Abstract
Background
There is limited evidence on the efficacy of antenatal steroids (ANS) among women with multiple gestations at risk of late preterm delivery.
Study design
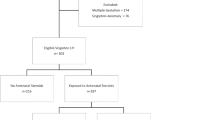
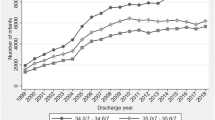
This retrospective study included multiple gestation, late preterm infants (340/7–366/7 weeks’ gestational age), born between January 2013 and December 2022. The primary outcome was composite respiratory outcome, defined as the need for respiratory support by 72 hours of age. Logistic and linear regressions were performed to compare the primary and secondary outcomes with and without exposure to any ANS, adjusted for gestational age, sex of infant, histologic chorioamnionitis, and intrauterine growth restriction.
Results
The composite respiratory outcome was significantly lower in any ANS group compared to no ANS group (28.6% vs. 33.7%) [adjusted odds ratio 0.50, 95% CI, 0.33–0.75, p < 0.001].
Conclusion
In late preterm multiple gestation infants, any ANS exposure was associated with lower risk of composite respiratory outcome.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Blencowe H, Cousens S, Chou D, Oestergaard M, Say L, Moller AB, et al. Born Too Soon Preterm Birth Action Group. Born too soon: the global epidemiology of 15 million preterm births. Reprod Health. 2013;10:S2. https://doi.org/10.1186/1742-4755-10-S1-S2.
Raju TN, Higgins RD, Stark AR, Leveno KJ. Optimizing care and outcome for late-preterm (near-term) infants: a summary of the workshop sponsored by the National Institute of Child Health and Human Development. Pediatrics. 2006;118:1207–14. https://doi.org/10.1542/peds.2006-0018.
Martin JA, Hamilton BE, Osterman MJK, Driscoll AK. Births: final data for 2018. Natl Vital Stat Rep. 2019;68:1–47.
Karnati S, Kollikonda S, Abu-Shaweesh J. Late preterm infants—changing trends and continuing challenges. Int J Pediatr Adolesc Med. 2020;7:36–44. https://doi.org/10.1016/j.ijpam.2020.02.006.
Petrini JR, Dias T, McCormick MC, Massolo ML, Green NS, Escobar GJ. Increased risk of adverse neurological development for late preterm infants. J Pediatr. 2009;154:169–76. https://doi.org/10.1016/j.jpeds.2008.08.020.
Hirvonen M, Ojala R, Korhonen P, Haataja P, Eriksson K, Gissler M, et al. Cerebral palsy among children born moderately and late preterm. Pediatrics. 2014;134:e1584–93. https://doi.org/10.1542/peds.2014-0945.
Stene-Larsen K, Brandlistuen RE, Lang AM, Landolt MA, Latal B, Vollrath ME. Communication impairments in early term and late preterm children: a prospective cohort study following children to age 36 months. J Pediatr. 2014;165:1123–8. https://doi.org/10.1016/j.jpeds.2014.08.027.
Chan E, Quigley MA. School performance at age 7 years in late preterm and early term birth: a cohort study. Arch Dis Child Fetal Neonatal Ed. 2014;99:F451–7. https://doi.org/10.1136/archdischild-2014-306124.
Guy A, Seaton SE, Boyle EM, Draper ES, Field DJ, Manktelow BN, et al. Infants born late/moderately preterm are at increased risk for a positive autism screen at 2 years of age. J Pediatr. 2015;166:269–75.e3. https://doi.org/10.1016/j.jpeds.2014.10.053.
Lindström K, Lindblad F, Hjern A. Preterm birth and attention-deficit/hyperactivity disorder in schoolchildren. Pediatrics. 2011;127:858–65. https://doi.org/10.1542/peds.2010-1279.
Chauhan SP, Scardo JA, Hayes E, Abuhamad AZ, Berghella V. Twins: prevalence, problems, and preterm births. Am J Obstet Gynecol. 2010;203:305–15. https://doi.org/10.1016/j.ajog.2010.04.031.
Luke B, Brown MB. Contemporary risks of maternal morbidity and adverse outcomes with increasing maternal age and plurality. Fertil Steril. 2007;88:283–93. https://doi.org/10.1016/j.fertnstert.2006.11.008.
McGoldrick E, Stewart F, Parker R, Dalziel SR. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev. 2020;12:CD004454. https://doi.org/10.1002/14651858.CD004454.pub4.
Roberts D, Brown J, Medley N, Dalziel SR. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev. 2017;3:CD004454. https://doi.org/10.1002/14651858.CD004454.pub3.
Sotiriadis A, Tsiami A, Papatheodorou S, Baschat AA, Sarafidis K, Makrydimas G. Neurodevelopmental outcome after a single course of antenatal steroids in children born preterm: a systematic review and meta-analysis. Obstet Gynecol. 2015;125:1385–96. https://doi.org/10.1097/AOG.0000000000000748.
Chawla S, Natarajan G, Shankaran S, Pappas A, Stoll BJ, Carlo WA, et al. National Institute of Child Health and Human Development Neonatal Research Network. Association of neurodevelopmental outcomes and neonatal morbidities of extremely premature infants with differential exposure to antenatal steroids. JAMA Pediatr. 2016;170:1164–72. https://doi.org/10.1001/jamapediatrics.2016.1936.
Porto AM, Coutinho IC, Correia JB, Amorim MM. Effectiveness of antenatal corticosteroids in reducing respiratory disorders in late preterm infants: randomised clinical trial. BMJ. 2011;342:d1696. https://doi.org/10.1136/bmj.d1696.
Yenuberi H, Ross B, Sasmita Tirkey R, Benjamin SJ, Rathore S, Karuppusami R, et al. Late-preterm antenatal steroids for reduction of neonatal respiratory complications: a randomized controlled trial. Obstet Gynecol. 2024;143:468–74. https://doi.org/10.1097/AOG.0000000000005520.
Gyamfi-Bannerman C, Thom EA, Blackwell SC, Tita AT, Reddy UM, Saade GR, et al. Antenatal betamethasone for women at risk for late preterm delivery. N Engl J Med. 2016;374:1311–20. https://doi.org/10.1056/NEJMoa1516783.
Ben-David A, Zlatkin R, Bookstein-Peretz S, Meyer R, Mazaki-Tovi S, Yinon Y. Does antenatal steroids treatment in twin pregnancies prior to late preterm birth reduce neonatal morbidity? Evidence from a retrospective cohort study. Arch Gynecol Obstet. 2020;302:1121–6. https://doi.org/10.1007/s00404-020-05709-w.
Zhu J, Zhao Y, An P, Zhao Y, Li S, Zhou J, et al. Antenatal corticosteroid treatment during the late-preterm period and neonatal outcomes for twin pregnancies. JAMA Netw Open. 2023;6:e2343781. https://doi.org/10.1001/jamanetworkopen.2023.43781.
Committee on Obstetric Practice. Committee opinion no. 713: antenatal corticosteroid therapy for fetal maturation. Obstet Gynecol. 2017;130:e102–9. https://doi.org/10.1097/AOG.0000000000002237.
Norman J, Shennan A, Jacobsson B, Stock SJ. FIGO Working Group for Preterm Birth. FIGO good practice recommendations on the use of prenatal corticosteroids to improve outcomes and minimize harm in babies born preterm. Int J Gynaecol Obstet. 2021;155:26–30. https://doi.org/10.1002/ijgo.13836.
Vandenbroucke JP, von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, et al. STROBE Initiative. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. PLoS Med. 2007;4:e297. https://doi.org/10.1371/journal.pmed.0040297.
Adamkin DH. Neonatal hypoglycemia. Semin Fetal Neonatal Med. 2017;22:36–41. https://doi.org/10.1016/j.siny.2016.08.007.
Zdanowicz JA, Sommer E, Raio L, Nelle M, Gerull R. Do late preterm twins face an increased neonatal morbidity compared with singletons? Swiss Med Wkly. 2018;148:w14581. https://doi.org/10.4414/smw.2018.14581.
Mekic N, Selimovic A, Cosickic A, Mehmedovic M, Hadzic D, Zulic E, et al. Predictors of adverse short-term outcomes in late preterm infants. BMC Pediatr. 2023;23:298. https://doi.org/10.1186/s12887-023-04112-z.
Scheuchenegger A, Lechner E, Wiesinger-Eidenberger G, Weissensteiner M, Wagner O, Schimetta W, et al. Short-term morbidities in moderate and late preterm infants. Klin Padiatr. 2014;226:216–20. https://doi.org/10.1055/s-0033-1355394.
Tsai ML, Lien R, Chiang MC, Hsu JF, Fu RH, Chu SM, et al. Prevalence and morbidity of late preterm infants: current status in a medical center of Northern Taiwan. Pediatr Neonatol. 2012;53:171–7. https://doi.org/10.1016/j.pedneo.2012.04.003.
Author information
Authors and Affiliations
Contributions
Pradeep Kumar Velumula: conceptualization, methodology, investigation, data curation, writing original draft; Praveen Kumar Boddu: methodology, investigation, writing—review and editing; Luna Khanal: investigation, writing—review and editing; Sanket Jani: conceptualization, methodology, writing—review and editing; Nithi Fernandes: conceptualization, methodology, writing—review and editing; Ronald Thomas: analysis, writing—review and editing; Monika Bajaj: analysis, writing—review and editing; Sanjay Chawla: conceptualization, methodology, writing—review and editing, supervision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Institutional Review Board (IRB) approval was obtained from Central Michigan University before initiation of the study, (IRB number: 2021-1527). The requirement of informed consent was waived, and all methods were performed in accordance with the relevant guidelines and regulations.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Velumula, P.K., Boddu, P.K., Khanal, L. et al. Association of antenatal steroid administration with neonatal morbidities among late preterm multiple gestation infants. J Perinatol 45, 24–29 (2025). https://doi.org/10.1038/s41372-024-02130-y
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41372-024-02130-y