Abstract
Objectives
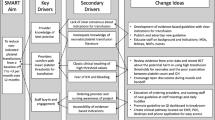
Our NICU transfusion stewardship group proposed new, more restrictive guidelines for red blood cell and platelet transfusions. To evaluate our clinician’s support for these, we conducted a series of structured interviews.
Study design
We presented 11 scenarios involving the new guidelines to each of 24 clinicians. After every scenario we asked whether they would abide by the guideline, and if not, why.
Results
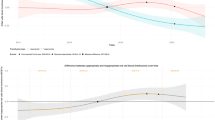
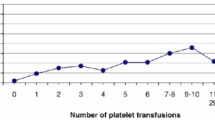
For 88% of scenarios, participants said they supported the guideline and would not transfuse. The most common reasons for wanting to transfuse when the guidelines said not to were; 1) the scenario-patient did not meet the guideline but was “close” and 2) the guideline was insufficiently explicit.
Conclusions
Structured interviews like these can identify barriers to complying with transfusion guidelines and can suggest guideline modifications. Future studies will determine the effect of this discovery process on guideline adherence and patient outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
Inquiries regarding data access can be addressed to the corresponding author.
References
Davenport P, Sola-Visner M. Immunologic effects of red blood cell and platelet transfusions in neonates. Curr Opin Hematol. 2022;29:297–305.
Pellegrino C, Papacci P, Beccia F, et al. Differences in cerebral tissue oxygenation in preterm neonates receiving adult or cord blood red blood cell transfusions. JAMA Netw Open. 2023;6:e2341643.
Christensen RD, Bahr TM, Davenport P, Sola-Visner MC, Ohls RK, Ilstrup SJ, et al. Implementing evidence-based restrictive neonatal intensive care unit platelet transfusion guidelines. J Perinatol. 2024. https://doi.org/10.1038/s41372-024-02050-x.
Bahr TM, Snow GL, Christensen TR, Davenport P, Henry E, Tweddell SM, et al. Can red blood cell and platelet transfusions have a pathogenic role in bronchopulmonary dysplasia? J Pediatr. 2024;265:113836.
Bahr TM, Ohls RK, Henry E, Davenport P, Ilstrup SJ, Kelley WE, et al. The number of blood transfusions received and the incidence and severity of chronic lung disease among NICU patient born >31 weeks gestation. J Perinatol. 2024. https://doi.org/10.1038/s41372-024-02135-7.
Davenport PE, Wood TR, Heagerty PJ, Sola-Visner MC, Juul SE, Patel RM. Platelet transfusion and death or neurodevelopmental impairment in children born extremely preterm. JAMA Netw Open. 2024;7:e2352394.
Kirpalani H, Bell EF, Hintz SR, Tan S, Schmidt B, Chaudhary AS, et al. Eunice Kennedy Shriver NICHD Neonatal Research Network. Higher or lower hemoglobin transfusion thresholds for preterm infants. N. Engl J Med. 2020;383:2639–51.l.
Franz AR, Engel C, Bassler D, Rüdiger M, Thome UH, Maier RF, et al. ETTNO Investigators. Effects of liberal vs restrictive transfusion thresholds on survival and neurocognitive outcomes in extremely low-birth-weight Infants: the ETTNO randomized clinical trial. JAMA. 2020;324:560–70.
Curley A, Stanworth SJ, Willoughby K, Fustolo-Gunnink SF, Venkatesh V, Hudson C, et al. PlaNeT2 MATISSE Collaborators. Randomized trial of platelet-transfusion thresholds in neonates. N Engl J Med. 2019;380:242–51.
Bahr TM, Christensen TR, Henry E, Astin M, Ilstrup SJ, Ohls RK, et al. Platelet transfusions in a multi-neonatal intensive care unit health care organization before and after publication of the PlaNeT-2 clinical trial. J Pediatr. 2023;257:113388.
Scrivens A, Reibel NJ, Heeger L, Stanworth S, Lopriore E, New HV, et al. Neonatal Transfusion Network. Survey of transfusion practices in preterm infants in Europe. Arch Dis Child Fetal Neonatal Ed. 2023;108:360–6.
Francis JJ, Tinmouth A, Stanworth SJ, Grimshaw JM, Johnston M, Hyde C, et al. Using theories of behaviour to understand transfusion prescribing in three clinical contexts in two countries: development work for an implementation trial. Implement Sci. 2009;4:70.
Ma T, Sun Y, Wang Q, Liu F, Hua K, Wang L, et al. Retrospective cohort study of neonatal blood transfusion in China. BMC Pediatr. 2023;23:621.
Use of blood products for elective surgery in 43 European hospitals. The Sanguis Study Group. Transfus Med. 1994;4:251–68.
Rubin R. It takes an average of 17 years for evidence to change practice-the burgeoning field of implementation science seeks to speed things up. JAMA. 2023;329:1333–6.
Chegini A, Jamalian A, Abolhassani MR, Alavi AB. A review of issues and challenges of implementation of patient blood management. Asian J Transfus Sci. 2024;18:115–23.
Kemper AR, Newman TB, Slaughter JL, Maisels MJ, Watchko JF, Downs SM, et al. Clinical Practice Guideline Revision: Management of Hyperbilirubinemia in the Newborn Infant 35 or More Weeks of Gestation. Pediatrics. 2022;150:e2022058859.
van der Staaij H, van der Bom JG, Caram-Deelder C, Lopriore E, Fijnvandraat K, Fustolo-Gunnink SF, et al. Predicting outcomes in preterm neonates with thrombocytopenia (PROSPEC). ClinicalTrials.gov (NCT 06043050). https://clinicaltrials.gov/study/NCT06043050.
Author information
Authors and Affiliations
Contributions
SMT and TMM; study design, collection and assembly of data and final approval of manuscript. TMB; study design, collection and assembly of data, data analysis and interpretation, manuscript writing, editing, and final approval of manuscript. AK, RDC, and RKO, study design, data analysis, manuscript writing, editing, and final approval of manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The Intermountain Health IRB determined this study to be outside the definition of human subject research, that it was exempt from IRB review, and that it did not require written informed consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tweddell, S.M., Morelli, T.M., Bahr, T.M. et al. Identifying barriers to complying with new restrictive NICU transfusion guidelines. J Perinatol (2025). https://doi.org/10.1038/s41372-025-02225-0
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41372-025-02225-0
This article is cited by
-
Involving neonatal hematology and transfusion medicine in global efforts to eliminate severe retinopathy of prematurity
Journal of Perinatology (2025)