Abstract
Objective
Describe racial and ethnic differences in delivery hospital NICU risk-adjusted mortality and morbidity rates (RAMMR), stratified by volume and level of care.
Study design
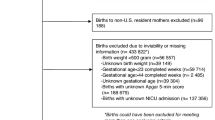
Cross-sectional analysis of all very low birthweight (<1500 g; VLBW) infants born in Michigan, Oregon, and South Carolina between 2010 and 2020 and Pennsylvania between 2010 and 2018 (n = 37,784). Lorenz concentration curves and indices were used to describe differences in NICU RAMMR by race and ethnicity. Analysis was performed for overall cohort; high-level, high-volume NICUs; and low-level and/or low-volume NICUs.
Result
Despite being most frequently born at high-level, high-volume centers, Non-Hispanic Black (NHB) neonates were overrepresented at hospitals with high RAMMR and all other groups were overrepresented at hospitals with lower RAMMR. Differences were most pronounced in the low-level and/or low-volume cohort.
Conclusion
NHB VLBW infants born at hospitals with low-level and/or low-volume NICUs are disproportionately exposed to adverse outcomes and must be the focus of future policy interventions.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
Data were obtained through specific data use agreements with the governments of the states included in this study. Individuals seeking to complete work utilizing these datasets must reach out to each state to obtain direct approvals and data access.
References
Johnson JD, Green CA, Vladutiu CJ, Manuck TA. Racial disparities in prematurity persist among women of high socioeconomic status. Am J Obstet Gynecol MFM. 2020;2:100104.
Hamilton BE, Martin JA, Osterman MJK. CDC vital statistics rapid release births: provisional data for 2022 [Internet]. Centers for Disease Control and Prevention; 2022 [cited 2025 Sep 16]. Available from: https://www.cdc.gov/nchs/products/index.htm.
Lewis TR, Kielt MJ, Walker VP, Levin JC, Guaman MC, Panitch HB, et al. Association of racial disparities with in-hospital outcomes in severe bronchopulmonary dysplasia. JAMA Pediatr. 2022;176:852–9.
Keller RL, Feng R, DeMauro SB, Ferkol T, Hardie W, Rogers EE, et al. Bronchopulmonary dysplasia and perinatal characteristics predict 1-year respiratory outcomes in newborns born at extremely low gestational age: a prospective cohort study. J Pediatr. 2017;187:89–97.e3.
Wang J, Ying GS, Yu Y, Tomlinson L, Binenbaum G. Racial differences in retinopathy of prematurity. Ophthalmic Epidemiol. 2023;30:523–31.
Qureshi AI, Adil MM, Shafizadeh N, Majidi S. A 2-fold higher rate of intraventricular hemorrhage-related mortality in African American neonates and infants Clinical article. J Neurosurg Pediatr. 2013;12:49–53.
Wolf MF, Rose AT, Goel R, Canvasser J, Stoll BJ, Patel RM. Trends and racial and geographic differences in infant mortality in the United States due to necrotizing enterocolitis, 1999 to 2020. JAMA Netw Open. 2023;6:E231511.
Travers CP, Carlo WA, McDonald SA, Das A, Ambalavanan N, Bell EF, et al. Racial/ethnic disparities among extremely preterm infants in the United States from 2002 to 2016. JAMA Netw Open. 2020;3:e206757.
Howell EA, Janevic T, Hebert PL, Egorova NN, Balbierz A, Zeitlin J. Differences in morbidity and mortality rates in black, white, and hispanic very preterm infants among New York City Hospitals. JAMA Pediatr. 2018;172:269–77.
Kunz SN, Phibbs CS, Profit J. The changing landscape of perinatal regionalization. Semin Perinatol. 2020;44:151241.
Phibbs CS, Baker LC, Caughey AB, Danielsen B, Schmitt SK, Phibbs RH. Level and Volume of Neonatal Intensive Care and Mortality in Very-Low-Birth-Weight Infants. N Engl J Med [Internet]. 2007;356:2165–75.
Lasswell S, Barfield W, Rochat R, Blackmon L. Perinatal regionalization for very low-birth-weight and very preterm infants: A meta-analysis. JAMA. 2010;304:992–1000.
Lorch S, Baiocchi M, Ahlberg C, Small D. The differential impact of delivery hospital on the outcomes of premature infants. Pediatrics. 2012;130:270–8.
Yannekis G, Passarella M, Lorch S. Differential effects of delivery hospital on mortality and morbidity in minority premature and low birth weight neonates. J Perinatol. 2020;40:404–11.
Phibbs CS, Passarella M, Schmitt SK, Martin A, Lorch SA. The impact of hospital delivery volumes of newborns born very preterm on mortality and morbidity. J Pediatr. 2025;276:114323.
Jensen EA, Lorch SA. Effects of a birth hospital’s neonatal intensive care unit level and annual volume of very low-birth-weight infant deliveries on morbidity and mortality. JAMA Pediatr. 2015;169:e151906.
Horbar JD, Edwards EM, Greenberg LT, Profit J, Draper D, Helkey D, et al. Racial segregation and inequality in the neonatal intensive care unit for very low-birth-weight and very preterm infants. JAMA Pediatr. 2019;173:455–61.
Profit J, Kowalkowski MA, Zupancic JAF, Pietz K, Richardson P, Draper D, et al. Baby-MONITOR: a composite indicator of NICU quality. Pediatrics. 2014;134:74–82.
Lake ET, Staiger D, Horbar J, Kenny MJ, Patrick T, Rogowski JA. Disparities in perinatal quality outcomes for very low birth weight infants in neonatal intensive care. Health Serv Res. 2015;50:374–97.
Handley SC, Formanowski B, Passarella M, Kozhimannil KB, Leonard SA, Main EK, et al. Perinatal care measures are incomplete if they do not assess the birth parent–infant dyad as a whole. Health Aff. 2023;42:1266–74.
Oregon Health Authority. Oregon Hospital Discharge Data (2010-2020). Oregon Health Authority Hospital Reporting Program. Portland, OR; 2023.
Phibbs CS, Passarella M, Schmitt SK, Rogowski JA, Lorch SA. Understanding the relative contributions of prematurity and congenital anomalies to neonatal mortality. J Perinatol. 2022;42:569–73.
Kozhimannil KB, Thao V, Hung P, Tilden E, Caughey AB, Snowden JM. Association between hospital birth volume and maternal morbidity among low-risk pregnancies in rural, urban, and teaching hospitals in the United States. Am J Perinatol. 2016;33:590–9.
Horbar JD, Carpenter JH, Badger GJ, Kenny MJ, Soll RF, Morrow KA, et al. Mortality and neonatal morbidity among infants 501 to 1500 grams from 2000 to 2009. Pediatrics. 2012;129:1019–26.
Saigal S, Doyle LW. Preterm Birth 3 An overview of mortality and sequelae of preterm birth from infancy to adulthood. Lancet. 2008;371:261–69.
Johnson TJ, Patel AL, Jegier BJ, Engstrom JL, Meier PP. Cost of morbidities in very low birth weight infants. J Pediatr. 2013;162:243–49.
Tribolet S, Dénes S. Standardized management of the first hour of premature infants: a meta-analysis. Pediatrics. 2025;155:e2024068606.
Leonard SA, Kennedy CJ, Carmichael SL, Lyell DJ, Main EK. An expanded obstetric comorbidity scoring system for predicting severe maternal morbidity. Obstetrics Gynecol. 2020;136:440–9.
Chung J, Phibbs C, Boscardin W, Kominski G, Ortega A, Needleman J. The effect of neonatal intensive care level and hospital volume on mortality of very low birth weight infants. Med Care. 2010;48:635–44.
Chung J, Phibbs C, Boscardin W, Kominski G, Ortega A, Gregory K, et al. Examining the effect of hospital-level factors on mortality of very low birth weight infants using multilevel modeling. J Perinatol. 2011;31:770–5.
Stark AR, Pursley DWM, Papile LA, Eichenwald EC, Hankins CT, Buck RK, et al. Standards for Levels of Neonatal Care: II, III, and IV. Pediatrics. 2023;151:e2023061957.
Jann B. Estimating Lorenz and concentration curves. Stata J. 2016;16:837–66.
O’donnell O, O’neill S, VanOurti T, Walsh B. conindex: Estimation of concentration indices. Stata J. 2016;16:112–38.
Beck AF, Edwards EM, Horbar JD, Howell EA, McCormick MC, Pursley DWM. The color of health: how racism, segregation, and inequality affect the health and well-being of preterm infants and their families. Pediatr Res. 2020;87:227–34.
Murosko D, Passerella M, Lorch S. Racial segregation and intraventricular hemorrhage in preterm infants. Pediatrics. 2020;145:e20191508.
Howell E, Herbert P, Chatterjee S, Kleiman L, Chassin M. Black/white differences in very low birth weight neonatal mortality rates among New York City hospitals. Pediatrics. 2008;121:e407–415.
Howell EA, Egorova NN, Balbierz A, Zeitlin J, Hebert PL. Site of delivery contribution to black-white severe maternal morbidity disparity. Am J Obstet Gynecol. 2016;215:143–52.
Handley SC, Passarella M, Interrante JD, Kozhimannil KB, Lorch SA. Perinatal outcomes for rural obstetric patients and neonates in rural-located and metropolitan-located hospitals. J Perinatol. 2022;42:1600–6.
HHS. U.S. Department of Health and Human Services Implementation Guidance on Data Collection Standards for Race, Ethnicity, Sex, Primary Language, and Disability Status [Internet]. US Department of Health and Human Services; 2011 [cited 2025 Sep 16]. Available from: http://www.whitehouse.gov/omb/fedreg_1997standards/.
Mai B, Nguyen D, Alcantar CM, Curammeng ER, Hernandez E, Kim V, et al. The racial heterogeneity project: implications for educational research, practice, and policy. ACT Center for Equity in Learning. 2017.
Acknowledgements
Authors: Dr. Gia Yannekis was supported by AHRQ grant number T32HS000063 as part of the Harvard-wide Pediatric Health Services Research Fellowship Program.
Additional Contributions: Joshua Radack, MS contributed significantly to NICU level assignment verification. Davene Wright, PhD served as Gia Yannekis’s mentor through the Harvard-Wide Pediatric Health Services Research Fellowship and provided support in project development and editing.
Michigan: The data used in this manuscript was acquired from the Michigan Department of Health and Human Services (MDHHS). The contents of this document including data analysis, interpretation or conclusions are solely the responsibility of the authors and do not represent the official views of MDHHS.
Oregon: Oregon Health Authority. Oregon Hospital Discharge Data (2010-2020). Oregon Health Authority Hospital Reporting Program. Portland, OR; 2023.
Pennsylvania: The Pennsylvania Health Care Cost Containment Council (PHC4) is an independent state agency responsible for addressing the problem of escalating health costs, ensuring the quality of health care, and increasing access to health care for all citizens regardless of ability to pay. PHC4 has provided data to this entity in an effort to further PHC4’s mission of educating the public and containing health care costs in Pennsylvania. PHC4, its agents, and staff, have made no representation, guarantee, or warranty, express or implied, that the data – financial, patient, payor, and physician specific information – provided to this entity, are errorfree, or that the use of the data will avoid differences of opinion or interpretation. This analysis was not prepared by PHC4. This analysis was done by the aforementioned authors, based in the Lorch Lab at Children’s Hospital of Philadelphia, as well as at Beth Israel Deaconess Medical Center and Boston Children’s Hospital. PHC4, its agents and staff, bear no responsibility or liability for the results of the analysis, which are solely the opinion of this entity.
South Carolina: This information is from the records of the Revenue and Fiscal Affairs Office, Health and Demographics Section, South Carolina. Our authorization to release this information does not imply endorsement of this study or its findings by either the revenue and fiscal affairs office or the data oversight council.
Funding
Funding for this study was provided by Eunice Kennedy Shriver National Institute of Child Health and Human Development R01HD099197 and R01HD084819.
Author information
Authors and Affiliations
Contributions
Dr. Scott Lorch developed the dataset for this project. Drs. Gia Yannekis, Sarah Kunz, and Scott Lorch all contributed to idea development, project design, data analysis, and manuscript writing and editing. Molly Passarella and Brielle Formanowski cleaned and prepared data and assisted with data analysis and with editing of the final product.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was determined to be Non-Human Subjects Research by the Institutional Review Boards of the Children’s Hospital of Philadelphia (IRB 20-017453), Beth Israel Deaconess Medical Center (2023D000917), and Boston Children’s Hospital (IRB-P00046692). All methods were performed in accordance with the relevant guidelines and regulations.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yannekis, G., Kunz, S.N., Passarella, M. et al. Disparities in delivery hospital risk-adjusted outcomes for very low birthweight infants: the role of NICU volume and level of care. J Perinatol 46, 238–245 (2026). https://doi.org/10.1038/s41372-025-02434-7
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41372-025-02434-7