Abstract
Purpose
Necrotizing enterocolitis (NEC) and spontaneous intestinal perforation (SIP) are severe gastrointestinal complications of prematurity. The clinical presentation and treatment of NEC and SIP (peritoneal drain vs laparotomy) can overlap; however, the pathogenesis is distinct. Therefore, a patient initially treated for SIP can subsequently develop NEC. This phenomenon has only been described in case reports, and no risk factor evaluation exists. We evaluate clinical characteristics, risk factors, and outcomes of patients treated for a distinct episode of NEC after SIP.
Methods
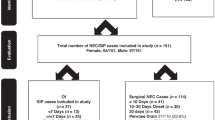
We performed a retrospective review of very low birth weight (<1500 g) neonates who presented with pneumoperitoneum between 07/2004 and 09/2022. Data was obtained from two separate neonatal intensive care units that were part of the same institution. Patients with an initial preoperative, intraoperative, or pathological diagnosis of NEC were excluded. Patients with an intraoperative diagnosis of SIP or preoperative diagnosis of SIP successfully treated with a peritoneal drain (PD) were evaluated. Patients subsequently treated (medically or surgically) for NEC after SIP were then compared to SIP-alone patients. Clinical characteristics included demographics, gestational age (GA), birth weight (BW), perinatal risk factors (chorioamnionitis, steroids, indomethacin), postoperative feeding regimen, and length of stay (LOS) were compared.
Results
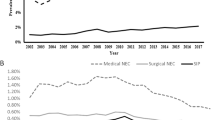
Of the 278 patients included, 31 (11.2%) patients had NEC after SIP. There was no difference in GA (25 weeks vs 25 weeks, p = 0.933) or BW (760 g vs 735 g, p = 0.370) between NEC after SIP vs SIP alone cohorts, respectively. Twenty (64%) of NEC after-SIP patients were previously treated with LP. NEC after SIP occurred with a median onset of 56 days. Pneumatosis was the most frequent (81%) presenting symptom and 12 (39%) patients had hematochezia. Four (12.9%) patients required LP for NEC and all had NEC intraoperatively and on pathology. A majority (77.4%) of patients were on breast milk (BM) at time of NEC diagnosis. NEC after SIP patients had lower maternal age at delivery (29.0 vs 25.0, p = 0.055) and the incidence of NEC after LP (primary or failed drain) was higher than PD alone (16.7% vs 6.2%, p = 0.007). NEC after SIP patients had longer LOS (135 vs 81, p < 0.001).
Conclusion
We report an 11.2% incidence of NEC at a median of 56 days following successful treatment of SIP, resulting in increased LOS. SIP patients are a high-risk cohort and protocols to prevent this phenomenon should be investigated.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
All data generated or analyzed during this study are included in this published article.
References
Neu J, Walker WA. Necrotizing enterocolitis. N Engl J Med. 2011;364:255–64.
Lin PW, Stoll BJ. Necrotising enterocolitis. Lancet. 2006;368:1271–83.
Swanson JR, Hair A, Clark RH, Gordon PV. Spontaneous intestinal perforation (SIP) will soon become the most common form of surgical bowel disease in the extremely low birth weight (ELBW) infant. J Perinatol. 2022;42:423–9.
Rausch LA, Hanna DN, Patel A, Blakely ML. Review of necrotizing enterocolitis and spontaneous intestinal perforation clinical presentation, treatment, and outcomes. Clin Perinatol. 2022;49:955–64.
Lopez CM, Sampah MES, Duess JW, Ishiyama A, Ahmad R, Sodhi CP, et al. Models of necrotizing enterocolitis. Semin Perinatol. 2023;47:151695.
Rose AT, Patel RM. A critical analysis of risk factors for necrotizing enterocolitis. Semin Fetal Neonatal Med. 2018;23:374–9.
Alganabi M, Lee C, Bindi E, Li B, Pierro A. Recent advances in understanding necrotizing enterocolitis. F1000Res. 2019;8:F1000 Faculty Rev-107.
Boston VE. Necrotising enterocolitis and localised intestinal perforation: different diseases or ends of a spectrum of pathology. Pediatr Surg Int. 2006;22:477–84.
Blakely ML, Tyson JE, Lally KP, Hintz SR, Eggleston B, Stevenson DK, et al. Initial laparotomy versus peritoneal drainage in extremely low birthweight infants with surgical necrotizing enterocolitis or isolated intestinal perforation: a multicenter randomized clinical trial. Ann Surg. 2021;274:e370–80.
Patel RM, Ferguson J, McElroy SJ, Khashu M, Caplan MS. Defining necrotizing enterocolitis: current difficulties and future opportunities. Pediatr Res. 2020;88:10–15.
Hwang H, Murphy JJ, Gow KW, Magee JF, Bekhit E, Jamieson D. Are localized intestinal perforations distinct from necrotizing enterocolitis? J Pediatr Surg. 2003;38:763–7.
Tam AL, Camberos A, Applebaum H. Surgical decision making in necrotizing enterocolitis and focal intestinal perforation: predictive value of radiologic findings. J Pediatr Surg. 2002;37:1688–91.
Blakely ML, Lally KP, McDonald S, Brown RL, Barnhart DC, Ricketts RR, et al. Postoperative outcomes of extremely low birth-weight infants with necrotizing enterocolitis or isolated intestinal perforation: a prospective cohort study by the NICHD Neonatal Research Network. Ann Surg. 2005;241:984–9.
Lure AC, Du X, Black EW, Irons R, Lemas DJ, Taylor JA, et al. Using machine learning analysis to assist in differentiating between necrotizing enterocolitis and spontaneous intestinal perforation: a novel predictive analytic tool. J Pediatr Surg. 2021;56:1703–10.
Rivero E, Javed F, Manzar S, Bhat R. Laparotomy or peritoneal drainage in preterm infants with spontaneous intestinal perforation or surgical necrotizing enterocolitis? J Perinatol. 2024;44:146–50.
Keane OA, Dantes G, Dutreuil VL, Do L, Rumbika S, Sylvestre PB, et al. Comparison of preoperative and intraoperative surgeon diagnosis and pathologic findings in spontaneous intestinal perforation vs necrotizing enterocolitis. J Perinatol. 2024;44:568–74.
Meyer CL, Payne NR, Roback SA. Spontaneous, isolated intestinal perforations in neonates with birth weight less than 1000 g not associated with necrotizing enterocolitis. J Pediatr Surg. 1991;26:714–7.
Buchheit JQ, Stewart DL. Clinical comparison of localized intestinal perforation and necrotizing enterocolitis in neonates. Pediatrics. 1994;93:32–36.
Blakely ML, Tyson JE, Lally KP, McDonald S, Stoll BJ, Stevenson DK, et al. Laparotomy versus peritoneal drainage for necrotizing enterocolitis or isolated intestinal perforation in extremely low birth weight infants: outcomes through 18 months adjusted age. Pediatrics. 2006;117:e680–687.
Ibrahim AHM, Hader HA, Alsherbiny H, Hussein MRA, Khan SA. Spontaneous intestinal perforation followed by necrotizing enterocolitis in an extremely low birth weight neonate: case report and review of the literature. Ann Pediatr Surg. 2020;16:20.
Velazco CS, Fullerton BS, Hong CR, Morrow KA, Edwards EM, Soll RF. et al. Morbidity and mortality among ‘big’ babies who develop necrotizing enterocolitis: a prospective multicenter cohort analysis. J Pediatr Surg. 2017;S0022-3468:30650–4.
Motta C, Scott W, Mahony L, Koch J, Wyckoff M, Reisch J, et al. The association of congenital heart disease with necrotizing enterocolitis in preterm infants: a birth cohort study. J Perinatol. 2015;35:949–53.
Walsh MC, Kliegman RM. Necrotizing enterocolitis: treatment based on staging criteria. Pediatr Clin N Am. 1986;33:179–201.
Gordon PV, Clark R, Swanson JR, Spitzer A. Can a national dataset generate a nomogram for necrotizing enterocolitis onset? J Perinatol. 2014;34:732–5.
Patel AL, Panagos PG, Silvestri JM. Reducing incidence of necrotizing enterocolitis. Clin Perinatol. 2017;44:683–700.
Horbar JD, Edwards EM, Greenberg LT, Morrow KA, Soll RF, Buus-Frank ME, et al. Variation in performance of neonatal intensive care units in the United States. JAMA Pediatr. 2017;171:e164396.
Kelleher ST, McMahon CJ, James A. Necrotizing enterocolitis in children with congenital heart disease: a literature review. Pediatr Cardiol. 2021;42:1688–99.
Cognata A, Kataria-Hale J, Griffiths P, Maskatia S, Rios D, O’Donnell A, et al. Human milk use in the preoperative period is associated with a lower risk for necrotizing enterocolitis in neonates with complex congenital heart disease. J Pediatr. 2019;215:11–16.e2.
Fatemizadeh R, Mandal S, Gollins L, Shah S, Premkumar M, Hair A. Incidence of spontaneous intestinal perforations exceeds necrotizing enterocolitis in extremely low birth weight infants fed an exclusive human milk-based diet: a single center experience. J Pediatr Surg. 2021;56:1051–6.
Fisher JG, Jones BA, Gutierrez IM, Hull MA, Kang KH, Kenny M, et al. Mortality associated with laparotomy-confirmed neonatal spontaneous intestinal perforation: a prospective 5-year multicenter analysis. J Pediatr Surg. 2014;49:1215–9.
Culbreath K, Keefe G, Edwards EM, Morrow KA, Soll RF, Jaksic T, et al. Morbidity associated with laparotomy-confirmed spontaneous intestinal perforation: A prospective multicenter analysis. J Pediatr Surg. 2022;57:981–5.
González-Rivera R, Culverhouse RC, Hamvas A, Tarr PI, Warner BB. The age of necrotizing enterocolitis onset: an application of Sartwell’s incubation period model. J Perinatol. 2011;31:519–23.
Jakaitis BM, Bhatia AM. Definitive peritoneal drainage in the extremely low birth weight infant with spontaneous intestinal perforation: predictors and hospital outcomes. J Perinatol. 2015;35:607–11.
Javidi D, Wang Z, Rajasekaran S, Hussain N. Temporal and seasonal variations in incidence of stage II and III NEC-a 28-year epidemiologic study from tertiary NICUs in Connecticut, USA. J Perinatol. 2021;41:1100–9.
Gephart SM, Gordon PV, Penn AH, Gregory KE, Swanson JR, Maheshwari A, et al. Changing the paradigm of defining, detecting, and diagnosing NEC: Perspectives on Bell’s stages and biomarkers for NEC. Semin Pediatr Surg. 2018;27:3–10.
Lueschow SR, Boly TJ, Jasper E, Patel RM, McElroy SJ. Correction: a critical evaluation of current definitions of necrotizing enterocolitis. Pediatr Res. 2022;91:711.
Elgendy MM, Othman HF, Heis F, Qattea I, Aly H. Spontaneous intestinal perforation in premature infants: a national study. J Perinatol. 2021;41:1122–8.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation and data collection were performed by GD, OK, LD, and SR. Data analysis was performed by ZH. The first draft of the manuscript was written by GD and OK with revisions made by AB. All authors commented on and provided revisions to previous versions of the manuscript. All authors read and approved the final manuscript as submitted.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was approved by Children’s Health Care of Atlanta Institutional Review Board (#00001764). Due to the nature of the study and impracticality, individual informed consent was waived. All methods were performed in accordance with the relevant guidelines and regulations. This study was performed in accordance with the Declaration of Helsinki.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dantes, G., Keane, O.A., Raikot, S. et al. Necrotizing enterocolitis following spontaneous intestinal perforation in very low birth weight neonates. J Perinatol 45, 642–649 (2025). https://doi.org/10.1038/s41372-024-02155-3
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41372-024-02155-3