Abstract
Objective
Evaluate the impact of a sodium (Na) supplementation protocol based upon urine Na concentration on growth parameters and morbidities.
Study design
Retrospective cohort study of infants 260/7-336/7 weeks gestational age (GA) cared for before (2012–15, n = 310) and after (2016–20, n = 382) implementation of the protocol. Within- and between-group changes over time were assessed using repeated measures generalized linear models.
Results
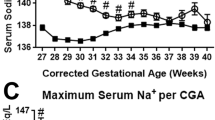
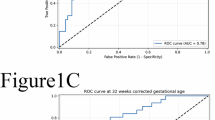
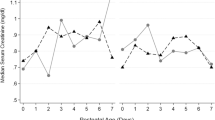
For infants 260/7-296/7 weeks GA, utilization of the protocol was associated with increased mean body weight z-score at 8-weeks postnatal age, increased mean head circumference z-score at 16-weeks postnatal age, and decreased time on mechanical ventilation (all p < 0.02). No impact on growth was identified for infants 30–336/7 weeks GA. Incidences of hypertension, hypernatremia, bronchopulmonary dysplasia, necrotizing enterocolitis, and culture positive sepsis were unaffected by the protocol.
Conclusion
Protocolized Na supplementation is associated with improved growth and reduced time on invasive mechanical ventilation in extremely preterm infants without increasing incidence of morbidities.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The dataset generated and analyzed during the current study is not publicly available due to protection of patient privacy but is available from the corresponding author upon reasonable request.
References
Al-Dahhan J, Haycock GB, Chantler C, Stimmler L. Sodium homeostasis in term and preterm neonates. I. Renal aspects. Arch Dis Child. 1983;58:335–42.
Gubhaju L, Sutherland MR, Horne RS, Medhurst A, Kent AL, Ramsden A, et al. Assessment of renal functional maturation and injury in preterm neonates during the first month of life. Am J Physiol Ren Physiol. 2014;307:F149–158.
Segar JL. Renal adaptive changes and sodium handling in the fetal-to-newborn transition. Semin Fetal Neonatal Med. 2017;22:76–82.
Butterworth SA, Lalari V, Dheensaw K. Evaluation of sodium deficit in infants undergoing intestinal surgery. J Pediatr Surg. 2014;49:736–40.
Mansour F, Petersen D, De Coppi P, Eaton S. Effect of sodium deficiency on growth of surgical infants: a retrospective observational study. Pediatr Surg Int. 2014;30:1279–84.
Knepper C, Ellemunter H, Eder J, Niedermayr K, Haerter B, Hofer P, et al. Low sodium status in cystic fibrosis-as assessed by calculating fractional Na(+) excretion-is associated with decreased growth parameters. J Cyst Fibros. 2016;15:400–5.
Coates AJ, Crofton PM, Marshall T. Evaluation of salt supplementation in CF infants. J Cyst Fibros. 2009;8:382–5.
Ehrenkranz RA, Dusick AM, Vohr BR, Wright LL, Wrage LA, Poole WK. Growth in the neonatal intensive care unit influences neurodevelopmental and growth outcomes of extremely low birth weight infants. Pediatrics. 2006;117:1253–61.
Sammallahti S, Kajantie E, Matinolli HM, Pyhälä R, Lahti J, Heinonen K, et al. Nutrition after preterm birth and adult neurocognitive outcomes. PLoS One. 2017;12:e0185632.
Franz AR, Pohlandt F, Bode H, Mihatsch WA, Sander S, Kron M, et al. Intrauterine, early neonatal, and postdischarge growth and neurodevelopmental outcome at 5.4 years in extremely preterm infants after intensive neonatal nutritional support. Pediatrics. 2009;123:e101–9.
Kleinman RE, Greer FR. American Academy of Pediatrics Committee on Nutrition Pediatric Nutrition. 8th edition. Itasca, IL: American Academy of Pediatrics; 2020.
Isemann B, Mueller EW, Narendran V, Akinbi H. Impact of Early Sodium Supplementation on Hyponatremia and Growth in Premature Infants: A Randomized Controlled Trial. J Parenter Enter Nutr. 2016;40:342–9.
Segar DE, Segar EK, Harshman LA, Dagle JM, Carlson SJ, Segar JL. Physiological Approach to Sodium Supplementation in Preterm Infants. Am J Perinatol. 2018;35:994–1000.
Segar JL, Grobe CC, Grobe JL. Maturational changes in sodium metabolism in periviable infants. Pediatr Nephrol. 2021;36:3693–8.
Diller N, Osborn DA, Birch P. Higher versus lower sodium intake for preterm infants. Cochrane Database Syst Rev. 2023;10:CD012642.
Embleton ND, Jennifer Moltu S, Lapillonne A, van den Akker CHP, Carnielli V, Fusch C, et al. Enteral Nutrition in Preterm Infants (2022): A Position Paper From the ESPGHAN Committee on Nutrition and Invited Experts. J Pediatr Gastroenterol Nutr. 2023;76:248–68.
Fine BP, Ty A, Lestrange N, Levine OR. Sodium deprivation growth failure in the rat: alterations in tissue composition and fluid spaces. J Nutr. 1987;117:1623–8.
Sam R, Feizi I. Understanding hypernatremia. Am J Nephrol. 2012;36:97–104.
Rohrscheib M, Sam R, Raj DS, Argyropoulos CP, Unruh ML, Lew SQ, et al. Edelman Revisited: Concepts, Achievements, and Challenges. Front Med (Lausanne). 2022;8:808765.
Elgin TG, Berger JN, Thomas BA, Colaizy TT, Klein JM. Ventilator Management in Extremely Preterm Infants. Neoreviews. 2022;23(Oct):e661–e676. https://doi.org/10.1542/neo.23-10-e661.
Fenton TR, Nasser R, Eliasziw M, Kim JH, Bilan D, Sauve R. Validating the weight gain of preterm infants between the reference growth curve of the fetus and the term infant. BMC Pediatr. 2013;13:92.
Fenton TR, Kim JH. A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatrics. 2013;13:59.
Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001;163:1723–9.
Walsh MC, Kliegman RM. Necrotizing enterocolitis: treatment based on staging criteria. Pediatr Clin North Am. 1986;33:179–201.
Ayisi RK, Mbiti MJ, Musoke RN, Orinda DA. Sodium supplementation in very low birth weight infants fed on their own mothers milk I: Effects on sodium homeostasis. East Afr Med J. 1992;69(Oct):591–5.
Petersen RY, Clermont D, Williams HL, Buchanan P, Hillman NH. Oral sodium supplementation on growth and hypertension in preterm infants: an observational cohort study. J Perinatol. 2024;44:1515–22.
Griffin IJ, Tancredi DJ, Bertino E, Lee HC, Profit J. Postnatal growth failure in very low birthweight infants born between 2005 and 2012. Arch Dis Child Fetal Neonatal Ed. 2016;101:F50–55.
Ziegler AA, Lawton SBR, Grobe CC, Reho JJ, Freudinger BP, Burnett CML, et al. Early-life sodium deprivation programs long-term changes in ingestive behaviors and energy expenditure in C57BL/6J mice. Am J Physiol Regul Integr Comp Physiol. 2023;325:R576–R592.
Williams WJ, Schneider SM, Gretebeck RJ, Lane HW, Stuart CA, Whitson PA. Effect of dietary sodium on fluid/electrolyte regulation during bed rest. Aviat Space Environ Med. 2003;74:37–46.
Raghuram K, Yang J, Church PT, Ciela Z, Synnes A, Mukerji A, et al. Head Growth Trajectory and Neurodevelopmental Outcomes in Preterm Neonates. Pediatrics. 2017;140:e20170216.
Gattineni J, Baum M. Developmental changes in renal tubular transport-an overview. Pediatr Nephrol. 2015;30:2085–98.
Bartoszewski R, Matalon S, Collawn JF. Ion channels of the lung and their role in disease pathogenesis. Am J Physiol Lung Cell Mol Physiol. 2017;313:L859–L872.
Iwamoto LM, Fujiwara N, Nakamura KT, Wada RK. Na-K-2Cl cotransporter inhibition impairs human lung cellular proliferation. Am J Physiol Lung Cell Mol Physiol. 2004;287:L510–514.
Panet R, Eliash M, Pick M, Atlan H. Na(+)/K(+)/Cl(-) cotransporter activates mitogen-activated protein kinase in fibroblasts and lymphocytes. J Cell Physiol. 2002;190:227–37.
Xie L, Luo X, Li B, Du L, Wang Z, Liu Y, et al. Impact of Changes in Early Respiratory Support Management on Respiratory Outcomes of Preterm Infants. Respir Care. 2022;67:1310–9.
Afsar B, Kuwabara M, Ortiz A, Yerlikaya A, Siriopol D, Covic A, et al. Salt Intake and Immunity. Hypertension. 2018;72:19–23.
Li X, Alu A, Wei Y, Wei X, Luo M. The modulatory effect of high salt on immune cells and related diseases. Cell Prolif. 2022;55:e13250.
Vanpée M, Herin P, Broberger U, Aperia A. Sodium supplementation optimizes weight gain in preterm infants. Acta Paediatr. 1995;84:1312–4.
Al-Dahhan J, Haycock GB, Nichol B, Chantler C, Stimmler L. Sodium homeostasis in term and preterm neonates. III. Effect of salt supplementation. Arch Dis Child. 1984;59:945–50.
Al-Dahhan J, Jannoun L, Haycock GB. Effect of salt supplementation of newborn premature infants on neurodevelopmental outcome at 10-13 years of age. Arch Dis Child Fetal Neonatal Ed. 2002;86:F120–123.
Edwards EM, Greenberg LT, Ehret DEY, Lorch SA, Horbar JD. Discharge Age and Weight for Very Preterm Infants: 2005–18. Pediatrics. 2021;147(Feb):e2020016006.
Yeung T, Rios JD, Beltempo M, Khurshid F, Toye J, Ojah C, et al. The Trend in Costs of Tertiary-Level Neonatal Intensive Care for Neonates Born Preterm at 220/7-286/7 Weeks of Gestation from 2010 to 2019 in Canada. J Pediatr. 2022;245:72–80.e6.
Funding
L.H. receives support from NIH/NIDDK R01DK128835. E.Steinbach receives support from the NIH/NIDDK T32DK007690-29. J.S. receives support from NIH/NIDDK R01DK133197 and NIH/NIDDK R01DK133121. P.T.E. and L.W. receive support from the NIH CTSA program grant UM1TR004403. This content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Contributions
E. Stalter, S.V., E. Steinbach, L.H., and J.S. conceptualized and designed the current study. E. Stalter, S.V., and E. Steinbach were involved in data curation, and P.T.E. and L.W. were involved in the analysis and interpretation of data. J.D., J.S. and L.H. conceptualized the original protocol. All authors contributed to the critical review of this work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
All methods were performed in accordance with relevant guidelines and regulations. Review of patient data was approved with waived consent by the University of Iowa Institutional Review Board (202203591) due to the retrospective nature of the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Stalter, E.J., Verhofste, S.L., Dagle, J.M. et al. Somatic growth outcomes in response to an individualized neonatal sodium supplementation protocol. J Perinatol 45, 305–311 (2025). https://doi.org/10.1038/s41372-024-02141-9
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41372-024-02141-9
This article is cited by
-
A pinch of salt to enhance preemie growth?
Journal of Perinatology (2025)
-
Maternal low sodium intake and early postnatal diuretics program metabolic and ventilatory dysfunction in mice
Pediatric Research (2025)