Abstract
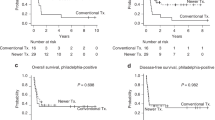
Fit patients with peripheral T-cell lymphoma, not otherwise specified (PTCL-NOS) and angioimmunoblastic T-cell lymphoma (AITL) in relapsed or refractory (R/R) disease status often receive salvage chemotherapy followed by autologous hematopoietic stem cell transplantation (autoHCT) or allogeneic HCT (alloHCT). However, there is no consensus on the type of HCT that should be applied for such patients. Herein, we retrospectively evaluated the survival outcome of 760 adult R/R PTCL-NOS or AITL patients who underwent the first HCT. Among them, 318 relapsed after first remission (REL) and 442 were refractory to the primary therapy (PIF). The 4-year overall survival (OS) of autoHCT and alloHCT was 50 and 50% for REL patients, and 52 and 49% for PIF patients, respectively. In the multivariable analysis, alloHCT tended to be associated with better progression-free survival (PFS) in REL (hazard ratio [HR] 0.74; 95% confidence interval [CI]: 0.53–1.03), and significantly better PFS in PIF (HR 0.64; 95% CI: 0.46–0.88) compared with autoHCT. The subgroup analysis with propensity-score matching showed that alloHCT was associated with better OS for REL-sensitive and PIF-nonremission disease. This study suggested that the advantage of alloHCT for R/R PTCL-NOS or AITL is different, depending on the disease status at HCT.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H (eds). WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. Revised 4th ed. Lyon: International Agency for Research on Cancer (IARC); 2017.
Vose J, Armitage J, Weisenburger D. International T-Cell Lymphoma Project. International peripheral T-cell and natural killer/T-cell lymphoma study: pathology findings and clinical outcomes. J Clin Oncol. 2008;26:4124–30.
de Leval L, Parrens M, Le Bras F, Jais J-P, Fataccioli V, Martin A, et al. Angioimmunoblastic T-cell lymphoma is the most common T-cell lymphoma in two distinct French information data sets. Haematologica. 2015;100:e361–4.
d’Amore F, Gaulard P, Trümper L, Corradini P, Kim W-S, Specht L, et al. Peripheral T-cell lymphomas: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2015;26:v108–15.
Yamaguchi M, Suzuki R. JSH practical guidelines for hematological malignancies, 2018: 7. Peripheral T-cell lymphoma (PTCL). Int J Hematol. 2019;109:137–40.
National Comprehensive Cancer Network. T-Cell Lymphomas (Version 1. 2021). https://www.nccn.org/professionals/physician_gls/pdf/t-cell.pdf. Accessed 6 Apr 2021.
Abramson JS, Feldman T, Kroll-Desrosiers AR, Muffly LS, Winer E, Flowers CR, et al. Peripheral T-cell lymphomas in a large US multicenter cohort: prognostication in the modern era including impact of frontline therapy. Ann Oncol. 2014;25:2211–7.
Fossard G, Broussais F, Coelho I, Bailly S, Nicolas-Virelizier E, Toussaint E, et al. Role of up-front autologous stem-cell transplantation in peripheral T-cell lymphoma for patients in response after induction: an analysis of patients from LYSA centers. Ann Oncol. 2018;29:715–23.
Park SI, Horwitz SM, Foss FM, Pinter-Brown LC, Carson KR, Rosen ST, et al. The role of autologous stem cell transplantation in patients with nodal peripheral T-cell lymphomas in first complete remission: report from COMPLETE, a prospective, multicenter cohort study. Cancer. 2019;125:1507–17.
Mak V, Hamm J, Chhanabhai M, Shenkier T, Klasa R, Sehn LH, et al. Survival of patients with peripheral T-cell lymphoma after first relapse or progression: spectrum of disease and rare long-term survivors. J Clin Oncol. 2013;31:1970–6.
Biasoli I, Cesaretti M, Bellei M, Maiorana A, Bonacorsi G, Quaresima M, et al. Dismal outcome of T-cell lymphoma patients failing first-line treatment: results of a population-based study from the Modena Cancer Registry. Hematol Oncol. 2015;33:147–51.
Bellei M, Foss FM, Shustov AR, Horwitz SM, Marcheselli L, Kim WS, et al. The outcome of peripheral T-cell lymphoma patients failing first-line therapy: a report from the prospective, International T-Cell Project. Haematologica. 2018;103:1191–7.
Chihara D, Fanale MA, Miranda RN, Noorani M, Westin JR, Nastoupil LJ, et al. The survival outcome of patients with relapsed/refractory peripheral T-cell lymphoma-not otherwise specified and angioimmunoblastic T-cell lymphoma. Br J Haematol 2017;176:750–8.
Lansigan F, Horwitz SM, Pinter-Brown LC, Rosen ST, Pro B, Hsi ED, et al. Outcomes for relapsed and refractory peripheral T-cell lymphoma patients after front-line therapy from the COMPLETE registry. Acta Haematol. 2020;143:40–50.
Smith SM, Burns LJ, Inwards DJ, Van Besien K, Wiernik PH, Cairo MS, et al. Hematopoietic cell transplantation for systemic mature T-cell non-Hodgkin lymphoma. J Clin Oncol. 2013;31:3100–9.
Kim SW, Yoon SS, Suzuki R, Matsuno Y, Yi HG, Yoshida T, et al. Comparison of outcomes between autologous and allogeneic hematopoietic stem cell transplantation for peripheral T-cell lymphomas with central review of pathology. Leukemia. 2013;27:1394–7.
Beitinjaneh A, Saliba RM, Medeiros LJ, Turturro F, Rondon G, Korbling M, et al. Comparison of survival in patients with T cell lymphoma after autologous and allogeneic stem cell transplantation as a frontline strategy or in relapsed disease. Biol Blood Marrow Transplant. 2015;21:855–9.
Huang H, Jiang Y, Wang Q, Guo L, Jin Z, Fu Z, et al. Outcome of allogeneic and autologous hematopoietic cell transplantation for high-risk peripheral T cell lymphomas: a retrospective analysis from a chinese center. Biol Blood Marrow Transplant. 2017;23:1393–7.
Atsuta Y, Suzuki R, Yoshimi A, Gondo H, Tanaka J, Hiraoka A, et al. Unification of hematopoietic stem cell transplantation registries in Japan and establishment of the TRUMP System. Int J Hematol. 2007;86:269–74.
Atsuta Y. Introduction of transplant registry unified management program 2 (TRUMP2): scripts for TRUMP data analyses, part I (variables other than HLA-related data). Int J Hematol. 2016;103:3–10.
Cheson BD, Horning SJ, Coiffier B, Shipp MA, Fisher RI, Connors JM, et al. Report of an international workshop to standardize response criteria for non-Hodgkin’s lymphomas. NCI Sponsored International Working Group. J Clin Oncol. 1999;17:1244.
Cheson BD, Pfistner B, Juweid ME, Gascoyne RD, Specht L, Horning SJ, et al. Revised response criteria for malignant lymphoma. J Clin Oncol. 2007;25:579–86.
Giralt S, Ballen K, Rizzo D, Bacigalupo A, Horowitz M, Pasquini M, et al. Reduced-intensity conditioning regimen workshop: defining the dose spectrum. Report of a workshop convened by the center for international blood and marrow transplant research. Biol Blood Marrow Transplant. 2009;15:367–9.
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J, et al. 1994 consensus conference on acute GVHD grading. Bone Marrow Transplant. 1995;15:825–8.
Shulman HM, Sullivan KM, Weiden PL, McDonald GB, Striker GE, Sale GE, et al. Chronic graft-versus-host syndrome in man. A long-term clinicopathologic study of 20 Seattle patients. Am J Med. 1980;69:204–17.
Filipovich AH, Weisdorf D, Pavletic S, Socie G, Wingard JR, Lee SJ, et al. National Institutes of Health consensus development project on criteria for clinical trials in chronic graft-versus-host disease: I. Diagnosis and staging working group report. Biol Blood Marrow Transplant. 2005;11:945–56.
Rothman KJ. No adjustments are needed for multiple comparisons. Epidemiology. 1990;1:43–6.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48:452–8.
Schmitz N, Truemper LH, Bouabdallah K, Ziepert M, Leclerc M, Cartron G, et al. A randomized phase 3 trial of autologous vs allogeneic transplantation as part of first-line therapy in poor-risk peripheral T-NHL. Blood. 2021;137:2646–56.
Epperla N, Ahn KW, Litovich C, Ahmed S, Battiwalla M, Cohen JB, et al. Allogeneic hematopoietic cell transplantation provides effective salvage despite refractory disease or failed prior autologous transplant in angioimmunoblastic T-cell lymphoma: a CIBMTR analysis. J Hematol Oncol. 2019;12:1–11.
Schmitz N, Lenz G, Stelljes M. Allogeneic hematopoietic stem cell transplantation (HSCT) for T-cell lymphomas. Blood. 2018;132:245–53.
Le Gouill S, Milpied N, Buzyn A, De Latour RP, Vernant JP, Mohty M, et al. Graft-versus-lymphoma effect for aggressive T-cell lymphomas in adults: a study by the Société Française de Greffe de Moëlle et de Thérapie Cellulaire. J Clin Oncol. 2008;26:2264–71.
Dodero A, Spina F, Narni F, Patriarca F, Cavattoni I, Benedetti F, et al. Allogeneic transplantation following a reduced-intensity conditioning regimen in relapsed/refractory peripheral T-cell lymphomas: long-term remissions and response to donor lymphocyte infusions support the role of a graft-versus-lymphoma effect. Leukemia. 2012;26:520–6.
Jacobsen ED, Kim HT, Ho VT, Cutler CS, Koreth J, Fisher DC, et al. A large single-center experience with allogeneic stem-cell transplantation for peripheral T-cell non-Hodgkin lymphoma and advanced mycosis fungoides/Sezary syndrome. Ann Oncol. 2011;22:1608–13.
Mamez A-C, Dupont A, Blaise D, Chevallier P, Forcade E, Ceballos P, et al. Allogeneic stem cell transplantation for peripheral T cell lymphomas: a retrospective study in 285 patients from the Société Francophone de Greffe de Moelle et de Thérapie Cellulaire (SFGM-TC). J Hematol Oncol. 2020;13:56.
Feyler S, Prince HM, Pearce R, Towlson K, Nivison-Smith I, Schey S, et al. The role of high-dose therapy and stem cell rescue in the management of T-cell malignant lymphomas: a BSBMT and ABMTRR study. Bone Marrow Transplant. 2007;40:443–50.
Loirat M, Chevallier P, Leux C, Moreau A, Bossard C, Guillaume T, et al. Upfront allogeneic stem-cell transplantation for patients with nonlocalized untreated peripheral T-cell lymphoma: an intention-to-treat analysis from a single center. Ann Oncol. 2015;26:386–92.
Tarella C, Gueli A, Delaini F, Rossi A, Barbui AM, Gritti G, et al. Rate of primary refractory disease in B and T-cell non-Hodgkin’s lymphoma: correlation with long-term survival. PLoS ONE. 2014;9:e106745.
Kyriakou C, Canals C, Finke J, Kobbe G, Harousseau JL, Kolb HJ, et al. Allogeneic stem cell transplantation is able to induce long-term remissions in angioimmunoblastic T-cell lymphoma: a retrospective study from the lymphoma working party of the European group for blood and marrow transplantation. J Clin Oncol. 2009;27:3951–8.
Mehta-Shah N, Kommalapati A, Teja S, Cashen AF, Dahi PB, Sauter CS, et al. Successful treatment of mature T-cell lymphoma with allogeneic stem cell transplantation: the largest multicenter retrospective analysis. Blood. 2020;136:35–6.
Acknowledgements
The authors greatly appreciate the physicians and data managers of the JSTCT centers for providing excellent patient care and reporting clinical data to the TRUMP. We also thank the members of The Japanese Data Center for HCT for their dedicated data management. We thank H. Nikki March, PhD, from Edanz (https://jp.edanz.com/ac) for language editing a draft of this paper.
Funding
This work was supported in part by the Practical Research Project for Allergic Diseases and Immunology (Research Technology of Medical Transplantation) from the Japan Agency for Medical Research and Development, AMED (19ek0510023h) (to Y.A.), Grants-in-Aid for Scientific Research from the Japan Society for the Promotion of Science (20J14747), Jichi Medical University Graduate Student Research Award 2021, and Japan Leukemia Research Award (to K. Kameda).
Author information
Authors and Affiliations
Contributions
K. Kameda, S.K., S.-W.K. and E.K. designed the study. K. Kameda performed analyses and wrote the first draft of the paper. S.K., S.-W.K., Y.U., and K. Kato reviewed and revised the paper. T.F., N.U., H.K., T.W., E.S., S.Y., K. I., M.N., T.I., S.F., J.I., and H.S. are the leading physicians at each institution that made significant contributions to provision of data to the TRUMP. J.K., T.K., T.I., and Y.A. collected and assembled data. All authors discussed the results, interpreted the data, and approved the final version of the paper.
Corresponding author
Ethics declarations
Competing interests
Conflicts of interest disclosure: K. Kato is a consultant for, and has received research funding from AbbVie, Chugai Pharmaceutical Co., Ltd., Daiichi Sankyo, Eisai, and Novartis; is a consultant for AstraZeneca; has received honoraria and research funding from Bristol-Myers Squibb, Kyowa Kirin, and Ono; is a consultant and has received honoraria and research funding from Celgene, Janssen; has received honoraria from Sumitomo Dainippon Pharma Co., Ltd., NSD, Mundi, outside the submitted work. K.I. has received honoraria from Chugai Pharmaceutical Co., Ltd., Kyowa Hakko Kirin Co., Ltd., Novartis Pharma K.K., Celgene Co., Ltd., Bristol-Myers Squibb K.K., Takeda Pharmaceutical Co. Ltd., Nippon Shinyaku Co., Ltd., Otuka Pharmaceutical Co. Ltd., Astellas Pharma Inc., and Sumitomo Dainippon Pharma Co., Ltd., outside the submitted work. S.F. has received honoraria from Takeda Pharmaceutical Co., Ltd., Ono Pharmaceutical Co., Ltd., Janssen Pharmaceutical K.K., Sanofi, Bristol-Myers Squibb Co., Ltd., and Celgene Co., Ltd., outside the submitted work. T.I. reports research funding from Astellas Pharma, Chugai Pharmaceutical Co., CSL Behring, Eisai Co., FUJIFILM Wako Chemicals., Kyowa Kirin Co., Ono Pharmaceutical Co., Pfizer, Nippon Shinyaku Co., Abbvie, Otsuka Pharmaceutical Co., Repertoire Genesis Inc., Sumitomo Dainippon Pharma Co., Taiho Pharmaceutical Co., Takara Bio Inc., Takeda Pharmaceutical Co., and Zenyaku Kogyo Co., honoraria from Bristol-Myers Squibb, Celgene, Janssen Pharmaceutical K.K., Kyowa Kirin Co., Takeda Pharmaceutical Co., CSL Behring, Astellas Pharma, Eisai Co., Novartis, FUJIFILM Wako Chemicals., Nippon Shinyaku Co., and Repertoire Genesis Inc., outside the submitted work. E.K. has received honoraria from Takeda Pharmaceutical Co and Sumitomo Dainippon Pharma Co, outside the submitted work. The remaining authors declare no competing financial interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Prior presentation Partially presented in an oral presentation at the EHA2021 Virtual Congress, June 9–17, 2021 (abstract S244).
Supplementary information
Rights and permissions
About this article
Cite this article
Kameda, K., Kako, S., Kim, SW. et al. Autologous or allogeneic hematopoietic cell transplantation for relapsed or refractory PTCL-NOS or AITL. Leukemia 36, 1361–1370 (2022). https://doi.org/10.1038/s41375-022-01545-w
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41375-022-01545-w
This article is cited by
-
Intermediate-dose TBI/fludarabine conditioning for allogeneic hematopoietic cell transplantation in patients with peripheral T-cell lymphoma
Bone Marrow Transplantation (2025)
-
Unusual peripheral T-cell lymphoma with a cytotoxic phenotype presenting in the pancreas
Annals of Hematology (2025)
-
Current status of hematopoietic cell transplantation in patients with peripheral T-cell lymphoma including adult T-cell leukemia–lymphoma
International Journal of Hematology (2025)
-
Therapie der nodalen peripheren T-Zell-Lymphome
Die Onkologie (2025)
-
Advances in the pathogenesis and therapeutic strategies of angioimmunoblastic T-cell lymphoma
Clinical and Experimental Medicine (2023)