Abstract
Objective
To evaluate pre- and post-ductal blood pressure (BP) in preterm infants according to patent ductus arteriosus (PDA) status obtained from targeted neonatal echocardiography (TnECHO).
Study design
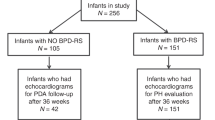
Retrospective cohort study of infants born at 22–28 weeks divided according to three groups: (i) No PDA, (ii) Low volume shunt, (iii) Moderate-high volume shunt. BP parameters, demographics, and clinical characteristics were compared.
Result
A total of 373 TnECHOs were included: 98 no PDA, 152 low volume shunt, and 123 moderate-high volume shunt. TnECHOs with no PDA had higher systolic, diastolic, and mean BP. Diastolic flow reversal in the post-ductal descending aorta was associated with lower post-ductal diastolic (p < 0.001) and mean BP (p < 0.001). Moderate-high volume shunt had higher rates of diastolic hypotension.
Conclusion
BP patterns varied according to PDA status. Post-ductal hypotension was more common with a moderate-high volume shunt. PDA status in this population may be the strongest influencer of BP variability.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Kluckow M. The pathophysiology of low systemic blood flow in the preterm infant. Front Pediatr. 2018;6:29.
Ruoss JL, Bazacliu C, Giesinger RE, McNamara PJ. Patent ductus arteriosus and cerebral, cardiac, and gut hemodynamics in premature neonates. Semin Fetal Neonatal Med. 2020;25:101120.
Seri I. Management of hypotension and low systemic blood flow in the very low birth weight neonate during the first postnatal week. J Perinatol. 2006;26:S8–13.
Laughon M, Bose C, Allred E, O’Shea TM, Van Marter LJ, Bednarek F, et al. Factors associated with treatment for hypotension in extremely low gestational age newborns during the first postnatal week. Pediatrics. 2007;119:273–80.
Munro MJ, Walker AM, Barfield CP. Hypotensive extremely low birth weight infants have reduced cerebral blood flow. Pediatrics. 2004;114:1591–6.
Watkins AM, West CR, Cooke RW. Blood pressure and cerebral haemorrhage and ischaemia in very low birthweight infants. Early Hum Dev. 1989;19:103–10.
Low JA, Froese AB, Galbraith RS, Smith JT, Sauerbrei EE, Derrick EJ. The association between preterm newborn hypotension and hypoxemia and outcome during the first year. Acta Paediatr. 1993;82:433–7.
Seri I. Circulatory support of the sick preterm infant. Semin Neonatol. 2001;6:85–95.
Hamrick SEG, Sallmon H, Rose AT, Porras D, Shelton EL, Reese J, et al. Patent ductus arteriosus of the preterm infant. Pediatrics. 2020;146:e20201209.
Evans N, Moorcraft J. Effect of patency of the ductus arteriosus on blood pressure in very preterm infants. Arch Dis Child. 1992;67:1169–73.
Baumgartner S, Olischar M, Wald M, Werther T, Berger A, Waldhor T, et al. Left ventricular pumping during the transition-adaptation sequence in preterm infants: impact of the patent ductus arteriosus. Pediatr Res. 2018;83:1016–23.
Batton B. Neonatal blood pressure standards: what is “normal”? Clin Perinatol. 2020;47:469–85.
Rios DR, Martins FF, El-Khuffash A, Weisz DE, Giesinger RE, McNamara PJ. Early role of the atrial-level communication in premature infants with patent ductus arteriosus. J Am Soc Echocardiogr. 2021;34:423–32.e421.
Initiative NN. Systolic blood pressure in babies of less than 32 weeks gestation in the first year of life. Northern Neonatal Nursing Initiative. Arch Dis Child Fetal Neonatal Ed. 1999;80:F38–42.
Dionne JM, Abitbol CL, Flynn JT. Hypertension in infancy: diagnosis, management and outcome. Pediatr Nephrol. 2012;27:17–32.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inf. 2009;42:377–81.
Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. The REDCap consortium: Building an international community of software platform partners. J Biomed Inf. 2019;95:103208.
Giesinger RE, McNamara PJ. Hemodynamic instability in the critically ill neonate: an approach to cardiovascular support based on disease pathophysiology. Semin Perinatol. 2016;40:174–88.
Giesinger RE, Rios DR, Chatmethakul T, Bischoff AR, Sandgren JA, Cunningham A, et al. Impact of early hemodynamic screening on extremely preterm outcomes in a high-performance center. Am J Respir Crit Care Med. 2023;208:290–300.
Han UJ, Cho HJ, Cho YK, Choi YY, Ma JS. Change in blood pressure and pulse pressure in preterm infants after treatment of patent ductus arteriosus with indomethacin. Korean Circ J. 2011;41:203–8.
Lubetzky R, Mandel D, Mimouni FB, Diamant S, Birger A, Barak M, et al. Indomethacin-induced early patent ductus arteriosus closure cannot be predicted by a decrease in pulse pressure. Am J Perinatol. 2004;21:257–61.
Zanardo V, Vedovato S, Chiozza L, Faggian D, Favaro F, Trevisanuto D. Pharmacological closure of patent ductus arteriosus: effects on pulse pressure and on endothelin-1 and vasopressin excretion. Am J Perinatol. 2008;25:353–8.
Evans N, Iyer P. Change in blood pressure after treatment of patent ductus arteriosus with indomethacin. Arch Dis Child. 1993;68:584–7.
Funding
The authors have no financial relationships relevant to this article to disclose. NIH and CTSA grant number UM1TR004403 for REDCap use.
Author information
Authors and Affiliations
Contributions
ARB designed the study, performed all echocardiography analyses, wrote the first draft of the manuscript. AAH helped develop the cohort, completed data collection, and wrote the manuscript. PJM provided clinical expertise and oversight, reviewed and revised the manuscript. DRR helped with study design, provided direct supervision throughout the project, and reviewed and revised the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
All methods were performed in accordance with relevant guidelines and regulations. This study was approved by the institutional review board at the University of Iowa (HawkIRB # 201410743). This study received a waiver of consent for participation of all subjects.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bischoff, A.R., Hobson, A.A., McNamara, P.J. et al. Impact of a patent ductus arteriosus on non-invasive pre- and post-ductal blood pressures in extremely preterm infants during the first two postnatal weeks. J Perinatol 45, 326–333 (2025). https://doi.org/10.1038/s41372-025-02223-2
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41372-025-02223-2