Abstract
Objective
To evaluate the factors that improve professional and personal well-being amongst women in neonatology (WiN).
Study design
A 30-question survey of multiple choice, rank order, and open-ended questions focused on professional and personal factors that affect the well-being of WiN members. Quantitative and qualitative methods were used to determine leading factors and themes.
Results
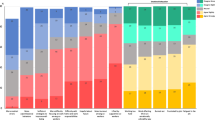
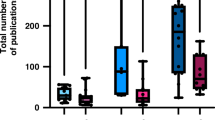
Of 326 respondents, 64% felt “well” professionally over half of the time. Professional well-being was most affected by scheduling flexibility, helping patients, administrative and staffing support, feelings of being valued, and clinical workload/acuity. Time for family and self-care, having domestic help, and scheduling flexibility were factors that most positively impacted personal well-being.
Conclusion
In this national survey, WiN members identified the factors that can improve their well-being. Strategic planning and targeted interventions are urgently needed to enhance work-life integration and job satisfaction, leading to improved neonatal workforce retention and improved quality of patient care.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
De-identified survey responses may be provided upon request to the corresponding author.
References
Lianov L. A powerful antidote to physician burnout: intensive healthy lifestyle and positive psychology approaches. Am J Lifestyle Med. 2021;15:563–6.
Maslach C, Leiter MP. Understanding the burnout experience: recent research and its implications for psychiatry. World Psychiatry. 2016;15:103–11.
Shanafelt TD, Dyrbye LN, West CP. Addressing physician burnout: the way forward. JAMA. 2017;317:901–2.
Shanafelt TD, Noseworthy JH. Executive leadership and physician well-being nine organizational strategies to promote engagement and reduce burnout. Mayo Clin Proc. 2017;92:129–46.
Menon NK, Shanafelt TD, Sinsky CA, Linzer M, Carlasare L, Brady KJS, et al. Association of physician burnout with suicidal ideation and medical errors. JAMA Netw open. 2020;3:e2028780.
Yeluru H, Newton HL, Kapoor R. Physician burnout through the female lens: a silent. Crisis Front Public Heal. 2022;10:880061.
Koval LM. Medscape Pediatrician Lifestyle, Happiness & Burnout Report 2023. 2023. https://www.medscape.com/slideshow/2023-lifestyle-pediatrician-6016089#1.
McClafferty HH, Hubbard DK, Foradori D, Brown ML, Profit J, Tawfik DS, et al. Physician health and wellness. Pediatrics 2022;150. https://doi.org/10.1542/peds.2022-059665.
Haidari E, Main EK, Cui X, Cape V, Tawfik DS, Adair KC, et al. Maternal and neonatal health care worker well-being and patient safety climate amid the COVID-19 pandemic. J Perinatol. 2021;41:961–9.
Tawfik DS, Profit J. Provider burnout: Implications for our perinatal patients. Semin Perinatol. 2020;44:151243.
Bellieni CV, Righetti P, Ciampa R, Iacoponi F, Coviello C, Buonocore G. Assessing burnout among neonatologists. J Matern-Fetal Neonatal Med. 2012;25:2130–4.
Guaman MC, Miller ER, Dammann CEL, Bishop CE, Machut KZ. Neonatologist staffing models: urgent change is needed. J Perinatol. 2022;42:1556–7.
Bishop CE, Machut KZ, Dammann CEL, Guaman MC, Miller ER, Lakshminrusimha S. Academic neonatologist—a species at the brink of extinction? J Perinatol. 2023;12:1526–29.
Weintraub AS, Geithner EM, Stroustrup A, Waldman ED. Compassion fatigue, burnout and compassion satisfaction in neonatologists in the US. J Perinatol. 2016;36:1021–6.
Bline K, Dammann CEL. Improving workplace culture by increasing financial transparency. Pediatr Res. 2022;92:1492–3.
Lakshminrusimha S, Olsen SL, Lubarsky DA. Behavioral economics in neonatology—balancing provider wellness and departmental finances. J Perinatol. 2022;42:683–8.
Machut KZ, Kushnir A, Oji-Mmuo CN, Kataria-Hale J, Lingappan K, Kwon S, et al. Effect of coronavirus disease-2019 on the workload of neonatologists. J Pediatr. 2022;242:145–151.e1.
Education AC for GM, Brigham T, Barden C, Nurses AA of CC, Dopp AL, Pharmacists AS of HS et al. A Journey to construct an all-encompassing conceptual model of factors affecting clinician well-being and resilience. NAM Perspect 2018; 8. https://doi.org/10.31478/201801b.
Lall MD, Gaeta TJ, Chung AS, Chinai SA, Garg M, Husain A, et al. Assessment of physician well-being, part two: beyond burnout. West J Emerg Med. 2019;20:291–304.
Tawfik DS, Shanafelt TD, Dyrbye LN, Sinsky CA, West CP, Davis AS, et al. Personal and professional factors associated with work-life integration among US physicians. JAMA Netw Open. 2021;4:e2111575.
Machut KZ, Lingappan K, Savich R, Dammann CEL. Toolkit for gender equity in pediatrics. Pediatr Res 2024;95:594–7.
Machut KZ, Bhombal S, Escobedo M, Kataria-Hale J, Kushnir A, Lingappan K, et al. Call to action: gender equity in neonatology. J Perinatol. 2022;42:982–3.
Macy ML, Leslie LK, Turner A, Freed GL. Growth and changes in the pediatric medical subspecialty workforce pipeline. Pediatr Res. 2021;89:1297–303.
Brower KJ. Physician Mental Health and Well-Being, Research and Practice. 2017; 295–323.
Webber S, Babal JC, Shadman KA, Coller RJ, Moreno MA. Exploring academic pediatrician perspectives of factors impacting physician well-being. Acad Pediatr. 2020;20:833–9.
Brady KJS, Trockel MT, Khan CT, Raj KS, Murphy ML, Bohman B, et al. What do we mean by physician wellness? A systematic review of its definition and measurement. Acad Psychiatry. 2018;42:94–108.
Trockel M, Hamidi M, Murphy ML, deVries PP, Bohman B. 2016 Physician Wellness Survey Full Report. 2017.
Wilson PM, Batra M, Kemper KJ, Mahan JD, Staples BB, Serwint JR. Physician well-being. Pediatr Rev. 2019;40:12–20.
Tucker P, Bejerot E, Kecklund G, Aronsson G, Åkerstedt T. The impact of work time control on physicians’ sleep and well-being. Appl Erg. 2015;47:109–16.
Erhard M, Schoenfelder J, Fügener A, Brunner JO. State of the art in physician scheduling. Eur J Oper Res. 2018;265:1–18.
Patruno J, Flicker A. Addressing physician burnout and ensuring high-quality care of the physician workforce. Obstet Gynecol. 2021;137:958–9.
McAdams RM. Fatigue and fallibility: the perils of prolonged shifts for neonatologists. J Perinatol. 2023;43:1530–4.
Well-Being C on SA to IPC by SC, Medicine NA of, Medicine NA of S Engineering, and Taking Action Against Clinician Burnout. 2019. https://doi.org/10.17226/25521.
Tawfik DS, Profit J, Webber S, Shanafelt TD. Organizational factors affecting physician well-being. Curr Treat Options Pediatr. 2019;5:11–25.
Shanafelt TD, Wang H, Leonard M, Hawn M, McKenna Q, Majzun R, et al. Assessment of the association of leadership behaviors of supervising physicians with personal-organizational values alignment among staff physicians. JAMA Netw Open. 2021;4:e2035622.
Gogo A, Osta A, McClafferty H, Rana DT. Cultivating a way of being and doing: Individual strategies for physician well-being and resilience. Curr Probl Pediatr Adolesc Heal Care. 2019;49:100663.
Makowski MS, Palomo C, Vries P, de, Shanafelt TD. Employer-provided professional coaching to improve self-compassion and burnout in physicians. Mayo Clin Proc. 2022;97:628–9.
Profit J, Cui X, Tawfik D, Adair KC, Sexton JB. “WISER” intervention to reduce healthcare worker burnout – 1 year follow up. J Perinatol 2024;1–5.
Eckleberry-Hunt J, Kirkpatrick H, Barbera T. The problems with burnout research. Acad Med. 2018;93:367–70.
Dyrbye LN, Shanafelt TD, Gill PR, Satele DV, West CP. Effect of a professional coaching intervention on the well-being and distress of physicians. JAMA Intern Med. 2019;179:1406–14.
West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016;388:2272–81.
Brady KJS, Kazis LE, Sheldrick RC, Ni P, Trockel MT. Selecting physician well-being measures to assess health system performance and screen for distress: conceptual and methodological considerations. Curr Probl Pediatr Adolesc Heal Care. 2019;49:100662.
Mann A, Shah AN, Thibodeau PS, Dyrbye L, Syed A, Woodward MA, et al. Online well-being group coaching program for women physician trainees. JAMA Netw Open. 2023;6:e2335541.
Lin MP, Lall MD, Samuels‐Kalow M, Das D, Linden JA, Perman S, et al. Impact of a women‐focused professional organization on academic retention and advancement: perceptions from a qualitative study. Acad Emerg Med. 2019;26:303–16.
Hartzband P, Groopman J. Physician burnout, interrupted. N Engl J Med. 2020;382:2485–7.
Swensen SJ, Shanafelt T. An organizational framework to reduce professional burnout and bring back joy in practice. Jt Comm J Qual Patient Saf. 2017;43:308–13.
Sinsky CA, Shanafelt TD, Dyrbye LN, Sabety AH, Carlasare LE, West CP. Health care expenditures attributable to primary care physician overall and burnout-related turnover: a cross-sectional analysis. Mayo Clin Proc. 2022;97:693–702.
Author information
Authors and Affiliations
Contributions
DY and SVR contributed to the survey design, quantitative data analysis, manuscript preparation, and revision. Qualitative statistician (CS) analyzed and created themes for text responses. All authors were instrumental in analyzing survey data, drafting the manuscript, and contributing to revisions.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was reviewed by the Institutional Review Board at Emory University. It was deemed exempt using the criteria for exemption under 45 CFR 46.104(d)(2)(i) Tests, surveys, interviews, or observation (non-identifiable).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yanni, D., Scheid, A., Sinha, C.B. et al. Improving well-being among women in neonatology. J Perinatol 45, 580–588 (2025). https://doi.org/10.1038/s41372-024-02091-2
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41372-024-02091-2
This article is cited by
-
NIH-funded neonatologist physician-scientists: an exploration of equity and success
Pediatric Research (2025)