospital, Children’s Hospital of Philadelphia, and Virtua Voorhees Hospital (UG1 HD68244)—Sara B. DeMauro, MD MSCE; Eric C. Eichenwald, MD; Barbara Schmidt, MD MSc; Haresh Kirpalani, MB MSc; Soraya Abbasi, MD; Aasma S. Chaudhary, BS RRT; Toni Mancini, RN BSN CCRC; Dara M. Cucinotta, RN; Judy C. Bernbaum, MD; Noah Cook, MD; Marsha Gerdes, PhD; Sarvin Ghavam, MD; Hallam Hurt, MD; Jonathan Snyder, RN BSN, Kristina Ziolkowski, CMA(AAMA) CCRP. University of Rochester Medical Center, Golisano Children’s Hospital, and the University of Buffalo Women’s and Children’s Hospital of Buffalo (UG1 HD68263, UL1 TR42)—Carl T. D’Angio, MD; Ronnie Guillet, MD PhD; Gary J. Myers, MD; Satyan Lakshminrusimha, MD; Anne Marie Reynolds, MD; Holly I.M. Wadkins; Michael G. Sacilowski, BS; Rosemary L. Jensen; Deanna Maffett, RN; Joan Merzbach, LMSW; William Zorn, PhD; Osman Farooq, MD; Ashley Williams, MSEd; Julianne Hunn, BS; Stephanie Guilford, BS; Kelley Yost, PhD; Mary Rowan, RN; Diane Prinzing; Melissa Bowman, RN NP; Ann Marie Scorsone, MS CCRC; Michelle Hartley-McAndrew, MD; Caitlin Fallone, MA; Kyle Binion, BS; Constance Orme; Premini Sabaratnam, MPH; Alison Kent, BMBS FRACP MD; Cassandra A. Horihan, MS; Rachel Jones; Elizabeth Boylin, BA; Daisy Rochez, BS MHA; Emily Li, BA; Jennifer Kachelmeyer, BS; Kimberly G. McKee, MPH; Kelly R. Coleman, PsyD. University of Texas Southwestern Medical Center, Parkland Health & Hospital System, and Children’s Medical Center Dallas (UG1 HD40689)—Myra H. Wyckoff, MD; Luc P. Brion, MD; Roy J. Heyne, MD; Diana M. Vasil, MSN BSN RNC-NIC; Lijun Chen, RN PhD; Sally S. Adams, MS RN CPNP; Maria M. De Leon, RN BSN; Frances Eubanks, RN BSN; E. Rebecca McDougald, MSN APRN CPNP-PC/AC; Lara Pavageau, MD; Pollieanna Sepulveda, RN; Alicia Guzman; Elizabeth Heyne, PsyD PA-C; Lizette E. Lee, RN; Azucena Vera, AS; Jillian Waterbury, DNP RN CPNP-PC; Kristine Tolentino-Plata, MS; Cathy Twell Boatman, MS CIMI. University of Utah Medical Center, Intermountain Medical Center, McKay-Dee Hospital, Utah Valley Hospital, and Primary Children’s Medical Center (UG1 HD87226, UL1 TR105)—Bradley A. Yoder, MD; Mariana Baserga, MD MSCI; Roger G. Faix, MD; Sarah Winter, MD; Stephen D. Minton, MD; Mark J. Sheffield, MD; Carrie A. Rau, RN BSN CCRC; Shawna Baker, RN; Jill Burnett, RNC BSN; Susan Christensen, RN; Laura Cole Bledsoe, RN; Sean D. Cunningham, PhD; Brandy Davis, RN BSN; Jennifer O. Elmont, RN BSN; Becky Hall, APRN; Manndi C. Loertscher, BS CCRP; Trisha Marchant, RNC BSN; Earl Maxson, RN CCRN; Kandace M. McGrath, BS; Hena G. Mickelsen, BA; Galina Morshedzadeh, BSN APRN; D. Melody Parry, RN BSN; Brixen A. Reich, MSN RNC CCRC; Susan T. Schaefer, RN BSN RRT; Kelly Stout, PhD; Ashley L. Stuart, PhD; Kimberlee Weaver-Lewis, RN MS; Kathryn D. Woodbury, RN BSN. Wayne State University, Hutzel Women’s Hospital, and Children’s Hospital of Michigan (UG1 HD21385)—Seetha Shankaran, MD; Girija Natarajan, MD; Beena G. Sood, MD MS; Athina Pappas, MD; Monika Bajaj, MD; Melissa February, MD; Prashant Agarwal, MD; Sanjay Chawla, MD; Rebecca Bara, RN BSN; Kirsten Childs, RN BSN; Eunice Hinz Woldt, RN MSN; Laura Goldston, MA, Bogdan Panaitescu MD PhD; John Barks, MD; Stephanie A. Wiggins, MS; Mary K. Christensen, BA RRT; Martha Carlson, MD; Diane F. White, RRT CCRP.
Funding
The National Institutes of Health and the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) (U10 HD21373, UG1 HD21364, UG1 HD21385, UG1 HD27851, UG1 HD27853, UG1 HD27856, UG1 HD27880,UG1 HD27904, UG1 HD34216, UG1 HD36790, UG1 HD40492, UG1 HD40689, UG1 HD53089, UG1 HD53109, UG1 HD68244, UG1 HD68270, UG1 HD68278, UG1 HD68263, UG1 HD68284; UG1 HD87226, UG1 HD87229) and the National Center for Advancing Translational Sciences (NCATS) (UL1 TR6, UL1 TR41, UL1 TR42, UL1 TR77, UL1 TR93, UL1 TR105, UL1 TR442, UL1 TR454, UL1 TR1117, provided grant support for the Neonatal Research Network, including for the Follow-up Study.
Author information
Authors and Affiliations
Consortia
Contributions
All authors were involved in the study design, analysis, and manuscript revision. All authors read and approved the final manuscript. Aleem is the guarantor who accepts full responsibility for the work and the conduct of the study, has access to the data, and controlled the decision to publish. Samia Aleem contributed to the conception and design of the study, the data interpretation, the manuscript drafting, and the critical revision of the manuscript. Barbara Do had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Barbara Do contributed to the design of the study, the data interpretation, the manuscript drafting, and the critical revision of the manuscript. Marie Gantz contributed to the conception and design of the study, the data interpretation, and the critical revision of the manuscript. Anna Maria Hibbs contributed to the conception and design of the study and the critical revision of the manuscript. Erik Jensen contributed to the conception and design of the study, the data interpretation, and the critical revision of the manuscript. Michael Cotten contributed to the conception and design of the study, the data interpretation, and the critical revision of the manuscript. William Malcolm contributed to the conception and design of the study, the data interpretation, and the critical revision of the manuscript. Alan Jobe contributed to the conception of the study and the critical revision of the manuscript. Rachel Greenberg contributed to the conception and design of the study, the data interpretation, the manuscript drafting, and the critical revision of the manuscript.
Corresponding author
Ethics declarations
Competing interests
RGG has received support from industry for research services (https://dcri.org/about-us/conflict-of-interest/). The authors have no other conflicts of interest relevant to this article to disclose.
Ethics approval and consent to participate
Each study center’s Institutional Review Board approved the collection of data during both the initial hospitalization and follow-up under a waiver of consent or after informed consent was obtained from parents or legal guardians.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Aleem, S., Do, B.T., Gantz, M.G. et al. The association of the room air challenge with long-term outcomes in extremely preterm infants. J Perinatol 44, 1300–1306 (2024). https://doi.org/10.1038/s41372-024-02074-3
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41372-024-02074-3