Abstract
Objective
To determine if a novel CPAP system is associated with physiologic improvement in premature infants in a low resource setting and if the introduction of blended oxygen would reduce FiO2.
Study design
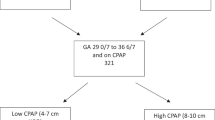
Feasibility study of infants ≤2000 g or ≤32 weeks gestational age with early respiratory distress who were placed on Vayu CPAP with continuous pulse oximetry. Physiologic parameters were recorded prior to initiation and through the first 24 h.
Results
Seventy-six infants of birthweight 1360 ± 324 g and gestational age 31.2 ± 2.5 weeks were included. Compared to baseline, heart rate, respiratory rate, FiO2, and Silverman Anderson score significantly decreased while oxygen saturations significantly increased at one hour with persistence through 24 h.
Conclusion
Utilization of Vayu CPAP in premature infants with respiratory distress was associated with immediate improvement in physiologic parameters. Use of blended oxygen coupled with pulse oximetry facilitates reduction in delivered oxygen.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Fraser J, Walls M, McGuire W. Respiratory complications of preterm birth. BMJ. 2004;329:962–5.
Warren JB, Anderson JM. Core concepts: respiratory distress syndrome. NeoReviews. 2009;10:c351–c61.
Silverman WA, Andersen DH. A controlled clinical trial of effects of water mist on obstructive respiratory signs, death rate and necropsy findings among premature infants. Pediatrics. 1956;17:1–10.
WHO recommendations for care of the preterm or low-birth-weight infant. Geneva: World Health Organization; 2022.
Deuber C, Terhaar M. Hyperoxia in very preterm infants a systematic review of the literature. J Perinat Neonatal Nurs. 2011;25:268–74.
Carlo WA, Finer NN, Walsh MC, Rich W, Gantz MG, Laptook AR, et al. Target ranges of oxygen saturation in extremely preterm infants. N Engl J Med. 2010;362:1959–69.
Askie LM, Darlow BA, Finer N, Schmidt B, Stenson B, Tarnow-Mordi W, et al. Association between oxygen saturation targeting and death or disability in extremely preterm infants in the neonatal oxygenation prospective meta-analysis collaboration. JAMA. 2018;319:2190.
Herrod SK, Stevenson A, Vaucher YE, Lambert SR, Isenberg SJ, Yap VL, et al. Oxygen management among infants in neonatal units in sub-Saharan Africa: a cross-sectional survey. J Perinatol. 2021;41:2631–8.
Tooke L, Ehret DEY, Okolo A, Dlamini-Ngeketo S, Joolay Y, Minto’o S, et al. Limited resources restrict the provision of adequate neonatal respiratory care in the countries of Africa. Acta Paediatr. 2021;111:275–83.
Breathing for Babies: Vayu Global Health Innovations; [November 6, 2023]. Available from: https://vayuinnovations.org/vayu-bcpap-system/.
Dundek ML, Ng EK, Brazil AM, Diblasi RM, Poli JA, Burke TF. Evaluation of a bubble CPAP system for low resource settings. Respir Care. 2021;66:1572–81.
Kawaza K, Machen HE, Brown J, Mwanza Z, Iniguez S, Gest A, et al. Efficacy of a low-cost bubble CPAP system in treatment of respiratory distress in a neonatal ward in Malawi. PLoS ONE. 2014;9:e86327.
Shayo A, Mlay P, Ahn E, Kidanto H, Espiritu M, Perlman J. Early neonatal mortality is modulated by gestational age, birthweight and fetal heart rate abnormalities in the low resource setting in Tanzania – a five year review 2015–2019. BMC Pediatr. 2022;22:313.
Ho JJ, Subramaniam P, Davis PG. Continuous positive airway pressure (CPAP) for respiratory distress in preterm infants (Review). Cochrane Database Syst Rev. 2020;10:CD002271.
Okello F, Egiru E, Ikiror J, Acom L, Loe K, Olupot-Olupot P, et al. Reducing preterm mortality in eastern Uganda: the impact of introducing low-cost bubble CPAP on neonates <1500 g. BMC Pediatr. 2019;19:311.
Rauschendorf P, Bou Saba G, Meara GK, Roodaki N, Conde-Agudelo A, Garcia DEC, et al. Effectiveness of a novel bubble CPAP system for neonatal respiratory support at a referral hospital in the Philippines. Front Pediatrics. 2023;11:1323178.
Tayler A, Ashworth H, Bou Saba G, Wadhwa H, Dundek M, Ng E, et al. Feasibility of a novel ultra-low-cost bubble CPAP (bCPAP) System for neonatal respiratory support at Muhimbili National Hospital, Tanzania. PLoS ONE. 2022;17:e0269147.
Dada S, Ashworth H, Sobitschka A, Raguveer V, Sharma R, Hamilton RL, et al. Experiences with implementation of continuous positive airway pressure for neonates and infants in low-resource settings: a scoping review. PLoS ONE. 2021;16:e0252718.
Poletto S, Trevisanuto D, Ramaswamy VV, Abubacar Seni AH, Ouedraogo P, Dellacà RL, et al. Bubble CPAP respiratory support devices for infants in low-resource settings. Pediatr Pulmonol. 2023;58:643–52.
Acknowledgements
We would like to thank all of the pediatric staff at Kilimanjaro Christian Medical Centre for their dedication and enthusiastic care of the infants in our study.
Funding
This work was supported in part by Bloomberg Philanthropies. Vayu Global Health Innovations donated the continuous positive airway pressure machines. Both Vayu Global Health Innovations and Bloomberg Philanthropies had no involvement in study design, data collection, data analysis, or decision for publication submission.
Author information
Authors and Affiliations
Contributions
Drs. Ahn and Perlman conceptualized and designed the study, supervised study implementation and data collection, were responsible for data curation, performed formal data analysis, and drafted the initial manuscript. Drs. Mselle and Shayo and Nurse Sechu assisted with study design, acquisition of data, and manuscript revisions. All authors critically reviewed the manuscript for important intellectual content, revised the manuscript and approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
This project was approved by the KCMC ethics committee (No 2622) and the National Institute of Medical Research (NIMR/HQ/R.8a/Vol.1X/4561) in Tanzania and included a data transfer agreement. All methods were performed in accordance with the relevant guidelines and regulations. Informed consent was obtained from the parents.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ahn, E., Shayo, A., Mselle, M. et al. Implementation of a novel bubble continuous positive airway pressure system with a blender in preterm infants in a low resource setting. J Perinatol 45, 63–67 (2025). https://doi.org/10.1038/s41372-024-02153-5
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41372-024-02153-5