Abstract
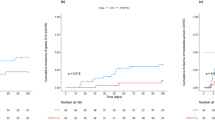
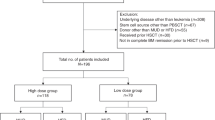
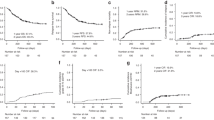
The effects of donor characteristics on outcomes after T-cell-replete (TCR) haploidentical donor peripheral blood stem cell transplantation (PBSCT) with post-transplant cyclophosphamide (PTCy) or low-dose antithymocyte globulin (ATG) remain unclear. We evaluated the impact in 1,677 patients who received a PTCy protocol (PTCy-haplo; n = 1,107) or low-dose ATG protocol (ATG-haplo; n = 570). A low CD34+ cell dose (<4 ×106/kg) was the only donor characteristic associated with worse overall survival (OS) after PTCy-haplo (adjusted hazard ratios [aHR] = 1.49, P = 0.008), whereas increasing donor age by decade (aHR = 1.12, P = 0.008) and human leukocyte antigen 2-3 antigen mismatches (aHR = 1.46, P = 0.010), compared to HLA 0-1 antigen mismatches, were associated with worse OS after ATG-haplo. Increasing donor age was associated with a high risk of grade III–IV acute GVHD both after PTCy-haplo (HR: 1.32, P = 0.009) and ATG-haplo (HR: 1.22, P = 0.006). Offspring donors had better relapse-free survival and GVHD-free relapse-free survival than sibling donors after ATG-haplo. Our data highlights the donor characteristics associated with improved transplant outcomes after TCR haploidentical donor PBSCT with PTCy or low-dose ATG.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author, JK, upon reasonable request.
References
Wang Y, Chang YJ, Xu LP, Liu KY, Liu DH, Zhang XH, et al. Who is the best donor for a related HLA haplotype-mismatched transplant? Blood. 2014;124:843–50.
Chang YJ, Luznik L, Fuchs EJ, Huang XJ. How do we choose the best donor for T-cell- replete, HLA-haploidentical transplantation? J Hematol Oncol. 2016;9:35.
Wang Y, Wu DP, Liu QF, Xu LP, Liu KY, Zhang XH, et al. Donor and recipient age, gender and ABO incompatibility regardless of donor source: validated criteria for donor selection for haematopoietic transplants. Leukemia. 2018;32:492–8.
Ciurea SO, Al Malki MM, Kongtim P, Fuchs EJ, Luznik L, Huang XJ, et al. The European Society for Blood and Marrow Transplantation (EBMT) consensus recommendations for donor selection in haploidentical hematopoietic cell transplantation. Bone Marrow Transpl. 2020;55:12–24.
Fuchs EJ. Haploidentical transplantation for hematologic malignancies: where do we stand? Hematol Am Soc Hematol Educ Program. 2012;2012:230–6.
Kanakry CG, Fuchs EJ, Luznik L. Modern approaches to HLA-haploidentical blood or marrow transplantation. Nat Rev Clin Oncol. 2016;13:10–24.
Luznik L, O’Donnell PV, Symons HJ, Chen AR, Leffell MS, Zahurak M, et al. HLA- haploidentical bone marrow transplantation for hematologic malignancies using nonmyeloablative conditioning and high-dose, posttransplantation cyclophosphamide. Biol Blood Marrow Transpl. 2008;14:641–50.
McCurdy SR, Kanakry JA, Showel MM, Tsai HL, Bolanos-Meade J, Rosner GL, et al. Risk- stratified outcomes of nonmyeloablative HLA-haploidentical BMT with high-dose posttransplantation cyclophosphamide. Blood. 2015;125:3024–31.
Bashey A, Zhang MJ, McCurdy SR, St Martin A, Argall T, Anasetti C, et al. Mobilized peripheral blood stem cells versus unstimulated bone marrow as a graft source for T-cell-replete haploidentical donor transplantation using post-transplant Cyclophosphamide. J Clin Oncol. 2017;35:3002.
Sugita J, Kawashima N, Fujisaki T, Kakihana K, Ota S, Matsuo K, et al. HLA-Haploidentical peripheral blood stem cell transplantation with post-transplant Cyclophosphamide after Busulfan-containing reduced-intensity conditioning. Biol Blood Marrow Transpl. 2015;21:1646–52.
Huselton E, Slade M, Trinkaus KM, DiPersio JF, Westervelt P, Romee R. Propensity score analysis of conditioning intensity in peripheral blood haploidentical hematopoietic cell transplantation. Biol Blood Marrow Transpl. 2018;24:2047–55.
Sugita J, Kagaya Y, Miyamoto T, Shibasaki Y, Nagafuji K, Ota S, et al. Myeloablative and reduced-intensity conditioning in HLA-haploidentical peripheral blood stem cell transplantation using post-transplant cyclophosphamide. Bone Marrow Transpl. 2019;54:432–41
Lee KH, Lee JH, Lee JH, Kim DY, Seol M, Lee YS, et al. Reduced-intensity conditioning therapy with busulfan, fludarabine, and antithymocyte globulin for HLA-haploidentical hematopoietic cell transplantation in acute leukemia and myelodysplastic syndrome. Blood. 2011;118:2609–17.
Huang XJ, Liu DH, Liu KY, Xu LP, Chen H, Han W, et al. Haploidentical hematopoietic stem cell transplantation without in vitro T-cell depletion for the treatment of hematological malignancies. Bone Marrow Transpl. 2006;38:291–7.
Lu DP, Dong L, Wu T, Huang XJ, Zhang MJ, Han W, et al. Conditioning including antithymocyte globulin followed by unmanipulated HLA-mismatched/haploidentical blood and marrow transplantation can achieve comparable outcomes with HLA- identical sibling transplantation. Blood. 2006;107:3065–73.
Huang XJ, Chang YJ. Unmanipulated HLA-mismatched/haploidentical blood and marrow hematopoietic stem cell transplantation. Biol Blood Marrow Transpl. 2011;17:197–204.
Nagler A, Kanate AS, Labopin M, Ciceri F, Angelucci E, Koc Y, et al. Post-transplant cyclophosphamide versus anti-thymocyte globulin for graft-versus-host disease prevention in haploidentical transplantation for adult acute lymphoblastic leukemia. Haematologica 2020;30.
Ruggeri A, Sun Y, Labopin M, Bacigalupo A, Lorentino F, Arcese W, et al. Post-transplant cyclophosphamide versus anti-thymocyte globulin as graft- versus-host disease prophylaxis in haploidentical transplant. Haematologica. 2017;102:401–10.
Kako S, Akahoshi Y, Harada N, Nakano H, Kameda K, Ugai T, et al. HLA-mismatched haploidentical transplantation using low-dose anti-thymocyte globulin (ATG: thymoglobulin). Hematology. 2017;22:129–35.
Cho BS, Yoon JH, Shin SH, Yahng SA, Lee SE, Eom KS, et al. Comparison of allogeneic stem cell transplantation from familial-mismatched/haploidentical donors and from unrelated donors in adults with high-risk acute myelogenous leukemia. Biol Blood Marrow Transpl. 2012;18:1552–63.
Ikegame K, Yoshida T, Yoshihara S, Daimon T, Shimizu H, Maeda Y, et al. Unmanipulated Haploidentical reduced-intensity stem cell transplantation using Fludarabine, Busulfan, low-dose Antithymocyte Globulin, and steroids for patients in non-complete remission or at high risk of relapse: a prospective multicenter Phase I/II Study in Japan. Biol Blood Marrow Transpl. 2015;21:1495–505.
Ogawa H, Ikegame K, Yoshihara S, Kawakami M, Fujioka T, Masuda T, et al. Unmanipulated HLA 2-3 antigen-mismatched (haploidentical) stem cell transplantation using nonmyeloablative conditioning. Biol Blood Marrow Transpl. 2006;12:1073–84.
Ikegame K, Kaida K, Fukunaga K, Osugi Y, Yoshihara K, Yoshihara S, et al. Allogeneic hematopoietic stem cell transplantation from a 2-HLA-haplotype-mismatched family donor for posttransplant relapse: a prospective phase I/II study. Bone Marrow Transpl. 2021;56:70–83.
Wada F, Watanabe M, Konuma T, Okabe M, Kobayashi S, Uchida N, et al. HLA 1-3 antigen-mismatched related peripheral blood stem cells transplantation using low-dose antithymocyte globulin versus unrelated cord blood transplantation. Am J Hematol. 2022;97:311–21.
Kanda J, Ando T, Kimura SI, Fujiwara SI, Imada K, Fujisawa S, et al. Hematopoietic stem cell transplantation from a related donor with human leukocyte Antigen 1-antigen mismatch in the graft-versus-host direction using low-dose anti-thymocyte globulin. Cell Transpl. 2020;29:963689720976567.
Giralt S, Ballen K, Rizzo D, Bacigalupo A, Horowitz M, Pasquini M, et al. Reduced- intensity conditioning regimen workshop: defining the dose spectrum. Report of a workshop convened by the center for international blood and marrow transplant research. Biol Blood Marrow Transpl. 2009;15:367–9.
Kanda J, Morishima Y, Terakura S, Wake A, Uchida N, Takahashi S, et al. Impact of graft- versus-host disease on outcomes after unrelated cord blood transplantation. Leukemia. 2017;31:663–8.
Wada F, Kanda J, Watanabe M, Arai Y, Hishizawa M, Kondo T, et al. Favorable outcomes after single cord blood transplantation for patients with high-risk hematologic diseases: a single-institute retrospective analysis. Transpl Cell Ther. 2021;27:495.e1-495.e9.
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J, et al. 1994 Consensus Conference on Acute GVHD Grading. Bone Marrow Transpl. 1995;15:825–8.
Sullivan KM, Agura E, Anasetti C, Appelbaum F, Badger C, Bearman S, et al. Chronic graft-versus-host disease and other late complications of bone marrow transplantation. Semin Hematol. 1991;28:250–9.
Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94:496–509.
Kurth T, Walker AM, Glynn RJ, Chan KA, Gaziano JM, Berger K, et al. Results of multivariable logistic regression, propensity matching, propensity adjustment, and propensity-based weighting under conditions of nonuniform effect. Am J Epidemiol. 2006;163:262–70.
Austin PC. The performance of different propensity score methods for estimating marginal hazard ratios. Stat Med. 2013;32:2837–49.
McCurdy SR, Zhang MJ, St Martin A, Al Malki MM, Bashey A, Gaballa S, et al. Effect of donor characteristics on haploidentical transplantation with posttransplantation cyclophosphamide. Blood Adv. 2018;2:299–307.
Solomon SR, Aubrey MT, Zhang X, Piluso A, Freed BM, Brown S, et al. Selecting the best donor for haploidentical transplant: Impact of HLA, killer cell immunoglobulin-like receptor genotyping, and other clinical variables. Biol Blood Marrow Transpl. 2018;24:789–98.
Mariotti J, Raiola AM, Evangelista A, Carella AM, Martino M, Patriarca F, et al. Impact of donor age and kinship on clinical outcomes after T-cell-replete haploidentical transplantation with PT-Cy. Blood Adv. 2020;4:3900–12.
Kollman C, Howe CWS, Anasetti C, Antin JH, Davies SM, Filipovich AH, et al. Donor characteristics as risk factors in recipients after transplantation of bone marrow from unrelated donors: the effect of donor age. Blood. 2001;98:2043–51.
Kollman C, Spellman SR, Zhang MJ, Hassebroek A, Anasetti C, Antin JH, et al. The effect of donor characteristics on survival after unrelated donor transplantation for hematologic malignancy. Blood. 2016;127:260–7.
Maffini E, Labopin M, Blaise D, Ciceri F, Gulbas Z, Deconinck E, et al. CD34+ cell dose effects on clinical outcomes after T-cell replete haploidentical allogeneic hematopoietic stem cell transplantation for acute myeloid leukemia using peripheral blood stem cells. A study from the acute leukemia working Party of the European Society for blood and marrow transplantation (EBMT). Am J Hematol. 2020;95:892–9.
Elmariah H, Naqvi SMH, Kim J, Nishihori T, Mishra A, Perez L, et al. Impact of infused CD34+ stem cell dosing for allogeneic peripheral blood stem cell transplantation with post-transplant cyclophosphamide. Bone Marrow Transpl. 2021;56:1683–90.
Pedraza A, Salas MQ, Rodriguez-Lobato LG, Charry P, Suarez-Lledo M, Martinez-Cibrian N, et al. Effect of CD34(+) cell dose on the outcomes of allogeneic stem cell transplantation with post-transplantation Cyclophosphamide. Transpl Cell Ther. 2023;29:181.e1-181.e10.
Styczynski J. WhO is the patient at risk of CMV recurrence: a review of the current scientific evidence with a focus on hematopoietic cell transplantation. Infect Dis Ther. 2018;7:1–16.
Ljungman P, de la Camara R, Robin C, Crocchiolo R, Einsele H, Hill JA, et al. Guidelines for the management of cytomegalovirus infection in patients with haematological malignancies and after stem cell transplantation from the 2017 European Conference on Infections in Leukaemia (ECIL 7). Lancet Infect Dis. 2019;19:e260–e272.
Schmidt-Hieber M, Labopin M, Beelen D, Volin L, Ehninger G, Finke J, et al. CMV serostatus still has an important prognostic impact in de novo acute leukemia patients after allogeneic stem cell transplantation: a report from the Acute Leukemia Working Party of EBMT. Blood. 2013;122:3359–64.
Ljungman P, Brand R, Einsele H, Frassoni F, Niederwieser D, Cordonnier C. Donor CMV serologic status and outcome of CMV-seropositive recipients after unrelated donor stem cell transplantation: an EBMT megafile analysis. Blood. 2003;102:4255–60.
van Rood JJ, Loberiza FR Jr, Zhang MJ, Oudshoorn M, Claas F, Cairo MS, et al. Effect of tolerance to noninherited maternal antigens on the occurrence of graft-versus-host disease after bone marrow transplantation from a parent or an HLA-haploidentical sibling. Blood. 2002;99:1572–7.
Ichinohe T, Uchiyama T, Shimazaki C, Matsuo K, Tamaki S, Hino M, et al. Feasibility of HLA-haploidentical hematopoietic stem cell transplantation between noninherited maternal antigen (NIMA)-mismatched family members linked with long-term fetomaternal microchimerism. Blood. 2004;104:3821–8.
Stern M, Ruggeri L, Mancusi A, Bernardo ME, de Angelis C, Bucher C, et al. Survival after T cell-depleted haploidentical stem cell transplantation is improved using the mother as donor. Blood. 2008;112:2990–5.
Elmariah H, Kasamon YL, Zahurak M, Macfarlane KW, Tucker N, Rosner GL, et al. Haploidentical bone marrow transplantation with post-transplant cyclophosphamide using non-first-degree related donors. Biol Blood Marrow Transpl. 2018;24:1099–102.
Ye Y, Wang M, Malard F, Shi J, Lu Y, Ouyang G, et al. Comparison of non-first-degree related donors and first-degree related donors in haploidentical HSCT: a multi-centre retrospective analysis. Bone Marrow Transpl. 2021;56:2567–74.
Luo Y, Xiao H, Lai X, Shi J, Tan Y, He J, et al. T-cell-replete haploidentical HSCT with low-dose anti-T-lymphocyte globulin compared with matched sibling HSCT and unrelated HSCT. Blood. 2014;124:2735–43.
Ye Y, Labopin M, Chen J, Gulbas Z, Zhang X, Koc Y, et al. Similar outcomes following non-first-degree and first-degree related donor haploidentical hematopoietic cell transplantation for acute leukemia patients in complete remission: a study from the Global Committee and the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation. J Hematol Oncol. 2023;16:25.
Fuchs EJ, McCurdy SR, Solomon SR, Wang T, Herr MM, Modi D, et al. HLA informs risk predictions after haploidentical stem cell transplantation with posttransplantation cyclophosphamide. Blood. 2022;139:1452–68.
Lorentino F, Labopin M, Fleischhauer K, Ciceri F, Mueller CR, Ruggeri A, et al. The impact of HLA matching on outcomes of unmanipulated haploidentical HSCT is modulated by GVHD prophylaxis. Blood Adv. 2017;1:669–80.
Morishima Y, Morishita Y, Tanimoto M, Ohno R, Saito H, Horibe K, et al. Low incidence of acute graft-versus-host disease by the administration of methotrexate and cyclosporine in Japanese leukemia patients after bone marrow transplantation from human leukocyte antigen compatible siblings; possible role of genetic homogeneity. The Nagoya Bone Marrow Transplantation Group. Blood. 1989;74:2252–6.
Morishima S, Ogawa S, Matsubara A, Kawase T, Nannya Y, Kashiwase K, et al. Impact of highly conserved HLA haplotype on acute graft-versus-host disease. Blood. 2010;115:4664–70.
Inamoto Y, White J, Ito R, Martin PJ, Fatobene G, Ito A, et al. Comparison of characteristics and outcomes of late acute and NIH chronic GVHD between Japanese and white patients. Blood Adv. 2019;3:2764–77.
Ciurea SO, Cao K, Fernandez-Vina M, Kongtim P, Malki MA, Fuchs E, et al. The European Society for Blood and Marrow Transplantation (EBMT) Consensus Guidelines for the Detection and Treatment of Donor-specific Anti-HLA Antibodies (DSA) in Haploidentical Hematopoietic Cell Transplantation. Bone Marrow Transpl. 2018;53:521–34.
Acknowledgements
We thank all the physicians and data managers at the centers who contributed to the collection of data on transplantation for the Japanese Society for Transplantation and Cellular Therapy (JSTCT) and the Transplant Registry Unified Management Program (TRUMP) 2. We also thank the members of the Data Management Committees of the JSTCT and TRUMP for their assistance.
Funding
This work was supported in part by the Takeda Science Foundation (JK) and JSPS KAKENHI Grant number 24K11515 (JK).
Author information
Authors and Affiliations
Contributions
F.W. and J.K. designed the study, reviewed and analyzed data, and wrote the first draft of the manuscript. M.I., M.H., K.K. (Koji Kawamura), and H.N. interpreted data and revised the manuscript; and K.K. (Katsuji Kaida), N.D., H.N., Y.H., T.F., T.E., N.H., Y.M., K.N., S.O., J.I., T.A., T.I., and Y.A. contributed to data collection. All authors approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
This study was approved by the Data Management Committee of the Japanese Data Center for Hematopoietic Cell Transplantation (JDCHCT) and the Ethics Committee of Kyoto University (approval number: R1437).
Patient consent
Informed consent was obtained from all patients.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wada, F., Iwasaki, M., Hirayama, M. et al. Donor selection in T-cell-replete haploidentical donor peripheral blood stem cell transplantation. Leukemia 39, 951–961 (2025). https://doi.org/10.1038/s41375-025-02538-1
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41375-025-02538-1