Abstract
Objective
Most Neonatal Intensive Care Unit (NICU) literature focuses on parent perspectives, overlooking how staff perceive and respond to family needs. We examined NICU staff perceptions to understand family experiences through a relational and systemic lens.
Design
We conducted five focus groups (N = 22) with multidisciplinary staff and used an inductive-deductive approach to identify themes.
Results
Staff emphasized that families have both unique journeys and common experiences. Staff described how sociocultural barriers, trauma histories, and the reproductive/NICU journey shape family stress. Common stressors include multiple traumas, grief and guilt, and ongoing uncertainty. Although coping strategies are influenced by family values/goals and prior experiences, staff commonly observed emotion-driven behaviors, involvement in care, and less self-care. Staff also noted that the NICU can disrupt family dynamics and communication, yet existing relationship dynamics shape family impact.
Conclusion
Staff perspectives provide additional context for understanding family experiences and highlight the need for tailored family-centered care.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
Data available upon reasonable request from the corresponding author.
References
Martin JA, Hamilton BE, Osterman MJK, Driscoll AK. Births: final data for 2019. Natl Vital Stat Rep. 2021;70:1–51. Retrieved from: https://www.cdc.gov/nchs/data/nvsr/nvsr70/nvsr70-02-508.pdf.
Grunberg VA, Geller PA, Hoffman C, Njoroge W, Ahmed A, Patterson CA. Parental mental health screening in the NICU: a psychosocial team initiative. J Perinatol. 2022;42:401–9. https://doi.org/10.1038/s41372-021-01217-0.
D’Agata AL, Coughlin M, Sanders MR. Clinician perceptions of the NICU infant experience: is the NICU hospitalization traumatic? Am J Perinatol. 2018;35:1159–67. https://doi.org/10.1055/s-0038-1641747.
Gorsky KG, Butala S, House M, Moon C, Calvetti S, Khando T, et al. Uncertainty and the NICU experience: a qualitative evaluation of family and provider perspectives. Children. 2023;10:1745 https://doi.org/10.3390/children10111745.
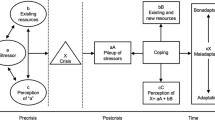
Loewenstein K, Barroso J, Phillips S. The experiences of parents in the neonatal intensive care unit: an integrative review of qualitative studies within the transactional model of stress and coping. J Perinat Neonatal Nurs. 2019;33:340–9. https://doi.org/10.1097/JPN.0000000000000436.
Flacking R, Ewald U, Nyqvist KH, Starrin B. Trustful bonds: a key to “becoming a mother” and to reciprocal breastfeeding. Stories of mothers of very preterm infants at a neonatal unit. Soc Sci Med. 2006;62:70–80. https://doi.org/10.1016/j.socscimed.2005.05.026.
Hendson L, Reis, Nicholas DB. Health care providers’ perspectives of providing culturally competent care in the NICU. J Obstet Gynecol Neonatal Nurs. 2015;44:17–27. https://doi.org/10.1111/1552-6909.12524.
Orr E, Ballantyne M, Gonzalez A, Jack SM. Providers’ perspectives of the neonatal intensive care unit context and care provision for adolescent parents: an interpretive description. BMC Pregnancy Childbirth. 2023;23:259. https://doi.org/10.1186/s12884-023-05553-1.
Huenink E, Porterfield S. Parent support programs and coping mechanisms in NICU parents. Adv Neonatal Care. 2017;17:E10–E18. https://doi.org/10.1097/ANC.0000000000000359.
Smith VC, Steelfisher GK, Salhi C, Shen LY. Coping with the neonatal intensive care unit experience: parents’ strategies and views of staff support. J Perinat Neonatal Nurs. 2012;26:343–52. https://doi.org/10.1097/JPN.0b013e318270ffe5.
Shaw RJ, Bernard RS, Storfer-Isser A, Rhine W, Horwitz SM. Parental coping in the neonatal intensive care unit. J Clin Psychol Med Settings. 2013;20:135–42. https://doi.org/10.1007/s10880-012-9328-x.
Persson C, Ericson K, Eriksson M, Salari R, Flacking R. Quality of couple relationship and associated factors in parents of NICU-cared infants during the first year after birth. J Peri. 2024;44:1738–45. https://doi.org/10.1038/s41372-024-02076-1.
Loewenstein K, Barroso J, Phillips S. The experiences of parent dyads in the NICU: a qualitative description. J Pediatr Nurs. 2021;60:1–10. https://doi.org/10.1016/j.pedn.2021.01.023.
Stefana A, Biban P, Padovani EM, Lavelli M. Fathers’ experiences of supporting their partners during their preterm infant’s stay in the neonatal intensive care unit: a multi-method study. J Perinatol. 2022;42:714–22. https://doi.org/10.1038/s41372-021-01195-3.
Gooding JS, Cooper LG, Blaine AI, Franck LS, Howse JL, Berns SD. Family support and family-centered care in the neonatal intensive care unit: origins, advances, impact. Semin Perinatol. 2011;35:20–8. https://doi.org/10.1053/j.semperi.2010.10.004. PMID: 21255703.
Guillaume S, Michelin N, Amrani E, Benier B, Durrmeyer X, Lescure S, et al. Parents’ expectations of staff in the early bonding process with their premature babies in the intensive care setting: a qualitative multicenter study with 60 parents. BMC Pediatr. 2013;13:18 https://doi.org/10.1186/1471-2431-13-18.
Dahan M, Rotteau L, Higazi S, Kwayke O, Lai G, Moulsdale W, et al. Understanding the family context: a qualitative descriptive study of parent and NICU clinician experiences and perspectives. Children. 2023;10:896 https://doi.org/10.3390/children10050896.
Franck LS, Cormier DM, Hutchison J, Moore D, Bisgaard R, Gay C, et al. A multisite survey of NICU healthcare professionals’ perceptions about family-centered care. Adv Neonatal Care. 2021;21:205–13. https://doi.org/10.1097/ANC.0000000000000805.
Labrie NHM, van Veenendaal NR, Ludolph RA, Ket JCF, van der Schoor SRD, van Kempen AAMW. Effects of parent-provider communication during infant hospitalization in the NICU on parents: a systematic review with meta-synthesis and narrative synthesis. Patient Educ Couns. 2021;104:1526–52. https://doi.org/10.1016/j.pec.2021.04.023.
Sigurdson K, Morton C, Mitchell B, et al. Disparities in NICU quality of care: a qualitative study of family and clinician accounts. J Perinatol. 2018;38:600–7. https://doi.org/10.1038/s41372-018-0057-3.
Flemming K, Booth A, Garside R, Tuncalp O, Noyes J. Qualitative evidence synthesis for complex interventions and guideline development: clarification of the purpose, designs, and relevant methods. BMJ Glob Health. 2019;4:e000882 https://doi.org/10.1136/bmjgh-2018-000882.
Hammarberg K, Kirkman M, de Lacey S. Qualitative research methods: when to use them and how to judge them. Hum Reprod. 2016;31:498–501. https://doi.org/10.1093/humrep/dev334.
March of Dimes. PeriStats: United States Maternal and infant health data. marchofdimes.org. (n.d.). Retrieved from https://www.marchofdimes.org/peristats/data?lev=1&obj=1®=25&slev=4&sreg=25&stop=154&top=11
Woźniak W. Homogeneity of focus groups as a pathway to successful research findings? Methodological notes from the fieldwork. Qual Sociol Rev. 2014. https://doi.org/10.18778/1733-8069.10.1.01.
Fereday K, Muir-Cochrane E. Demonstrating rigor using thematic analysis: a hybrid approach of inductive and deductive coding and theme development. Int J Qual Methods. 2006;5:80–92. https://doi.org/10.1177/160940690600500107.
Software: Dedoose Version 9.0.17, cloud application for managing, analyzing, and presenting qualitative and mixed-method research data. 2021. Los Angeles, CA: SocioCultural Research Consultants, LLC. www.dedoose.com.
Hansen K, Davis P, Hubbard DK. Trauma-informed care in the neonatal intensive care unit. J Soc Work End Life Palliat Care. 2023;19:326–35. https://doi.org/10.1080/15524256.2023.2262155.
Forkey J, Szilagyi M, Kelly ET, Duffee J. The Council on Foster Care, Adoption, and Kinship Care, Council on Community Pediatrics, Council on Child Abuse and Neglect, Committee on Psychosocial Aspects of Child and Family Health Trauma-informed care. Pediatrics. 2021;148. e2021052580. https://doi.org/10.1542/peds.2021-052580.
Wang LL, Ma JJ, Meng HH, Zhou J. Mothers’ experiences of neonatal intensive care: a systematic review and implications for clinical practice. World J Clin Cases. 2021;9:7062–72. https://doi.org/10.12998/wjcc.v9.i24.7062.
Ondusko DS, Klawetter S, Hawkins Carter E, Osborne M, Peterson JW, Underwood Carrasco VI, et al. The needs and experiences of black families in the neonatal intensive care unit. Pediatrics. 2025;155:e2024067473. https://doi.org/10.1542/peds.2024-067473.
Witt RE, Malcolm M, Colvin BN, Gill MR, Ofori J, Roy S, et al. Racism and quality of neonatal intensive care: voices of black mothers. Pediatrics. 2022;150:e2022056971. https://doi.org/10.1542/peds.2022-056971.
Karvonen KL, Smith O, Chambers-Butcher B, Afulani P, Mathis-Perry T, Rangwalla K, et al. Parent and staff focus groups to address NICU racial inequities: “There’s radical optimism in that we’re in a different time and we’re not doing it alone.”. J Perinatol. 2025;45:350–8. https://doi.org/10.1038/s41372-024-02063-6.
Grunberg VA, Presciutti A, Vranceanu AM, Lerou PH. Parental self-efficacy and personal time help explain impact of parent-staff interactions on parental distress and bonding in the neonatal intensive care unit. J Pediatr. 2025;276:114300. https://doi.org/10.1016/j.jpeds.2024.114300.
Grunberg VA, Geller PA, Hoffman C, Patterson CA. A biopsychosocial model of NICU family adjustment and child development. J Perinatol. 2023;43:510–7. https://doi.org/10.1038/s41372-022-01585-1.
Soni R, Tscherning C. Family-centered and developmental care on the neonatal unit. Paediatr Child Health. 2021;31:18–23. https://doi.org/10.1016/j.paed.2020.10.003.
Acknowledgements
We want to thank the staff in Newborn Medicine at Massachusetts General Hospital who graciously offered to participate in these interviews.
Funding
VG is supported by a K23 award from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (K23HD110597). A-MV is supported by a K24 award from the National Institute Center for Complementary and Integrative Health (1K24AT011760-01).
Author information
Authors and Affiliations
Contributions
Conceptualization: EB, VG; Data curation: EB, VG; Formal analysis: EB, VG; Investigation: EB, PHL, AMV, VG; Methodology: EB, VG, AMV; Project administration: VG; Funding Support: PHL, VG; Resources: PHL, AMV, VG; Supervision: VG; Roles/Writing—original draft: EB; and Writing—review and editing: EB, VG, PHL, AMV.
Corresponding author
Ethics declarations
Competing interests
We declare no relevant conflicts of interest. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Ethics approval and consent to participate
All methods were performed in accordance with guidelines and regulations. Approval was obtained from the Massachusetts General Hospital Institutional Review Board (Reference number: 2022P002861). Informed consent was obtained from all participants.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Belkin, E.M., Lerou, P.H., Vranceanu, AM. et al. “Each family has a story:” lived experiences of NICU families from staff perspectives. J Perinatol (2025). https://doi.org/10.1038/s41372-025-02435-6
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41372-025-02435-6