Abstract
Objectives
To assess risk factors for acute kidney injury (AKI) in neonates with hypoxic ischemic encephalopathy (HIE) using KDIGO and Gupta definitions, and evaluate long-term kidney function.
Methods
Retrospective study including 72 neonates with HIE and prospective evaluation of long-term kidney health data of 33 survivors.
Results
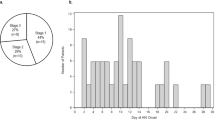
AKI was detected in 49% using KDIGO and 32% using Gupta’s definition. KDIGO-defined AKI correlated with thrombocytopenia, low pH, transfusions need, nephrotoxic drugs, and furosemide use (p < 0.05). The Gupta definition showed additional associations with hypotension, cardiac dysfunction, and death (p < 0.05). In a logistic regression model, both definitions linked AKI to nephrotoxic drug exposure and transfusions. Follow-up assessments revealed elevated blood pressure in 12%, hyperfiltration in 18%, and proteinuria in 6% of survivors.
Conclusions
The Gupta definition may help identify AKI in an additional number of neonates with HIE. Long-term monitoring is essential for the early detection of kidney dysfunction.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
This article and its online supplementary material include all data generated or analyzed during the study. For further inquiries, the corresponding author may be contacted.
References
Arnautovic T, Sinha S, Laptook AR. Neonatal hypoxic-ischemic encephalopathy and hypothermia treatment. Obstet Gynecol. 2024;143:67–81.
Papazian O. [Neonatal hypoxic-ischemic encephalopathy]. Medicina. 2018;78:36–41.
Cánovas-Ahedo M, Alonso-Alconada D. Combined therapy in neonatal hypoxic-ischaemic encephalopathy. An de Pediatría. 2019;91:59.e6.
Rumpel J, Spray BJ, Chock VY, Kirkley MJ, Slagle CL, Frymoyer A, et al. Urine biomarkers for the assessment of acute kidney injury in neonates with hypoxic ischemic encephalopathy receiving therapeutic hypothermia. J Pediatr. 2022;241:133–40.e3.
Robertsson Grossmann K, Bárány P, Blennow M, Chromek M. Acute kidney injury in infants with hypothermia‐treated hypoxic‐ischaemic encephalopathy: an observational population‐based study. Acta Paediatr. 2022;111:86–92.
Gupta C, Massaro AN, Ray PE. A new approach to define acute kidney injury in term newborns with hypoxic ischemic encephalopathy. Pediatr Nephrol. 2016;31:1167–78.
Ahn HC, Frymoyer A, Boothroyd DB, Bonifacio S, Sutherland SM, Chock VY. Acute kidney injury in neonates with hypoxic ischemic encephalopathy based on serum creatinine decline compared to KDIGO criteria. Pediatr Nephrol. 2024;39:2789–96.
Chaturvedi S, Ng KH, Mammen C. The path to chronic kidney disease following acute kidney injury: a neonatal perspective. Pediatr Nephrol. 2017;32:227–41.
Coleman C, Tambay Perez A, Selewski DT, Steflik HJ. Neonatal acute kidney injury. Front Pediatr. 2022;10:842544.
Robertsson Grossmann K, Vishnevskaya L, Diaz Ruiz S, Kublickiene K, Bárány P, Blennow M, et al. Kidney outcomes in early adolescence following perinatal asphyxia and hypothermia-treated hypoxic-ischaemic encephalopathy. Pediatr Nephrol. 2023;38:1205–14.
Roto S, Nupponen I, Kalliala I, Kaijomaa M. Risk factors for neonatal hypoxic ischemic encephalopathy and therapeutic hypothermia: a matched case-control study. BMC Pregnancy Childbirth. 2024;24:421.
Aslam S, Strickland T, Molloy EJ. Neonatal encephalopathy: need for recognition of multiple etiologies for optimal management. Front Pediatr. 2019;7:142.
Pfister RH, Bingham P, Edwards EM, Horbar JD, Kenny MJ, Inder T, et al. The Vermont oxford neonatal encephalopathy registry: rationale, methods, and initial results. BMC Pediatr. 2012;12:84.
Ramya K, Mukhopadhyay K, Kumar J. Predictive factors and risk scoring system for acute kidney injury (AKI) in sick neonates-a prospective cohort study. Eur J Pediatr. 2024;183:5419–24.
Chirico V, Lacquaniti A, Tripodi F, Conti G, Marseglia L, Monardo P, et al. Acute kidney injury in neonatal intensive care unit: epidemiology, diagnosis and risk factors. J Clin Med. 2024;13:3446.
Askenazi DJ, Koralkar R, Hundley HE, Montesanti A, Patil N, Ambalavanan N. Fluid overload and mortality are associated with acute kidney injury in sick near-term/term neonate. Pediatr Nephrol. 2013;28:661–6.
Meena J, Kumar J, Kocharlakota JP, Gupta H, Mittal P, Kumar A, et al. Acute kidney injury in neonates: a meta-analysis. Pediatrics. 2024;154:e2023065182.
Bojan M, Vicca S, Boulat C, Gioanni S, Pouard P. Aprotinin, transfusions, and kidney injury in neonates and infants undergoing cardiac surgery. Br J Anaesth. 2012;108:830–7.
Kecskes Z, Healy G, Jensen A. Fluid restriction for term infants with hypoxic-ischaemic encephalopathy following perinatal asphyxia. Cochrane Database Syst Rev. 2005;2005:Cd004337.
Lyu D, Fu S. Association between platelet count and neonatal acute kidney injury: a cohort study using the medical information mart for intensive care III database. J Matern Fetal Neonatal Med. 2024;37:2379910.
Steflik HJ, Charlton JR, Briley M, Selewski DT, Gist KM, Hanna MH, et al. Neonatal nephrotoxic medication exposure and early acute kidney injury: results from the AWAKEN study. J Perinatol. 2023;43:1029–37.
Turner SS, Davidson JM, Elabiad MT. Changes in urinary kidney injury molecule-1 levels after blood transfusions in preterm infants. Sci Rep. 2021;11:11690.
Debillon T, Bednarek N, Ego A. LyTONEPAL Writing Group. LyTONEPAL: long term outcome of neonatal hypoxic encephalopathy in the era of neuroprotective treatment with hypothermia: a French population-based cohort. BMC Pediatr. 2018;18:255.
Roy JP, Goldstein SL, Schuh MP. Under-recognition of neonatal acute kidney injury and lack of follow-up. Am J Perinatol. 2022;39:526–31.
Starr MC, Harer MW, Steflik HJ, Gorga S, Ambalavanan N, Beck TM, et al. Kidney health monitoring in neonatal intensive care unit graduates: a modified delphi consensus statement. JAMA Netw Open. 2024;7:e2435043.
Akkoc G, Duzova A, Korkmaz A, Oguz B, Yigit S, Yurdakok M. Long-term follow-up of patients after acute kidney injury in the neonatal period: abnormal ambulatory blood pressure findings. BMC Nephrol. 2022;23:116.
Funding
The authors received a research grant from the Portuguese Society of Pediatrics (SPP) (“Bolsa de Investigação SPP”). The first author received a PhD grant from the CUF academic center (“Bolsa de Doutoramento em Medicina”).
Author information
Authors and Affiliations
Contributions
All authors participated in the study conception and design. The first author (SC) was responsible for data collection and analysis and prepared the draft manuscript. The second and third authors (PCR and AMG) reviewed the paper. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics
Study approval statement: This study protocol was reviewed and approved by the Centro Académico de Medicina de Lisboa (CAML) Ethics Committee. Consent to participate statement: A written informed consent was obtained from participants’ parents/legal guardians to participate in the study. All methods were performed in accordance with the relevant guidelines and regulations.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Todo Bom Costa, S., Costa Reis, P. & Mendes Graça, A. Evaluation of risk factors and outcomes of neonates with hypoxic ischemic encephalopathy and acute kidney injury. J Perinatol 45, 1040–1046 (2025). https://doi.org/10.1038/s41372-025-02379-x
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41372-025-02379-x