Abstract
Objective
We previously reported the possible pathogenic role, among infants born ≤29 weeks, of transfusions in bronchopulmonary dysplasia. The present study examined this association in infants born >31 weeks.
Study design
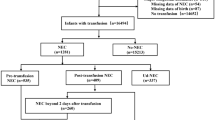
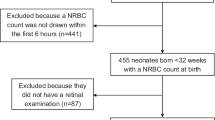
Analysis of red blood cell (RBC) and platelet transfusions in five NICUs to infants born >31 weeks, and chronic neonatal lung disease (CNLD) at six-weeks of age.
Results
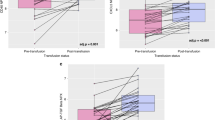
Seven-hundred-fifty-one infants born >31 weeks were still in the NICU when six-weeks of age. CNLD was identified in 397 (53%). RBC and platelet transfusions were independently associated with CNLD after controlling for potential confounders. For every transfusion, the adjusted odds of developing CNLD increased by a factor of 1.64 (95% CI, 1.38–2.02; p < 0.001).
Conclusions
Among NICU patients born >31 weeks, transfusions received by six weeks are associated with CNLD incidence and severity. Though we controlled for known confounding variables in our regression models, severity of illness is an important confounder that limits our conclusions.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
A deidentified data set is available by contacting the corresponding author.
References
Kapur N, Nixon G, Robinson P, Massie J, Prentice B, Wilson A, et al. Respiratory management of infants with chronic neonatal lung disease beyond the NICU: A position statement from the Thoracic Society of Australia and New Zealand. Respirology. 2020;25:880–8.
Holzfurtner L, Shahzad T, Dong Y, Rekers L, Selting A, Staude B, et al. When inflammation meets lung development-an update on the pathogenesis of bronchopulmonary dysplasia. Mol Cell Pediatr. 2022;9:7.
Bahr TM, Snow GL, Christensen TR, Davenport P, Henry E, Tweddell SM, et al. Can red blood cell and platelet transfusions have a pathogenic role in bronchopulmonary dysplasia? J Pediatr. 2024;265:113836.
Suzuki G, Ichibayashi R, Masuyama Y, Yamamoto S, Serizawa H, Nakamichi Y, et al. Association of red blood cell and platelet transfusions with persistent inflammation, immunosuppression, and catabolism syndrome in critically ill patients. Sci Rep. 2022;12:629.
Bahr TM, Ohls RK, Ilstrup SJ, Christensen RD. NICU patients receiving more than 25 platelet transfusions. Am J Perinatol. 2023. https://doi.org/10.1055/a-2073-3848.
Dohner ML, Wiedmeier SE, Stoddard RA, Null D Jr, Lambert DK, Burnett J, et al. Very high users of platelet transfusions in the neonatal intensive care unit. Transfusion. 2009;49:869–72.
Curley A, Stanworth SJ, Willoughby K, Fustolo-Gunnink SF, Venkatesh V, Hudson C, et al. PlaNeT2 MATISSE Collaborators. Randomized trial of platelet-transfusion thresholds in neonates. N Engl J Med. 2019;380:242–51.
Scrivens A, Reibel NJ, Heeger L, Stanworth S, Lopriore E, New HV, et al. Neonatal transfusion network. Survey of transfusion practices in preterm infants in Europe. Arch Dis Child Fetal Neonatal Ed. 2023;108:360–6.
Davenport P, Sola-Visner M. Immunologic effects of red blood cell and platelet transfusions in neonates. Curr Opin Hematol. 2022;29:297–305.
Dani C, Poggi C, Gozzini E, Leonardi V, Sereni A, Abbate R, et al. Red blood cell transfusions can induce proinflammatory cytokines in preterm infants. Transfusion. 2017;57:1304–10.
Delaney C, Davizon-Castillo P, Allawzi A, Posey J, Gandjeva A, Neeves K, et al. Platelet activation contributes to hypoxia-induced inflammation. Am J Physiol Lung Cell Mol Physiol. 2021;320:L413–21.
Jensen EA, Dysart K, Gantz MG, McDonald S, Bamat NA, Keszler M, et al. The diagnosis of bronchopulmonary dysplasia in very preterm infants. An evidence-based approach. Am J Respir Crit Care Med. 2019;200:751–9.
Henry E, Christensen RD, Sheffield MJ, Eggert LD, Carroll PD, Minton SD, et al. Why do four NICUs using identical RBC transfusion guidelines have different gestational age-adjusted RBC transfusion rates? J Perinatol. 2015;35:132–6.
Pearl J, Glymour M, Jewell NP. Causal inference in statistics – a primer. John Wiley and Sons Ltd., West Sussex, UK, 2021.
Bahr TM, Christensen TR, Henry E, Astin M, Ilstrup SJ, Ohls RK, et al. Platelet transfusions in a multi-neonatal intensive care unit health care organization before and after publication of the PlaNeT-2 clinical trial. J Pediatr. 2023;257:113388.
Davenport PE, Chan Yuen J, Briere J, Feldman HA, Sola-Visner MC, Leeman KT. Implementation of a neonatal platelet transfusion guideline to reduce non-indicated transfusions using a quality improvement framework. J Perinatol. 2021;41:1487–94.
Sola-Visner M, Delaney C, Davenport P. EBNEO commentary: platelet transfusions in neonates and brain development: the new frontier. Acta Paediatr. 2023;112:1826–7.
Davenport P, Soule-Albridge E, Sola-Visner M. Hemostatic and immunologic effects of platelet transfusions in neonates. Clin Perinatol. 2023;50:793–803.
Bianchi M, Orlando N, Barbagallo O, Sparnacci S, Balentini CG, Carducci B, et al. Allogenic cord blood red blood cells: assessing cord blood unit fractionation and validation. Blood Transfus. 2021;19:435–44.
Teofili L, Papacci P, Orlando N, Bianchi M, Pasciuto T, Mozzetta I, et al. BORN study: a multicenter randomized trial investigating cord blood red blood cell transfusions to reduce the severity of retinopathy of prematurity in extremely low gestational age neonates. Trials. 2022;23:1010.
Teofili L, Papacci P, Giannantonio C, Bianchi M, Valentini DG, Vento G. Allogenic cord blood transfusion in preterm infants. Clin Perinatol. 2023;50:88193.
Christensen RD, Bahr TM, Christensen TR, Ohls RK, Krong J, Carlton LC, et al. Banked term umbilical cord blood to meet the packed red blood cell transfusion needs of extremely-low-gestational-age neonates: a feasibility analysis. J Perinatol. 2023. https://doi.org/10.1038/s41372-023-01833-y.
Author information
Authors and Affiliations
Contributions
TMB: Conceptualization, methodology, statistical analysis, data curation, writing-review & editing, final approval of the manuscript. RKO: Conceptualization, writing—review & editing, final approval of the manuscript. EH: Conceptualization, data curation, final approval of the manuscript. PD: Writing—review & editing, final approval of the manuscript. SJI: Conceptualization, data curation, writing-review & editing, final approval of the manuscript. WEK Conceptualization, writing—review & editing, final approval of the manuscript. BAY: Conceptualization, writing—review & editing, final approval of the manuscript. MCS-V; Writing—review & editing, final approval of the manuscript. RDC: Conceptualization, methodology, data curation, writing—original draft, writing—review & editing, final approval of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The Institutional Review Board of Intermountain Health approved the proposal for this data-only retrospective analysis and determined this to be exempt from the need for individual informed consent (IRB# 1052045). All study activities were performed in accordance with Intermountain Health IRB and privacy guidelines and regulations.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bahr, T.M., Ohls, R.K., Henry, E. et al. The number of blood transfusions received and the incidence and severity of chronic lung disease among NICU patients born >31 weeks gestation. J Perinatol 45, 218–223 (2025). https://doi.org/10.1038/s41372-024-02135-7
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41372-024-02135-7
This article is cited by
-
Three studies needed to inform the design of the U-BET (umbilical cord blood for extremely low-gestational-age transfusions) clinical trial
Journal of Perinatology (2026)
-
A prospective randomized pilot trial comparing weekly vs. biweekly Darbepoetin administration to preterm infants
Journal of Perinatology (2025)
-
Identifying barriers to complying with new restrictive NICU transfusion guidelines
Journal of Perinatology (2025)