Abstract
Objective
Describe how preterm infants experience residential mobility, or moving, before age 2 years.
Study design
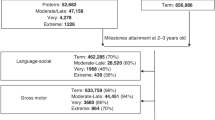
This retrospective cohort study included 9267 preterm infants followed in a mid-Atlantic urban and suburban primary care network. Multivariable regression modeling identified patient and community factors associated with residential mobility, defined by a change in Census Block Group.
Results
2494 infants (27%) moved before age 2 years; 559 (6%) moved more than once. Extreme prematurity, compared to late prematurity, was associated with increased odds of mobility (aOR 1.26, 95% CI 1.03–1.54). Governmental insurance, male sex, a positive or missing post-partum depression screen, and neighborhood deprivation were also positively associated with mobility. Among movers, 741 (30%) first relocated before 6 months of age, and mobility rates decreased with increasing chronologic age.
Conclusion
Early-life residential mobility is common among preterm infants, particularly extremely preterm infants. These findings have implications for discharge preparation among this vulnerable group.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The data utilized in this study are held securely with the Arcus Data Repository at the Children’s Hospital of Philadelphia. Conditions of the data sharing agreements between the authors and Arcus and the sensitive nature of the data prohibit public posting of the full datasets. Requests for future research are available for CHOP-credentialed researchers via the Arcus Archives. Code for the full dataset creation and analysis is available from the authors upon request. • Arcus Data Repository Team. Arcus Data Repository. Extracted: June 10, 2024. Version v1 15.7. Arcus at the Children’s Hospital of Philadelphia. • Sankey Diagram created using SankeyArt, accessed June 1, 2025 at https://www.sankeyart.com/.
Code availability
Code for the dataset creation and analysis is available upon request.
References
Amoah DK, Nolan V, Relyea G, Gurney JG, Yu X, Tylavsky FA, et al. Factors associated with residential mobility during pregnancy. Women Health. 2018;58:955–66.
Margerison-Zilko C, Cubbin C, Jun J, Marchi K, Braveman P. Post-partum residential mobility among a statewide representative sample of California Women, 2003–2007. Matern Child Health J. 2016;20:139–48.
Saadeh FB, Clark MA, Rogers ML, Linkletter CD, Phipps MG, Padbury JF, et al. Pregnant and moving: understanding residential mobility during pregnancy and in the first year of life using a prospective birth cohort. Matern Child Health J. 2013;17:330–43.
Meeker JR, Burris H, Boland MR. An algorithm to identify residential mobility from electronic health-record data. Int J Epidemiol. 2022;50:2048–57.
Ling C, Heck JE, Cockburn M, Liew Z, Marcotte E, Ritz B. Residential mobility in early childhood and the impact on misclassification in pesticide exposures. Environ Res. 2019;173:212–20.
Mollborn S, Lawrence E, Root ED. Residential mobility across early childhood and children’s kindergarten readiness. Demography. 2018;55:485–510.
Swaminathan S, Alexander GR, Boulet S. Delivering a very low birth weight infant and the subsequent risk of divorce or separation. Matern Child Health J. 2006;10:473–9.
Singer LT, Fulton S, Kirchner HL, Eisengart S, Lewis B, Short E, et al. Parenting very low birth weight children at school age: maternal stress and coping. J Pediatr. 2007;151:463–9.
Schappin R, Wijnroks L, Uniken Venema MMAT, Jongmans MJ. Rethinking stress in parents of preterm infants: a meta-analysis. PLoS One. 2013;8:e54992.
Lakshmanan A, Song AY, Belfort MB, Yieh L, Dukhovny D, Friedlich PS, et al. The financial burden experienced by families of preterm infants after NICU discharge. J Perinatol. 2022;42:223–30.
Nassel D, Chartrand C, Doré-Bergeron M-J, Lefebvre F, Ballantyne M, Van Overmeire B, et al. Very preterm infants with technological dependence at home: impact on resource use and family. Neonatology. 2019;115:363–70.
Saurel-Cubizolles M-J, Marchand-Martin L, Pierrat V, Arnaud C, Burguet A, Fresson J, et al. Maternal employment and socio-economic status of families raising children born very preterm with motor or cognitive impairments: the EPIPAGE cohort study. Dev Med Child Neurol. 2020;62:1182–90.
Cordova-Ramos EG, Brochier A, Tripodis Y, Garg A, Parker MG. Beyond income: material hardship and the health and healthcare of premature children. J Perinatol. 2023;43:357–63.
Simsek M, Costa R, de Valk HAG. Childhood residential mobility and health outcomes: a meta-analysis. Health Place. 2021;71:102650.
Jelleyman T, Spencer N. Residential mobility in childhood and health outcomes: a systematic review. J Epidemiol Community Health. 2008;62:584–92.
Pearce A, Elliman D, Bedford H, Law C.Millennium Cohort Study Child Health Group Residential mobility and uptake of childhood immunisations: findings from the UK Millennium Cohort Study. Vaccine. 2008;26:1675–80.
Lucas JA, Hsu A, Heintzman J, Bailey SR, Suglia SF, Bazemore A, et al. The association of mobility, social deprivation, and pediatric primary care outcomes in community health centers. J Pediatr. 2023;259:113465.
Medical Home Initiatives for Children With Special Needs Project Advisory Committee The medical home. Pediatrics. 2002;110:184–6.
Connors J, Havranek T, Campbell D. Discharge of medically complex infants and developmental follow-up. Pediatr Rev. 2021;42:316–28.
Preterm Birth [Internet]. March of Dimes | PeriStats. [cited 15 July 2025]. Available from: https://www.marchofdimes.org/peristats/data?top=3.
D’Agostino JA, Passarella M, Saynisch P, Martin AE, Macheras M, Lorch SA. Preterm infant attendance at health supervision visits. Pediatrics. 2015;136:e794–802.
Hobbs M, Moltchanova E, Marek L, Yogeeswaran K, Milfont TL, Deng B, et al. Environmental influences on mental health: eight-year longitudinal data show a bi-directional association between residential mobility and mental health outcomes. Health Place. 2025;94:103487.
Abenavoli R., Amadon S., Briggs S Cascading effects of residential mobility on maternal and child mental health. Dev Psychol; e-pub ahead of print, 10 April 2025; https://doi.org/10.1037/dev0001950.
Kind AJH, Buckingham WR. Making neighborhood-disadvantage metrics accessible - the neighborhood Atlas. N Engl J Med. 2018;378:2456–8.
Banwell E, Collaco JM, Oates GR, Rice JL, Juarez LD, Young LR, et al. Area deprivation and respiratory morbidities in children with bronchopulmonary dysplasia. Pediatr Pulmonol. 2022;57:2053–9.
Sullivan K, Thakur N. Structural and social determinants of health in asthma in developed economies: a scoping review of literature published between 2014 and 2019. Curr Allergy Asthma Rep. 2020;20:5.
Boyd RW, Lindo EG, Weeks LD, McLemore MR On racism: a new standard for publishing on racial health inequities. Health Affairs Forefront [Internet]. [cited 17 July 2024]; Available from: https://www.healthaffairs.org/content/forefront/racism-new-standard-publishing-racial-health-inequities.
Lawrence E, Root ED, Mollborn S. Residential mobility in early childhood: Household and neighborhood characteristics of movers and non-movers. Demogr Res. 2015;33:939–50.
Groenwold RHH, White IR, Donders ART, Carpenter JR, Altman DG, Moons KGM. Missing covariate data in clinical research: when and when not to use the missing-indicator method for analysis. CMAJ. 2012;184:1265–9.
Morris T, Manley D, Sabel CE. Residential mobility: Towards progress in mobility health research. Prog Hum Geogr. 2018;42:112–33.
Edwards EM, Ehret DEY, Horbar JD Potentially better practices for follow through in neonatal intensive care units. Pediatrics 2024;154:e2023065530.
Cordova-Ramos EG, Kerr S, Heeren T, Drainoni M-L, Garg A, Parker MG. National prevalence of social determinants of health screening among US neonatal care units. Hosp Pediatr. 2022;12:1040–7.
Boone KM, Nelin MA, Chisolm DJ, Keim SA. Gaps and Factors Related to Receipt of Care within a Medical Home for Toddlers Born Preterm. J Pediatr. 2019;207:1618e1.
Kuzniewicz MW, Parker S-J, Schnake-Mahl A, Escobar GJ. Hospital readmissions and emergency department visits in moderate preterm, late preterm, and early term infants. Clin Perinatol. 2013;40:753–75.
Liao Y, Gil J, Pereira RHM, Yeh S, Verendel V. Disparities in travel times between car and transit: Spatiotemporal patterns in cities. Sci Rep. 2020;10:4056.
CDC. Suicide Prevention Communication Playbook [Internet]. Suicide Prevention. 2025. [cited 2025 May 28]; Available from https://www.cdc.gov/suicide/playbook/index.html.
Bruckner TA, Kane JB, Gailey S. Strong upward neighborhood mobility and preterm birth: a matched-sibling design approach. Ann Epidemiol. 2019;36:48–54.e1.
Collins JW Jr, Colgan J, Rankin KM, Desisto C. Affluent-born White mother’s descending neighborhood income and infant mortality: a population-based study. Matern Child Health J. 2018;22:1484–91.
Jairam JA, Cohen E, Diong C, Berger H, Brown HK, Guan J, et al. Maternal downward neighborhood income mobility and ensuing severe neonatal morbidity. JAMA Pediatr 2025;179:463–5.
Gailey S, Ncube CN, Sadler RC, Bruckner TA. Neighborhood mobility and racial disparities in preterm birth: a sibling study in California. Health Place. 2024;89:103280.
Tunstall H, Mitchell R, Pearce J, Shortt N. The general and mental health of movers to more- and less-disadvantaged socio-economic and physical environments within the UK. Soc Sci Med. 2014;118:97–107.
Gailey S, Cross RI, Messer LC, Bruckner TA. Characteristics associated with downward residential mobility among birthing persons in California. Soc Sci Med. 2021;279:113962.
Coulter R, Van Ham M, Findlay AM. Re-thinking residential mobility: Linking lives through time and space. Prog Hum Geogr. 2016;40:352–74.
Schinasi LH, Auchincloss AH, Forrest CB, Diez Roux AV. Using electronic health record data for environmental and place based population health research: a systematic review. Ann Epidemiol. 2018;28:493–502.
Acknowledgements
This research received support from Arcus at the Children’s Hospital of Philadelphia, which provided access to the data and resources. Murosko was supported by an NIH Award, T32HL098054. A GIS Pilot Award sponsored by Arcus at the Children’s Hospital of Philadelphia supported this project.
Author information
Authors and Affiliations
Contributions
D Murosko: Conceptualization; Funding acquisition; Investigation; Methodology; Visualization; Roles/Writing—original draft; and Writing—review & editing. T Nelin: Conceptualization; Investigation; Methodology; Validation; Writing—review & editing P. Sharma, V Tam and E Volkova: Data curation; Formal analysis; Investigation; Methodology; Project administration; Writing—review & editing. K Scott: Conceptualization; Methodology; Writing—review & editing. EF Gregory and S Lorch: Conceptualization; Methodology; Resources; Supervision; Validation; Writing—review & editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Murosko, D., Nelin, T., Sharma, P. et al. Prevalence, predictors, and patterns of residential mobility by the parents of preterm infants. J Perinatol (2025). https://doi.org/10.1038/s41372-025-02414-x
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41372-025-02414-x