Abstract
Background
Neonatal infections cause significant morbidity and mortality. A comprehensive analysis of bloodstream infections (BSI), urinary tract infections (UTI) and meningitis across level IV neonatal intensive care units (NICUs) is lacking.
Methods
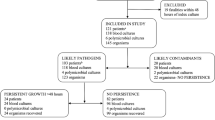
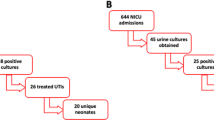
This retrospective cohort study utilized data from the Children’s Hospitals Neonatal Database (CHND) between January 2011 to December 2022. Patients with positive blood, urine, and cerebrospinal fluid (CSF) cultures were assessed. BSI trends across five geographic zones and a 10-year trend were studied.
Results
Of 172,921 patients, 15,541 (9.0%) had a culture-positive BSI, UTI, and/or meningitis. Within the 18,281 positive cultures (9794 BSI, 7097 UTI and 1390 CSF), 21,919 pathogens were identified. Infection rates were inversely related to gestational age. Pathogen distribution varied across regions, and over 10 years, Coagulase negative Staphylococcus declined, while E. coli and S. aureus proportions increased.
Conclusion
Understanding infection trends in level IV NICUs can inform targeted preventive strategies and quality improvement initiatives.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Shane AL, Sanchez PJ, Stoll BJ. Neonatal sepsis. Lancet. 2017;390:1770–80.
Cailes B, Kortsalioudaki C, Buttery J, Pattnayak S, Greenough A, Matthes J, et al. Epidemiology of UK neonatal infections: the neonIN infection surveillance network. Arch Dis Child Fetal Neonatal Ed. 2018;103:F547–F553.
Flannery DD, Edwards EM, Puopolo KM, Horbar JD. Early-onset sepsis among very preterm infants. Pediatrics. 2021;148:e2021052456.
Giannoni E, Dimopoulou V, Klingenberg C, Naver L, Nordberg V, Berardi A, et al. Analysis of antibiotic exposure and early-onset neonatal sepsis in Europe, North America, and Australia. JAMA Netw Open. 2022;5:e2243691.
Klinger G, Bromiker R, Zaslavsky-Paltiel I, Klinger S, Sokolover N, Lerner-Geva L, et al. Late-onset sepsis in very low birth weight infants. Pediatrics. 2023;152:e2023062223.
Flannery DD, Edwards EM, Coggins SA, Horbar JD, Puopolo KM. Late-onset sepsis among very preterm infants. Pediatrics. 2022;150:e2022058813.
American Academy of Pediatrics Committee on Fetus and Newborn. Levels of neonatal care. Pediatrics. 2012;130:587–97.
Stark AR, Pursley DM, Papile LA, Eichenwald EC, Hankins CT, Buck RK, et al. Standards for levels of neonatal care: II, III, and IV. Pediatrics. 2023;151:e2023061957.
Dong Y, Speer CP. Late-onset neonatal sepsis: recent developments. Arch Dis Child Fetal Neonatal Ed. 2015;100:F257–263.
Murthy K, Dykes FD, Padula MA, Pallotto EK, Reber KM, Durand DJ, et al. The Children’s Hospitals Neonatal Database: an overview of patient complexity, outcomes and variation in care. J Perinatol. 2014;34:582–6.
Keene S, Grover TR, Murthy K, Pallotto EK, Brozanski B, Gien J, et al. Extracorporeal membrane oxygenation and bloodstream infection in congenital diaphragmatic hernia. J Perinatol. 2019;39:1384–91.
Keene S, Murthy K, Pallotto E, Brozanski B, Gien J, Zaniletti I, et al. Acquired infection and antimicrobial utilization during initial NICU hospitalization in infants with congenital diaphragmatic hernia. Pediatr Infect Dis J. 2018;37:469–74.
Bizzarro MJ, Shabanova V, Baltimore RS, Dembry LM, Ehrenkranz RA, Gallagher PG. Neonatal sepsis 2004-2013: the rise and fall of coagulase-negative staphylococci. J Pediatr. 2015;166:1193–9.
Puopolo KM, Lynfield R, Cummings JJ, AAP Committee On Fetus and Newborn, AAP Committee On Infectious Diseases. Management of infants at risk for Group B streptococcal disease. Pediatrics. 2019;144:e20192350.
Romain AS, Cohen R, Plainvert C, Joubrel C, Bechet S, Perret A, et al. Clinical and laboratory features of Group B streptococcus meningitis in infants and newborns: study of 848 cases in France, 2001-2014. Clin Infect Dis. 2018;66:857–64.
Horbar JD, Edwards EM, Greenberg LT, Profit J, Draper D, Helkey D, et al. Racial segregation and inequality in the neonatal intensive care unit for very low-birth-weight and very preterm infants. JAMA Pediatr. 2019;173:455–61.
Lake ET, Staiger D, Horbar J, Kenny MJ, Patrick T, Rogowski JA. Disparities in perinatal quality outcomes for very low birth weight infants in neonatal intensive care. Health Serv Res. 2015;50:374–97.
Downey LC, Benjamin DK Jr, Clark RH, Watt KM, Hornik CP, Laughon MM, et al. Urinary tract infection concordance with positive blood and cerebrospinal fluid cultures in the neonatal intensive care unit. J Perinatol. 2013;33:302–6.
Kilpatrick R, Boutzoukas AE, Chan E, Girgis V, Kinduelo V, Kwabia SA, et al. Urinary tract infection epidemiology in NICUs in the United States. Am J Perinatol. 2024;41:e2202–e2208.
Mohseny AB, van Velze V, Steggerda SJ, Smits-Wintjens V, Bekker V, Lopriore E. Late-onset sepsis due to urinary tract infection in very preterm neonates is not uncommon. Eur J Pediatr. 2018;177:33–38.
Eliakim A, Dolfin T, Korzets Z, Wolach B, Pomeranz A. Urinary tract infection in premature infants: the role of imaging studies and prophylactic therapy. J Perinatol. 1997;17:305–8.
Cooper LN, Beauchamp AM, Ingle TA, Diaz MI, Wakene AD, Katterpalli C, et al. Socioeconomic disparities and the prevalence of antimicrobial resistance. Clin Infect Dis. 2024;79:1346–53.
Shane AL, Stoll BJ. Neonatal sepsis: progress towards improved outcomes. J Infect. 2014;68:S24–32.
Cantey JB, Baird SD. Ending the culture of culture-negative sepsis in the neonatal ICU. Pediatrics. 2017;140:e20170044.
Klingenberg C, Kornelisse RF, Buonocore G, Maier RF, Stocker M. Culture-negative early-onset neonatal sepsis - at the crossroad between efficient sepsis care and antimicrobial stewardship. Front Pediatr. 2018;6:285.
Mukhopadhyay S, Puopolo KM, Hansen NI, Lorch SA, DeMauro SB, Greenberg RG, et al. Neurodevelopmental outcomes following neonatal late-onset sepsis and blood culture-negative conditions. Arch Dis Child Fetal Neonatal Ed. 2021;106:467–73.
Acknowledgements
Beverly Brozanski, Jacquelyn Evans, Theresa Grover, Karna Murthy, Michael Padula, Eugenia Pallotto, Anthony Piazza, Kristina Reber and Billie Short and ex-officio David Durand, Francine Dykes, Jeanette Asselin, are executive members of the Children’s Hospitals Neonatal Consortium, Inc., who developed and manage the CHND (thechnc.org). For more information, please contact: exec@thechnc.org. We appreciate Mr. John Mallett and Ms. Evelyn Werbaneth’s contribution to study design and data analysis. We are indebted to the above CHNC participating institutions that serve the infants and their families; these institutions have invested in and continue to participate in the Children’s Hospital’s Neonatal Database (CHND).
Funding
This study was supported by the Children’s Hospitals Neonatal Consortium, Mentored Fellow Research Award, and supported by NIH/NCATS Colorado CTSI Grant Number UL1 TR004399. NIH/NCATS Colorado CTSI Grant had no role in the design and conduct of this study; the contents are the authors’ sole responsibility and do not necessarily represent official NIH views.
Author information
Authors and Affiliations
Contributions
YN and TG conceptualized and designed the study, drafted the initial manuscript, and critically reviewed and revised the manuscript. JZ, SP, KM, MP critically reviewed and revised the manuscript. IZ designed the data collection instruments, collected data, carried out the initial analyses and critically reviewed and revised the manuscript. BW carried out the initial analysis and critically reviewed and revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
KM, MP, TG are Board members of the CHNC, a 501-c-3 Organization. The other authors do not have conflicts of interest to disclose.
Ethics approval
Research involving human subjects, human data is in accordance with the Declaration of Helsinki. The Stanley Manne Children’s Research Institute’s Institutional Review Board (Chicago, IL) provided oversight for this analysis (#2011-14673). Each participating site has IRB oversight to contribute to CHND.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nishihara, Y., Zaniletti, I., Zenge, J. et al. Epidemiology of bacterial and fungal infections among level IV neonatal units in North America. J Perinatol 45, 997–1004 (2025). https://doi.org/10.1038/s41372-025-02337-7
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41372-025-02337-7