Abstract
Objective
The aim of this study was to examine the predictive value of the lung ultrasound score (LUS) for successful extubation in preterm infants born at ≤25+6 weeks.
Methods
This was a single-center, prospective cohort study. Preterm infants with gestational age (GA) ≤ 25+6 weeks who received invasive mechanical ventilation (IMV) for ≥72 h were included. Lung ultrasound was performed every day. Multivariate logistic regression analysis was used to evaluate factors that predict extubation outcomes.
Results
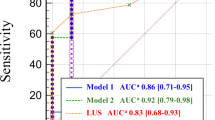
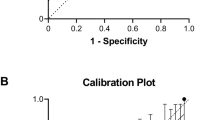
Ninety-three infants with GA ≤ 25+6 weeks were included. The mean GA was 24.5 ± 1.2 weeks. Extubation failure occurred in 55 (59.1%) neonates, and success occurred in 38 (40.9%) neonates. The LUS was significantly lower in the successful group than in the failed group (24.0 ± 2.5 vs. 32.1 ± 3.1 p < 0.001). Logistic regression analysis showed that LUS was an independent predictor of successful extubation (odd ratio 0.15 [95% CI 0.045–0.508], P = 0.002). The area under the receiver operating characteristic curve was 0.98 (p < 0.001) for LUS, and a cutoff value of ≥ 28 had 94.6% sensitivity and 92.7% specificity in detecting extubation failure.
Conclusion
The LUS has good accuracy for predicting successful extubation in extremely preterm infants with GA ≤ 25+6 weeks.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Walsh MC, Morris BH, Wrage LA, Vohr BR, Poole WK, Tyson JE, et al. Extremely low birthweight neonates with protracted ventilation: mortality and 18-month neurodevelopmental outcomes. J Pediatr. 2005;146:798–804. https://doi.org/10.1016/j.jpeds.2005.01.047.
Escobar V, Soares DS, Kreling J, Ferrari LSL, Felcar JM, Camillo CAM, et al. Influence of time under mechanical ventilation on bronchopulmonary dysplasia severity in extremely preterm infants: a pilot study. BMC Pediatr. 2020;20:241 https://doi.org/10.1186/s12887-020-02129-2.
Bose CL, Laughon MM, Allred EN, O’Shea TM, Van Marter LJ, Ehrenkranz RA, et al. Systemic inflammation associated with mechanical ventilation among extremely preterm infants. Cytokine. 2013;61:315–22. https://doi.org/10.1016/j.cyto.2012.10.014.
Bauman NM, Benjamin B. Subglottic ductal cysts in the preterm infant: association with laryngeal intubation trauma. Ann Otol Rhinol Laryngol. 1995;104:963–8. https://doi.org/10.1177/000348949510401209.
da Silva O, Stevens D. Complications of airway management in very-low-birth-weight infants. Biol Neonate. 1999;75:40–5. https://doi.org/10.1159/000014075
Jensen EA, DeMauro SB, Kornhauser M, Aghai ZH, Greenspan JS, Dysart KC. Effects of Multiple Ventilation Courses and Duration of Mechanical Ventilation on Respiratory Outcomes in Extremely Low-Birth-Weight Infants. JAMA Pediatr. 2015;169:1011–7. https://doi.org/10.1001/jamapediatrics.2015.2401.
Chawla S, Natarajan G, Shankaran S, Carper B, Brion LP, Keszler M, et al. Markers of Successful Extubation in Extremely Preterm Infants, and Morbidity After Failed Extubation. J Pediatr. 2017;189:113–119.e2. https://doi.org/10.1016/j.jpeds.2017.04.050.
Manley BJ, Doyle LW, Owen LS, Davis PG. Extubating Extremely Preterm Infants: Predictors of Success and Outcomes following Failure. J Pediatr. 2016;173:45–9. https://doi.org/10.1016/j.jpeds.2016.02.016.
Sant’Anna GM, Keszler M. Weaning infants from mechanical ventilation. Clin Perinatol. 2012;39:543–62. https://doi.org/10.1016/j.clp.2012.06.003.
Mukerji A, Razak A, Aggarwal A, Jacobi E, Musa M, Alwahab Z, et al. Early versus delayed extubation in extremely preterm neonates: a prospective cohort study. J Perinatol. 2020;40:118–23. https://doi.org/10.1038/s41372-019-0495-6.
Spaggiari E, Amato M, Ricca OA, Corradini Zini L, Bianchedi I, Lugli L, et al. Can Fraction of Inspired Oxygen Predict Extubation Failure in Preterm Infants? Child (Basel). 2022;9:30 https://doi.org/10.3390/children9010030.
Gupta D, Greenberg RG, Sharma A, Natarajan G, Cotten M, Thomas R, et al. A predictive model for extubation readiness in extremely preterm infants. J Perinatol. 2019;39:1663–9. https://doi.org/10.1038/s41372-019-0475-x.
Shalish W, Kanbar LJ, Rao S, Robles-Rubio CA, Kovacs L, Chawla S, et al. Prediction of Extubation readiness in extremely preterm infants by the automated analysis of cardiorespiratory behavior: study protocol. BMC Pediatr. 2017;17:167 https://doi.org/10.1186/s12887-017-0911-z.
Shalish W, Latremouille S, Papenburg J, Sant’Anna GM. Predictors of extubation readiness in preterm infants: a systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed. 2019;104:F89–F97. https://doi.org/10.1136/archdischild-2017-313878.
Davis KamlinCO, Morley PG. CJ. Predicting successful extubation of very low birthweight infants. Arch Dis Child Fetal Neonatal Ed. 2006;91:F180–3. https://doi.org/10.1136/adc.2005.081083.
Chawla S, Natarajan G, Gelmini M, Kazzi SN. Role of spontaneous breathing trial in predicting successful extubation in premature infants. Pediatr Pulmonol. 2013;48:443–8. https://doi.org/10.1002/ppul.22623.
Singh Y, Tissot C, Fraga MV, Yousef N, Cortes RG, Lopez J, et al. International evidence-based guidelines on Point of Care Ultrasound (POCUS) for critically ill neonates and children issued by the POCUS Working Group of the European Society of Paediatric and Neonatal Intensive Care (ESPNIC). Crit Care. 2020;24:65 https://doi.org/10.1186/s13054-020-2787-9.
Brat R, Yousef N, Klifa R, Reynaud S, Shankar Aguilera S, De Luca D. Lung Ultrasonography Score to Evaluate Oxygenation and Surfactant Need in Neonates Treated With Continuous Positive Airway Pressure. JAMA Pediatr. 2015;169:e151797 https://doi.org/10.1001/jamapediatrics.2015.1797.
Soliman RM, Elsayed Y, Said RN, Abdulbaqi AM, Hashem RH, Aly H. Prediction of extubation readiness using lung ultrasound in preterm infants. Pediatr Pulmonol. 2021;56:2073–80. https://doi.org/10.1002/ppul.25383.
El Amrousy D, Elgendy M, Eltomey M, Elmashad AE. Value of lung ultrasonography to predict weaning success in ventilated neonates. Pediatr Pulmonol. 2020;55:2452–6. https://doi.org/10.1002/ppul.24934.
Zong H, Huang Z, Fu Y, Chen X, Yu Y, Huang Y, et al. Lung ultrasound score as a tool to predict severity of bronchopulmonary dysplasia in neonates born ≤25 weeks of gestational age. J Perinatol. 2024;44:273–9. https://doi.org/10.1038/s41372-023-01811-4.
Mohsen N, Nasef N, Ghanem M, Yeung T, Deekonda V, Ma C, et al. Accuracy of lung and diaphragm ultrasound in predicting successful extubation in extremely preterm infants: A prospective observational study. Pediatr Pulmonol. 2023;58:530–9. https://doi.org/10.1002/ppul.26223.
Tenza-Lozano E, Llamas-Alvarez A, Jaimez-Navarro E, Fernández-Sánchez J. Lung and diaphragm ultrasound as predictors of success in weaning from mechanical ventilation. Crit Ultrasound J. 2018;10:12 https://doi.org/10.1186/s13089-018-0094-3.
Shalish W, Kanbar L, Keszler M, Chawla S, Kovacs L, Rao S, et al. Patterns of reintubation in extremely preterm infants: a longitudinal cohort study. Pediatr Res. 2018;83:969–75. https://doi.org/10.1038/pr.2017.330.
Ammari A, Suri M, Milisavljevic V, Sahni R, Bateman D, Sanocka U, et al. Variables associated with the early failure of nasal CPAP in very low birth weight infants. J Pediatr. 2005;147:341–7. https://doi.org/10.1016/j.jpeds.2005.04.062.
Kidman AM, Manley BJ, Boland RA, Davis PG, Bhatia R. Predictors and outcomes of extubation failure in extremely preterm infants. J Paediatr Child Health. 2021;57:913–9. https://doi.org/10.1111/jpc.15356.
Ohnstad MO, Stensvold HJ, Pripp AH, Tvedt CR, Jelsness-Jørgensen LP, Astrup H, et al. Norwegian Neonatal Network. Predictors of extubation success: a population-based study of neonates below a gestational age of 26 weeks. BMJ Paediatr Open. 2022;6:e001542 https://doi.org/10.1136/bmjpo-2022-001542.
Eltomey MA, Shehata AH, Nassar MAE, Elmashad AEM. Can lung ultrasound assist in the decision of weaning mechanically ventilated neonates? Egypt J Radio Nucl Med. 2019;50:47 https://doi.org/10.1186/s43055-019-0055-2
Jiang QX, Shi LJ, Shen LY, Li XQ, Huang RS, Chen LJ, et al. Application Value of a New Lung Ultrasound Scoring Method in Neonatal Respiratory Distress Syndrome Treatment. Ultrasound Med Biol. 2022;48:275–82. https://doi.org/10.1016/j.ultrasmedbio.2021.10.009.
Liang Z, Meng Q, You C, Wu B, Li X, Wu Q. Roles of Lung Ultrasound Score in the Extubation Failure From Mechanical Ventilation Among Premature Infants With Neonatal Respiratory Distress Syndrome. Front Pediatr. 2021;9:709160 https://doi.org/10.3389/fped.2021.709160.
Acknowledgements
We would like to thank the staff who participated in this study.
Funding
This study is supported by Shenzhen Science and Technology Program (JCYJ20230807120201004 to H.Z), Shenzhen Fund for Guangdong Provincial Highlevel Clinical Key Specialties (No.SZGSP009), Sanming Project of Medicine in Shenzhen (No.SZSM202211001), Shenzhen Key Laboratory of Maternal and Child Health and Diseases (ZDSYS 20230626091559006).
Author information
Authors and Affiliations
Contributions
Each author made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data. CY conceived and designed the study. BL, YH, YH, HS ZL, JW and QX acquired data and analyzed data. The preliminary draft of the manuscript was prepared by HZ, BL, YH, and CY. All authors gave their approval for the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics statement
This study was performed in line with the principles of the declaration on Helsinki. The study was approved by the ethics committee of the hospital (No. SFYLJ2023048).
Informed consent
The study was approved by the Ethics Committee of the Shenzhen Maternity & Child Healthcare Hospital. and written informed consent was obtained from the parents.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zong, H., Lin, B., Huang, Y. et al. Accuracy of lung ultrasound in predicting successful extubation in preterm infants born ≤ 25 weeks. J Perinatol 45, 830–836 (2025). https://doi.org/10.1038/s41372-024-02206-9
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41372-024-02206-9