Abstract
Objective
To study the mechanistic role of neonatal morbidities on language performance in extremely preterm (EP) infants.
Study design
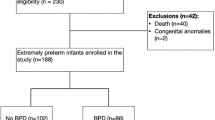
We conducted secondary analyses on EP infants born at a single tertiary care center, investigating whether neonatal morbidities mediated associations between gestational age and language performance at 18–26 months corrected age.
Results
Infants born at 25–26 weeks (n = 298) outperformed those born at 22–24 weeks (n = 177) in expressive communication, receptive communication, composite language, and cognition. Retinopathy of prematurity (ROP), grade 2/3 bronchopulmonary dysplasia (BPD), and cognition partially explained gestational age effects on expressive and receptive communication. In the final sequential path models, infants born 22–24 weeks gestation were more likely to be diagnosed with grade 2/3 BPD, which was linked to diminished cognitive skills, and reduced language skills.
Conclusion
Families of EP infants born under 25 weeks or with ROP and/or grade 2/3 BPD should be counseled about higher language impairment risk and receive proactive intervention.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The dataset is available in NICHD DASH (https://dash.nichd.nih.gov/) from the corresponding author on reasonable request.
References
Ehret DEY, Edwards EM, Greenberg LT, Bernstein IM, Buzas JS, Soll RF, et al. Association of antenatal steroid exposure with survival among infants receiving postnatal life support at 22 to 25 weeks’ gestation. JAMA Netw Open. 2018;1:e183235.
Venkatesan T, Rees P, Gardiner J, Battersby C, Purkayastha M, Gale C, et al. National trends in preterm infant mortality in the United States by race and socioeconomic status, 1995–2020. JAMA Pediatr. 2023;177:1085.
Serenius F, Källén K, Blennow M, Ewald U, Fellman V, Holmström G, et al. Neurodevelopmental outcome in extremely preterm infants at 2.5 years after active perinatal care in Sweden. JAMA Netw Open. 2013;309:1810–20.
Ibrahim J, Mir I, Chalak L. Brain imaging in preterm infants <32 weeks gestation: a clinical review and algorithm for the use of cranial ultrasound and qualitative brain MRI. Pediatr Res. 2018;84:799–806.
Hintz SR, Kendrick DE, Wilson-Costello DE, Das A, Bell E, Vohr B, et al. Early-childhood neurodevelopmental outcomes are not improving for infants born at <25 weeks’ gestational age. Pediatrics. 2011;127:62–70.
Gargus RA, Vohr BR, Tyson JE, High P, Higgins RD, Wrage L, et al. Unimpaired outcomes for extremely low birth weight infants at 18 to 22 months. Pediatrics. 2009;124:112–21.
Vohr BR, Wright LL, Poole WK, McDonald SA. for the NICHD Neonatal Research Network Follow-up Study. Neurodevelopmental outcomes of extremely low birth weight infants <32 weeks’ gestation between 1993 and 1998. Pediatrics. 2005;116:635–43.
Gómez E, Strasser K. Language and socioemotional development in early childhood: the role of conversational turns. Dev Sci. 2021;24. https://doi.org/10.1111/desc.13109
Adams KA, Marchman VA, Loi EC, Ashland MD, Fernald A, Feldman HM. Caregiver talk and medical risk as predictors of language outcomes in full term and preterm toddlers. Child Dev. 2018;89:1674–90.
Borchers LR, Bruckert L, Travis KE, Dodson CK, Loe IM, Marchman VA, et al. Predicting text reading skills at age 8 years in children born preterm and at term. Early Hum Dev. 2019;130:80–6.
Rose SA, Feldman JF, Jankowski JJ. A cognitive approach to the development of early language. Child Dev. 2009;80:134–50.
Wolke D. Language problems in neonatal at risk children: towards an understanding of developmental mechanisms. Acta Paediatr. 1999;88:488–90.
Wolke D, Samara M, Bracewell M, Marlow N. Specific language difficulties and school achievement in children born at 25 weeks of gestation or less. J Pediatr. 2008;152:256–62.e1.
Barre N, Morgan A, Doyle LW, Anderson PJ. Language abilities in children who were very preterm and/or very low birth weight: a meta-analysis. J Pediatr. 2011;158:766–74.e1.
van Noort-van der Spek IL, Franken MCJP, Weisglas-Kuperus N. Language functions in preterm-born children: a systematic review and meta-analysis. Pediatrics. 2012;129:745–54.
Foster-Cohen S, Edgin JO, Champion PR, Woodward LJ. Early delayed language development in very preterm infants: evidence from the MacArthur-Bates CDI. J Child Lang. 2007;34:655–75.
Landry SH, Chapieski L, Fletcher JM, Denson S. Three-year outcomes for low birth weight infants: differential effects of early medical complications. J Pediatr Psychol. 1988;13:317–27.
Kaushal M, Razak A, Patel W, Pullattayil AK, Kaushal A. Neurodevelopmental outcomes following bevacizumab treatment for retinopathy of prematurity: a systematic review and meta-analysis. J Perinatol. 2021;41:1225–35.
Msall ME, Phelps DL, DiGaudio KM, Dobson V, Tung B, McClead RE, et al. Severity of neonatal retinopathy of prematurity is predictive of neurodevelopmental functional outcome at age 5.5 years. Pediatrics. 2000;106:998–1005.
Short EJ, Klein NK, Lewis BA, Fulton S, Eisengart S, Kercsmar C, et al. Cognitive and academic consequences of bronchopulmonary dysplasia and very low birth weight: 8-year-old outcomes. Pediatrics. 2003;112:e359–59.
Watkins PL, Dagle JM, Bell EF, Colaizy TT. Outcomes at 18 to 22 months of corrected age for infants born at 22 to 25 weeks of gestation in a center practicing active management. J Pediatr. 2020;217:52–8.e1.
Albers CA, Grieve AJ. Test Review: Bayley, N. (2006). Bayley Scales of Infant and Toddler Development–Third Edition. San Antonio, TX: Harcourt Assessment. J Psychoeduc Assess. 2007;25:180–90.
Johnson S, Moore T, Marlow N. Using the Bayley-III to assess neurodevelopmental delay: which cut-off should be used? Pediatr Res. 2014;75:670–4.
Vassar R, Schadl K, Cahill-Rowley K, Yeom K, Stevenson D, Rose J. Neonatal brain microstructure and machine-learning-based prediction of early language development in children born very preterm. Pediatr Neurol. 2020;108:86–92.
Adams-Chapman I, Heyne RJ, DeMauro SB, Duncan AF, Hintz SR, Pappas A, et al. Neurodevelopmental impairment among extremely preterm infants in the neonatal research network. Pediatrics. 2018;141:e20173091.
Bell EF, Hintz SR, Hansen NI, Bann CM, Wyckoff MH, DeMauro SB, et al. Mortality, in-hospital morbidity, care practices, and 2-year outcomes for extremely preterm infants in the US, 2013–2018. JAMA. 2022;327:248.
Venkatesh KK, Lynch CD, Costantine MM, Backes CH, Slaughter JL, Frey HA, et al. Trends in active treatment of live-born neonates between 22 weeks 0 days and 25 weeks 6 days by gestational age and maternal race and ethnicity in the US, 2014 to 2020. JAMA. 2022;328:652.
Gkiougki E, Chatziioannidis I, Pouliakis A, Iacovidou N. Periviable birth: a review of ethical considerations. Hippokratia. 2021;25:1–7.
Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1500 gm. J Pediatr. 1978;92:529–34.
Hamrick SEG, Hansmann G. Patent ductus arteriosus of the preterm infant. Pediatrics. 2010;125:1020–30.
Benitz WE, Committee on Fetus and Newborn, Watterberg KL, Aucott S, Cummings JJ, Eichenwald EC, et al. Patent ductus arteriosus in preterm infants. Pediatrics. 2016;137:e20153730.
Shane AL, Sánchez PJ, Stoll BJ. Neonatal sepsis. Lancet. 2017;390:1770–80.
Wynn JL. Defining neonatal sepsis. Curr Opin Pediatr. 2016;28:135–40.
Lee JS, Polin RA. Treatment and prevention of necrotizing enterocolitis. Semin Neonatol. 2003;8:449–59.
AlFaleh K, Anabrees J. Probiotics for prevention of necrotizing enterocolitis in preterm infants: probiotics for prevention of necrotizing enterocolitis in preterm infants. Evid-Based Child Health Cochrane Rev J. 2014;9:584–671.
Rich BS, Dolgin SE. Necrotizing enterocolitis. Pediatr Rev. 2017;38:552–9.
Jensen EA, Dysart K, Gantz MG, McDonald S, Bamat NA, Keszler M, et al. The diagnosis of bronchopulmonary dysplasia in very preterm infants. An evidence-based approach. Am J Respir Crit Care Med. 2019;200:751–9.
Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations.1986;51:1173.
Reidy N, Morgan A, Thompson DK, Inder TE, Doyle LW, Anderson PJ. Impaired language abilities and white matter abnormalities in children born very preterm and/or very low birth weight. J Pediatr. 2013;162:719–24.
Patra K, Greene M, Patel A, Meier P. Maternal education level predicts cognitive, language, and motor outcome in preterm infants in the second year of life. Am J Perinatol. 2016;33:738–44.
Ko G, Shah P, Lee S, Asztalos E. Impact of maternal education on cognitive and language scores at 18 to 24 months among extremely preterm neonates. Am J Perinatol. 2012;30:723–30.
Sentenac M, Johnson S, Charkaluk ML, Sëppanen AV, Aden U, Cuttini M, et al. Maternal education and language development at 2 years corrected age in children born very preterm: results from a European population-based cohort study. J Epidemiol Community Health. 2020;74:346–53.
Thorpe K. Twin children’s language development. Early Hum Dev. 2006;82:387–95.
Räikkönen K, Gissler M, Tapiainen T, Kajantie E. Associations between maternal antenatal corticosteroid treatment and psychological developmental and neurosensory disorders in children. JAMA Netw Open. 2022;5:e2228518.
Rosseel Y. lavaan: an R package for structural equation modeling. J Stat Softw. 2012;48:1–36.
Natarajan G, Pappas A, Shankaran S, Kendrick DE, Das A, Higgins RD, et al. Outcomes of extremely low birth weight infants with bronchopulmonary dysplasia: impact of the physiologic definition. Early Hum Dev. 2012;88:509–15.
Singer LT, Siegel AC, Lewis B, Hawkins S, Yamashita T, Baley J. Preschool language outcomes of children with history of bronchopulmonary dysplasia and very low birth weight. J Dev Behav Pediatr. 2001;22:19–26.
Lewis BA, Singer LT, Fulton S, Salvator A, Short EJ, Klein N, et al. Speech and language outcomes of children with bronchopulmonary dysplasia. J Commun Disord. 2002;35:393–406.
Rinaldi S, Caselli MC, Cofelice V, D’Amico S, De Cagno AG, Corte GD, et al. Efficacy of the treatment of developmental language disorder: a systematic review. Brain Sci. 2021;11:407.
Ellis EM, Thal DJ. Early language delay and risk for language impairment. Perspect Lang Learn Educ. 2008;15:93–100.
Whitehouse AJO, Robinson M, Zubrick SR. Late talking and the risk for psychosocial problems during childhood and adolescence. Pediatrics. 2011;128:e324–e332.
Pérez-Pereira M. Prevalence of language delay among healthy preterm children, language outcomes and predictive factors. Children. 2021;8:282.
Fagan MK, Montgomery TR. Managing referrals for children with receptive language delay. Clin Pediatr. 2009;48:72–80.
Kline JE, Illapani VSP, He L, Altaye M, Parikh NA. Retinopathy of prematurity and bronchopulmonary dysplasia are independent antecedents of cortical maturational abnormalities in very preterm infants. Sci Rep. 2019;9:19679.
Lee JM, Choi YH, Hong J, Kim NY, Kim EB, Lim JS, et al. Bronchopulmonary dysplasia is associated with altered brain volumes and white matter microstructure in preterm infants. Neonatology. 2019;116:163–70.
Kline JE, Illapani VSP, He L, Altaye M, Logan JW, Parikh NA. Early cortical maturation predicts neurodevelopment in very preterm infants. Arch Dis Child-Fetal Neonatal Ed. 2020;105:460–5.
Back SA, Volpe JJ Chapter 15 - Encephalopathy of Prematurity: Pathophysiology. In: Volpe JJ, Inder TE, Darras BT, et al., eds. Volpe’s Neurology of the Newborn (Sixth Edition). Elsevier; 2018:405–424.e8. https://doi.org/10.1016/B978-0-323-42876-7.00015-6
Grelli KN, Keller RL, Rogers EE, Partridge JC, Xu D, Barkovich AJ, et al. Bronchopulmonary dysplasia precursors influence risk of white matter injury and adverse neurodevelopmental outcome in preterm infants. Pediatr Res. 2021;90:359–65.
Jungner Å, Vallius Kvist S, Romantsik O, Bruschettini M, Ekström C, Bendix I, et al. White matter brain development after exposure to circulating cell-free hemoglobin and hyperoxia in a rat pup model. Dev Neurosci. 2020;41:234–46.
Basu SK, Kapse KJ, Murnick J, Pradhan S, Spoehr E, Zhang A, et al. Impact of bronchopulmonary dysplasia on brain GABA concentrations in preterm infants: Prospective cohort study. Early Hum Dev. 2023;186:105860.
Basu SK, Pradhan S, du Plessis AJ, Ben-Ari Y, Limperopoulos C. GABA and glutamate in the preterm neonatal brain: in-vivo measurement by magnetic resonance spectroscopy. Neuroimage. 2021;238:118215.
Ahn JH, Lee KM, Kim MJ, Park HK, Kim YJ, Ahn SJ, et al. Neurodevelopmental outcomes in very low birthweight infants with retinopathy of prematurity in a nationwide cohort study. Sci Rep. 2022;12:5053.
Brumbaugh JE, Bell EF, Hirsch SC, Crenshaw EG, DeMauro SB, Adams-Chapman IS, et al. Relationships between retinopathy of prematurity without ophthalmologic intervention and neurodevelopment and vision at 2 years. Pediatr Res. Published online October 22, 2021. https://doi.org/10.1038/s41390-021-01778-y
Glass TJA, Chau V, Gardiner J, Foong J, Vinall J, Zwicker JG, et al. Severe retinopathy of prematurity predicts delayed white matter maturation and poorer neurodevelopment. Arch Dis Child Fetal Neonatal Ed. 2017;102:F532–37.
Sveinsdóttir K, Ley D, Hövel H, Fellman V, Hüppi PS, Smith LEH, et al. Relation of retinopathy of prematurity to brain volumes at term equivalent age and developmental outcome at 2 years of corrected age in very preterm infants. Neonatology. 2018;114:46–52.
Guarini A, Sansavini A, Fabbri C, Alessandroni R, Faldella G, Karmiloff-Smith A. Reconsidering the impact of preterm birth on language outcome. Early Hum Dev. 2009;85:639–45.
Schneider W, Wolke D, Schlagmüller M, Meyer R. Pathsways to school achievement in very preterm and full term children. Eur J Psychol Educ. 2004;19:385–406.
Saigal S, Szatmari P, Rosenbaum P, Campbell D, King S. Cognitive abilities and school performance of extremely low birth weight children and matched term control children at age 8 years: a regional study. J Pediatr. 1991;118:751–60.
Mutch L, Leyland A, McGee A. Patterns of neuropsychological function in a low‐birthweight population. Dev Med Child Neurol. 1993;35:943–56.
Nelson PM, Demir-Lira ÖE. Parental cognitive stimulation in preterm-born children’s neurocognitive functioning during the preschool years: a systematic review. Pediatr Res. 2023;94:1284–96.
Acknowledgements
The authors would like to thank the families who participated in the study and the research staff who helped with data collection.
Funding
Paige Nelson was supported by the National Institute of General Medical Science (Grant T32GM108540). The original data collection was funded by the National Institutes of Health, the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) (UG1HD053109).
Author information
Authors and Affiliations
Contributions
PMN and HMH conceptualized and designed the study, guided the statistical analyses, drafted the initial manuscript, and revised subsequent drafts. HMH also oversaw and coordinated data collection. FS contributed to drafting the initial manuscript, and ÖED supported the statistical analyses. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was performed in accordance with the Declaration of Helsinki. The original data collection was reviewed and approved by the Institutional Review Board at the University of Iowa. For this study, the IRB determined that, due to the de-identified nature of the data, further IRB review was not necessary. Informed consent was obtained from all participants.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nelson, P.M., Scheiber, F., Demir-Lira, Ö.E. et al. Early medical risks to language development in extremely preterm infants. J Perinatol 45, 378–385 (2025). https://doi.org/10.1038/s41372-024-02191-z
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41372-024-02191-z