Abstract
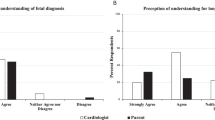
Objective
Survival outcomes are shifting in trisomy 18 as cardiac disease is being repaired in infancy reminiscent of trisomy 21. The landscape of prenatal counseling related to cardiac disease and trisomy 18 is unknown.
Study design
A survey was distributed to pediatric cardiologists presenting two scenarios of cardiac disease varying by genetic diagnosis: trisomy 18 vs 21. Respondents were asked if cardiac surgery would be offered and ranked the importance of various factors in decision-making.
Result
Sixty three percent described surgery as an option in trisomy 18 compared to 97% in trisomy 21. Genetic diagnosis was most important in trisomy 18 compared to neonatal survival in trisomy 21. Quality of life and survival to discharge were least important in trisomy 18 compared to genetic diagnosis in trisomy 21.
Conclusion
Significant variability in prenatal counseling exists for trisomy 18. Indecision may be influenced by the genetic diagnosis, survival, and quality of life.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Goel N, Morris JK, Tucker D, de Walle HE, Bakker MK, Kancherla V, et al. Trisomy 13 and 18-prevalence and mortality-A multi-registry population based analysis. Am J Med Genet A. 2019;179:2382–92.
Stallings EB, Isenburg JL, Rutkowski RE, Kirby RS, Nembhard WN, Sandidge T, et al. National Birth Defects Prevention Network. National population-based estimates for major birth defects, 2016-2020. Birth Defects Res. 2024;116:e2301.
Irving C, Richmond S, Wren C, Longster C, Embleton ND. Changes in fetal prevalence and outcome for trisomies 13 and 18: a population-based study over 23 years. J Matern Fetal Neonatal Med. 2011;24:137–41.
Springett A, Wellesley D, Greenlees R, Loane M, Addor M, Arriola L, et al. Congenital anomalies associated with trisomy 18 or trisomy 13: a registry-based study in 16 European countries, 2000–2011. Am J Med Genet A. 2015;167A:3062–9.
Embleton ND, Wyllie JP, Wright MJ, Burn J, Hunter S. Natural history of trisomy 18. Arch Dis Child. 1996;75:F38–F41.
Van Dyke DC, Allen M. Clinical management considerations in long-term survivors with trisomy 18. Pediatrics. 1990;85:753–9.
Baty BJ, Blackburn BL, Carey JC. Natural history of trisomy 18 and trisomy 13: I. growth, physical assessment, medical histories, survival, and recurrence risk. Am J Med Genet. 1994;49:175–88.
Peterson JK, Kochilas LK, Catton KG, Moller JH, Setty SP. Long-term outcomes of children with trisomy 13 and 18 after congenital heart disease interventions. Ann Thorac Surg. 2017;103:1941–9.
Kosiv KA, Gossett JM, Bai S, Collins RT. 2nd. Congenital heart surgery on in-hospital mortality in trisomy 13 and 18. Pediatrics. 2017;140:e20170772.
Peterson R, Calamur N, Fiore A, Huddleston C, Spence K. Factors influencing outcomes after cardiac intervention in infants with trisomy 13 and 18. Pediatr Cardiol. 2018;39:140–7.
Cooper DS, Riggs KW, Zafar F, Jacobs JP, Hill KD, Pasquali SK, et al. Cardiac surgery in patients with trisomy 13 and 18: an analysis of the Society of Thoracic Surgeons Congenital Heart Surgery Database. J Am Heart Assoc. 2019;8:e012349.
Greene CL, Schulz A, Chávez M, Staffa SJ, Zurakowski D, Friedman KG, et al. Operative and nonoperative outcomes in patients with trisomy 13 and 18 with congenital heart disease. JTCVS Open. 2024;20:123–31.
Greenberg JW, Kulshrestha K, Ramineni A, Winlaw DS, Lehenbauer DG, Zafar F, et al. Contemporary trends in cardiac surgical care for trisomy 13 and 18 patients admitted to hospitals in the United States. J Pediatr. 2024;268:113955.
St Louis JD, Bhat A, Carey JC, Lin AE, Mann PC, Smith LM, et al. The American Association for Thoracic Surgery (AATS) 2023 expert consensus document: recommendation for the care of children with trisomy 13 or trisomy 18 and a congenital heart defect. J Thorac Cardiovasc Surg. 2024;167:1519–32.
Cleary JP, Janvier A, Farlow B, Weaver M, Hammel J, Lantos J. Cardiac interventions for patients with trisomy 13 and Trisomy 18: experience, ethical issues, communication, and the case for individualized family-centered care. World J Pediatr Congenit Heart Surg. 2022;13:72–76.
Carey JC. Management of children with the trisomy 18 and trisomy 13 syndromes: is there a shift in the paradigm of care?. Am J Perinatol. 2021;38:1122–5.
Carvajal HG, Callahan CP, Miller JR, Rensink BL, Eghtesady P. Cardiac surgery in trisomy 13 and 18: a guide to clinical decision-making. Pediatr Cardiol. 2020;41:1319–33.
Champagne CR, Lewis M, Gilchrist DM. Should we mend their broken hearts? The history of cardiac repairs in children with Down syndrome. Pediatrics. 2014;134:1048–50.
Frost N. The Hopkins Mongol case: the dawn of the bioethics movement. Pediatrics. 2020;146:S3–S8.
St Louis JD, Jodhka U, Jacobs JP, Xia H, Hill KD, Pasquali SK, et al. Contemporary outcomes of complete atrioventricular septal defect repair: analysis of the Society of Thoracic Surgeons Congenital Heart Surgery database. J Thorac Cardiovasc Surg. 2014;148:2526–31.
Meyer RE, Liu G, Gilboa SM, Ethen MK, Aylsworth AS, Powell CM, et al. National Birth Defects Prevention Network. Survival of children with trisomy 13 and trisomy 18: a multi-state population-based study. Am J Med Genet A. 2016;170A:825–37.
Tamaki S, Iwatani S, Izumi A, Hirayama K, Kataoka D, Ohyama S, et al. Improving survival in patients with trisomy 18. Am J Med Genet A. 2022;188:1048–55.
Cortezzo DE, Tolusso LK, Swarr DT. Perinatal outcomes of fetuses and infants diagnosed with trisomy 13 or trisomy 18. J Pediatr. 2022;247:116–23.e5.
Mizrahi M, Well A, Gottlieb EA, Stewart E, Lucke A, Fraser CD, et al. Trisomy 18: disparities of care and outcomes in the State of Texas between 2009 and 2019. Cardiol Young. 2023;33:2328–33.
Evans JM, Dharmar M, Meierhenry E, Marcin JP, Raff GW. Association between Down syndrome and in-hospital death among children undergoing surgery for congenital heart disease: a US population-based study. Circ Cardiovasc Qual Outcomes. 2014;7:445–52.
Jacobs JP, O’Brien SM, Hill KD, Kumar SR, Austin EH, Gaynor JW, et al. Refining the Society of Thoracic Surgeons Congenital Heart Surgery database mortality risk model with enhanced risk adjustment for chromosomal abnormalities, syndromes, and noncardiac congenital anatomic abnormalities. Ann Thorac Surg. 2019;108:558–66.
Curzon CL, Milford-Beland S, Li JS, O’Brien SM, Jacobs JP, Jacobs ML, et al. Cardiac surgery in infants with low birth weight is associated with increased mortality: analysis of the Society of Thoracic Surgeons Congenital Heart database. J Thorac Cardiovasc Surg. 2008;135:546–51.
Alsoufi B, McCracken C, Ehrlich A, Mahle WT, Kogon B, Border W, et al. Single ventricle palliation in low weight patients is associated with worse early and midterm outcomes. Ann Thorac Surg. 2015;99:668–76.
Miller TA, Ghanayem NS, Newburger JW, McCrindle BW, Hu C, DeWitt AG, et al. Pediatric Heart Network Investigators. Gestational age, birth weight, and outcomes six years after the Norwood procedure. Pediatrics. 2019;143:e20182577.
Alsoufi B, McCracken C, Oster M, Shashidharan S, Kanter K. Genetic and extracardiac anomalies are associated with inferior single ventricle palliation outcomes. Ann Thorac Surg. 2018;106:1204–12.
Jenkins KJ, Gauvreau K, Newburger JW, Spray TL, Moller JH, Iezzoni LI. Consensus-based method for risk adjustment for surgery for congenital heart disease. J Thorac Cardiovasc Surg. 2002;123:110–8.
Tahara M, Shimozono S, Nitta T, Yamaki S. Medial defects of the small pulmonary arteries in fatal pulmonary hypertension in infants with trisomy 13 and trisomy 18. Am J Med Genet A. 2014;164A:319–23.
Kosiv KA, Long J, Lee HC, Collins RT 2nd. A validated model for prediction of survival to 6 months in patients with trisomy 13 and 18. Am J Med Genet A. 2021;185:806–13.
Kuo DZ, Houtrow AJ. Council on children with disabilities. Recognition and management of medical complexity. Pediatrics. 2016;138:e20163021.
Weaver MS, Anderson V, Beck J, Delaney JW, Ellis C, Fletcher S, et al. Interdisciplinary care of children with trisomy 13 and 18. Am J Med Genet A. 2021;185:966–77.
Kim AJH, Marshall M, Gievers L, Tate T, Taub S, Dukhovny S, et al. Structured framework for multidisciplinary parent counseling and medical interventions for fetuses and infants with trisomy 13 or trisomy 18. Am J Perinatol. 2024;41:e2666–e2673.
Janvier A, Farlow B, Wilfond BS. The experience of families with children with trisomy 13 and 18 in social networks. Pediatrics. 2012;130:293–8.
Guon J, Wilfond BS, Farlow B, Brazg T, Janvier A. Our children are not a diagnosis: the experience of parents who continue their pregnancy after a prenatal diagnosis of trisomy 13 or 18. Am J Med Genet A. 2014;164A:308–18.
Fruhman G, Miller C, Amon E, Raible D, Bradshaw R, Martin K. Obstetricians’ views on the ethics of cardiac surgery for newborns with common aneuploidies. Prenat Diagn. 2018;38:303–9.
Jacobs AP, Subramaniam A, Tang Y, Phillips JB, Biggio JR, Edwards RK, et al. Trisomy 18: a survey of opinions, attitudes, and practices of neonatologists. Am J Med Genet A. 2016;170:2638–43.
Bierer R, Mladucky J, Anderson R, Carey JC. Parent narratives provide perspectives on the experience of care in trisomy 18. Am J Med Genet C Semin Med Genet. 2024;11:e32114.
Salter EK, Hester DM, Vinarcsik L, Antommaria AHM, Bester J, Blustein J, et al. Pediatric decision making: consensus recommendations. Pediatrics. 2023;152:e2023061832.
Kon AA. The shared decision-making continuum. JAMA. 2010;304:903–4.
Stacey D, Légaré F, Lewis K, Barry MJ, Bennet CL, Eden KB, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2017;4:CD001431.
Yu L, Yang S, Zhang C, Guo P, Zhang X, Xu M, et al. Decision aids for prenatal testing: a systematic review and meta-analysis. J Adv Nurs. 2021;77:3964–79.
Wong HYC, Asim S, Feng Q, Fu SXH, Sahota DS, So PL, et al. Effectiveness of interactive digital decision aids in prenatal screening decision-making: systematic review and meta-analysis. J Med Internet Res. 2023;25:e37953.
Andrews SE, Downey AG, Showalter DS, Fitzgerald H, Showalter VP, Carey JC, et al. Shared decision making and the pathways approach in the prenatal and postnatal management of the trisomy 13 and trisomy 18 syndromes. Am J Med Genet C Semin Med Genet. 2016;172:257–63.
Haug S, Goldstein M, Cummins D, Fayard E, Merritt TA. Using patient-centered care after a prenatal diagnosis of trisomy 18 or trisomy 13: A Review. JAMA Pediatr. 2017;171:382–7.
Pyle AK, Fleischman AR, Hardart G, Mercurio MR. Management options and parental voice in the treatment of trisomy 13 and 18. J Perinatol. 2018;38:1135–43.
Leuthner SR, Acharya K. Perinatal counseling following a diagnosis of Trisomy 13 or 18: incorporating the facts, parental values, and maintaining choices. Adv Neonatal Care. 2020;20:204–15.
Acknowledgements
The authors would like to thank the Institutional Sponsors of the nonprofit 501(c)(3) Fetal Heart Society and the Utah Center for Excellence in ELSI Research. A full list of Fetal Heart Society sponsors is available at: https://fetalheartsociety.org/donations/institutional-sponsors/.
Funding
UCEER Pilot Fund.
Author information
Authors and Affiliations
Contributions
KK conceived the project, designed of the survey instrument, interpreted the analysis and prepared tables, and drafted the initial manuscript; BW advised on the study, assisted with the design of the survey instrument, conducted the analysis, and created figures, and critically reviewed and revised the manuscript; RA advised on the study, assisted with the design of the survey instrument, and critically reviewed and revised the manuscript; JC conceived the project, assisted with the design of the survey instrument, interpreted the analysis, and critically reviewed and revised the manuscript; and all authors approved the final manuscript as submitted and agreed to be accountable for all aspects of the work. KK has full access to the study data and final responsibility for the decision to submit for publication.
Corresponding author
Ethics declarations
Competing interests
KAK and JCC both serve as physician advisors to the Support Organization for Trisomy (SOFT), a parent support group. KAK serves on the steering committee and JCC serves on the executive committee for the Trisomy 13 and 18 Collaborative, which is philanthropic initiative to support families impacted by trisomy 13 and 18 and promote shared decision-making.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kosiv, K.A., Wong, B.G., Anderson, R.A. et al. Current prenatal counseling of congenital heart disease in trisomy 18, pediatric cardiologists’ perspective: a Fetal Heart Society Research Collaborative Study. J Perinatol (2025). https://doi.org/10.1038/s41372-025-02392-0
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41372-025-02392-0