Abstract
With the advent of deep space exploration and ambitious plans to return humans to the Moon and journey onward to Mars, humans will face exposure to ionizing radiation beyond Earth’s atmosphere and magnetosphere. This is particularly concerning for the hematopoietic system that is sensitive to galactic cosmic rays (GCRs) during interplanetary missions. Epidemiological studies and animal studies implicate that exposure to ionizing radiation can cause leukemias, with recent consensus showing that almost all types of leukemias, even chronic lymphocytic leukemia, can be caused by ionizing radiation despite previous controversies. The possible deleterious effects of deep space travel on the formation, development, etiology, and pathophysiology of hematologic malignancies, specifically leukemias, remain largely unclear. The mechanism(s) by which ionizing radiations cause leukemia differs for different leukemia types and is poorly understood in the spaceflight environment, posing a serious health risk for future astronauts. This paper provides a comprehensive review of the various studies and evidence available on Earth and in space assessing the relationship between ionizing radiation and increased risk of leukemia. We also discuss the unique characteristics of leukemia in space, ethical considerations, risk assessments and potential challenges this may bring to astronauts and healthcare professionals as humanity continues to explore the cosmos.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Antonsen EL, Connell E, Anton W, Reynolds RJ, Buckland DM, Van Baalen M. Updates to the NASA human system risk management process for space exploration. Npj Microgr. 2023;9:72.
Simpson JA. Elemental and isotopic composition of the galactic cosmic-rays. Annu Rev Nucl Part S. 1983;33:323–81.
Chancellor JC, Scott GB, Sutton JP. Space radiation: the number one risk to astronaut health beyond Low Earth Orbit. Life (Basel). 2014;4:491–510.
Kato K, Omori A, Kashiwakura I. Radiosensitivity of human haematopoietic stem/progenitor cells. J Radio Prot. 2013;33:71–80.
Almeida-Porada G, Rodman C, Kuhlman B, Brudvik E, Moon J, George S, et al. Exposure of the bone marrow microenvironment to simulated solar and galactic cosmic radiation induces biological bystander effects on human hematopoiesis. Stem Cells Dev. 2018;27:1237–56.
Little MP, Wakeford R, Zablotska LB, Borrego D, Griffin KT, Allodji RS, et al. Radiation exposure and leukaemia risk among cohorts of persons exposed to low and moderate doses of external ionising radiation in childhood. Brit J Cancer. 2023;129:1152–65.
Brenner DJ, Doll R, Goodhead DT, Hall EJ, Land CE, Little JB, et al. Cancer risks attributable to low doses of ionizing radiation: Assessing what we really know. P Natl Acad Sci USA. 2003;100:13761–6.
Liu H, Schaal D, Curry H, Clark R, Magliari A, Kupelian P, et al. Review of cone beam computed tomography based online adaptive radiotherapy: current trend and future direction. Radiat Oncol. 2023;18:144.
Iliopoulos P, Simopoulou F, Simopoulos V, Kyrgias G, Theodorou K Review on Cone Beam Computed Tomography (CBCT) Dose in Patients Undergoing Image Guided Radiotherapy (IGRT). Advances in Dosimetry and New Trends in Radiopharmaceuticals. IntechOpen2023.
Filippi AR, Vanoni V, Meduri B, Cozzi L, Scorsetti M, Ricardi U, et al. Intensity modulated radiation therapy and second cancer risk in adults. Int J Radiat Oncol Biol Phys. 2018;100:17–20.
Durante M, Cucinotta FA. Physical basis of radiation protection in space travel. Rev Mod Phys. 2011;83:1245–81.
Fogtman A, Baatout S, Baselet B, Berger T, Hellweg CE, Jiggens P, et al. Towards sustainable human space exploration-priorities for radiation research to quantify and mitigate radiation risks. Npj Microgr. 2023;9:8.
Restier-Verlet J, El-Nachef L, Ferlazzo ML, Al-Choboq J, Granzotto A, Bouchet A, et al. Radiation on Earth or in Space: What does it change? Int J Mol Sci. 2021;22:3739.
Norbury JW. Perspective on space radiation for space flights in 2020-2040. Adv Space Res. 2011;47:611–21.
Benton ER, Benton E. Space radiation dosimetry in low-Earth orbit and beyond. Nucl Instrum Meth B. 2001;184:255–94.
Bailey JV Radiation protection and instrumentation. Biomedical Results of Apollo, vol. NASA-SP-368. National Aeronautics and Space Administration; 1975.
Welsh JS, Bevelacqua JJ, Mortazavi SMJ. Ramsar, Iran, as a Natural Radiobiological Surrogate for Mars. Health Phys. 2022;122:508–12.
Sohrabi M, Babapouran M. New public dose assessment from internal and external exposures in low- and elevated-level natural radiation areas of Ramsar, Iran. International Congr Ser. 2005;1276:169–74.
Ghiassi-nejad M, Mortazavi SM, Cameron JR, Niroomand-rad A, Karam PA. Very high background radiation areas of Ramsar, Iran: preliminary biological studies. Health Phys. 2002;82:87–93.
Movahedi A, Mostajaboddavati M, Rajabibazl M, Mirfakhraie R, Enferadi M. Association of telomere length with chronic exposure to ionizing radiation among inhabitants of natural high background radiation areas of Ramsar, Iran. Int J Radiat Biol. 2019;95:1113–21.
Mortazavi SMJ, Mortazavi G, Mortazavi SAR, Paknahad M. Is induction of anomalies in lymphocytes of the residents of high background radiation areas associated with increased cancer risk?. J Biomed Phys Eng. 2019;9:367–72.
Nawotniak SEK, Miller MJ, Stevens AH, Marquez JJ, Payler SJ, Brady AL, et al. Opportunities and challenges of promoting scientific dialog throughout execution of future science-driven extravehicular activity. Astrobiology. 2019;19:426–39.
Zeitlin C, Hassler DM, Cucinotta FA, Ehresmann B, Wimmer-Schweingruber RF, Brinza DE, et al. Measurements of energetic particle radiation in transit to Mars on the Mars science laboratory. Science. 2013;340:1080–4.
Hassler DM, Zeitlin C, Wimmer-Schweingruber RF, Ehresmann B, Rafkin S, Eigenbrode JL, et al. Mars’ surface radiation environment measured with the mars science laboratory’s curiosity rover. Science 2014;343:1244797.
Rizzo A, Borra EM, Ciciani L, Di Fino L, Romoli G, Amantini GS, et al. Foundations of radiological protection in space: the integrated multidisciplinary approach for next manned missions in deep space. Eur Phys J Plus. 2023;138:1001.
U.S. Nuclear Regulatory Commission. Doses in Our Daily Lives. 2022 [cited; Available from: https://www.nrc.gov/about-nrc/radiation/around-us/doses-daily-lives.html.
Jagannathan-Bogdan M, Zon LI. Hematopoiesis. Development. 2013;140:2463–7.
Finch SC. Radiation-induced leukemia: Lessons from history. Best Pr Res Cl Ha. 2007;20:109–18.
Gale RP, Hochhaus A. To Mars and beyond. Space exploration and space medicine in Leukemia. Leukemia 2024;38:1869.
Shah DJ, Sachs RK, Wilson DJ. Radiation-induced cancer: a modern view. Brit J Radio. 2012;85:E1166–E1173.
Muhsen IN, Zubair AC, Niederwieser T, Hashmi SK. Space exploration and cancer: the risks of deeper space adventures. Leukemia. 2024;38:1872-75.
Guo Z, Zhou GM, Hu WT. Carcinogenesis induced by space radiation: A systematic review. Neoplasia 2022;32:100828.
Kwok M, Agathanggelou A, Stankovic T. DNA damage response defects in hematologic malignancies: mechanistic insights and therapeutic strategies. Blood. 2024;143:2123–44.
Nishibuchi I, Tashiro S. DNA double-strand break repair capacity and normal tissue toxicity induced by radiotherapy. J Radiat Res. 2024;65:i52–i56.
Milder CM, Elgart SR, Chappell L, Charvat JM, Van Baalen M, Huff JL, et al. Cancer risk in astronauts: a constellation of uncommon consequences; 2016. Report No.: 20160014586.
Zhang YM, Chen XL, Wang XM, Chen J, Du CH, Wang JP, et al. Insights into ionizing radiation-induced bone marrow hematopoietic stem cell injury. Stem Cell Res Ther. 2024;15:222.
Chlon TM, Stepanchick E, Hershberger CE, Daniels NJ, Hueneman KM, Davis AK, et al. Germline DDX41 mutations cause ineffective hematopoiesis and myelodysplasia. Cell Stem Cell. 2021;28:1966.
Yuan JY, Ofengeim D. A guide to cell death pathways. Nat Rev Mol Cell Bio. 2024;25:379–95.
Milyavsky M, Gan OI, Trottier M, Komosa M, Tabach O, Notta F, et al. A distinctive DNA damage response in human hematopoietic stem cells reveals an apoptosis-independent role for p53 in self-renewal. Cell Stem Cell. 2010;7:186–97.
Patterson AM, Liu LQ, Sampson CH, Plett PA, Li HG, Singh P, et al. A single radioprotective dose of prostaglandin E blocks irradiation-induced apoptotic signaling and early cycling of hematopoietic stem cells. Stem Cell Rep. 2020;15:358–73.
Shao LJ, Luo Y, Zhou DH. Hematopoietic stem cell injury induced by ionizing radiation. Antioxid Redox Sign. 2014;20:1447–62.
Wang Y, Liu LB, Pazhanisamy SK, Li HL, Meng A, Zhou DH. Total body irradiation causes residual bone marrow injury by induction of persistent oxidative stress in murine hematopoietic stem cells. Free Radic Bio Med. 2010;48:348–56.
Lu L, Wang YY, Zhang JL, Li DG, Meng AM p38 MAPK inhibitor insufficiently attenuates HSC senescence administered long-term after 6 Gy total body irradiation in mice. Int J Mol Sci 2016;17:905.
Gilbert ES. Ionising radiation and cancer risks: What have we learned from epidemiology?. Int J Radiat Biol. 2009;85:467–82.
Folley JH, Borges W, Yamawaki T. Incidence of leukemia in survivors of the atomic bomb in Hiroshima and Nagasaki, Japan. Am J Med. 1952;13:311–21.
Preston DL, Kusumi S, Tomonaga M, Izumi S, Ron E, Kuramoto A, et al. Cancer incidence in atomic-bomb survivors .3. Leukemia, Lymphoma and Multiple-Myeloma, 1950-1987. Radiat Res. 1994;139:129.
Preston DL, Pierce DA, Shimizu Y, Cullings HM, Fujita S, Funamoto S, et al. Effect of recent changes in atomic bomb survivor dosimetry on cancer mortality risk estimates. Radiat Res. 2004;162:377–89.
NCR. Health Risks from Exposure to Low Levels of Ionizing Radiation: BEIR VII, Phase I, Letter Report (1998). National Academies Press (US): Washington (DC), 1998.
Yoshida K, French B, Yoshida N, Hida A, Ohishi W, Kusunoki Y. Radiation exposure and longitudinal changes in peripheral monocytes over 50 years: the Adult Health Study of atomic-bomb survivors. Brit J Haematol. 2019;185:107–15.
Preston DL, Shimizu Y, Pierce DA, Suyama A, Mabuchi K. Studies of mortality of atomic bomb survivors. Report 13: Solid cancer and noncancer disease mortality: 1950-1997. Radiat Res. 2003;160:381–407.
Bolus NE. Basic review of radiation biology and terminology. J Nucl Med Technol. 2017;45:259–64.
Schroder C, Mose L, Mathier E, Zwahlen DR, Aebersold DM, Forster R, et al. Five fractions versus seven fractions SBRT for intermediate- and high-risk prostate cancer: a propensity score matched pair analysis. Cancers (Basel) 2023;15:5815.
Juarez JE, Kishan AU. Acute toxicities after extremely hypofractionated radiotherapy for prostate cancer: lessons from HYPO-RT-PC and PACE-B. Transl Cancer Res. 2020;9:4469–72.
Beckendorf V, Guerif S, Le Prisé E, Cosset JM, Bougnoux A, Chauvet B, et al. 70 Gy Versus 80 Gy in Localized Prostate Cancer: 5-Year Results of Getug 06 Randomized Trial. Int J Radiat Oncol. 2011;80:1056–63.
Breitenstein BD. The probability that a specific cancer and a specified radiation exposure are causally related. Health Phys. 1988;55:397–8.
Measurements. NCoRPa. NCRP Report No. 134 - Operational Radiation Safety Training 2000. Report No.: 134.
Cucinotta FA, Schimmerling W, Wilson JW, Peterson LE, Badhwar GD, Saganti PB, et al. Space radiation cancer risks and uncertainties for Mars missions. Radiat Res. 2001;156:682–8.
International Commission on Radiological Protection. 1990 Recommendations of the International Commission on Radiological Protection. ICRP Publication 60: Pergamon Press, Oxford., 1991.
Court-Brown WM, Doll R. Leukaemia and aplastic anaemia in patients irradiated for ankylosing spondylitis (Reprinted). J Radio Prot. 2007;27:B15–B154.
Boice JD, Blettner M, Kleinerman RA, Stovall M, Moloney WC, Engholm G, et al. Radiation-dose and leukemia risk in patients treated for cancer of the cervix. Jnci-J Natl Cancer I. 1987;79:1295–311.
Weiss HA, Darby SC, Fearn T, Doll R. Leukemia mortality after X-ray treatment for ankylosing-spondylitis. Radiat Res. 1995;142:1–11.
Little MP, Weiss HA, Boice JD, Darby SC, Day NE, Muirhead CR. Risks of leukemia in Japanese atomic bomb survivors, in women treated for cervical cancer, and in patients treated for ankylosing spondylitis. Radiat Res. 1999;152:280–92.
Giles D, Hewitt D, Stewart A, Webb J. Malignant disease in childhood and diagnostic irradiation in utero. Lancet. 1956;271:447.
Stewart A, Webb J, Hewitt D. A survey of childhood malignancies. Br Med J. 1958;1:1495–508.
Wakeford R, Little MP. Risk coefficients for childhood cancer after intrauterine irradiation: a review. Int J Radiat Biol. 2003;79:293–309.
Hawkins MM, Wilson LMK, Stovall MA, Marsden HB, Potok MHN, Kingston JE, et al. Epipodophyllotoxins, alkylating-agents, and radiation and risk of secondary leukemia after childhood-cancer. Brit Med J. 1992;304:951–8.
Curtis RE, Boice JD, Stovall M, Bernstein L, Greenberg RS, Flannery JT, et al. Risk of leukemia after chemotherapy and radiation treatment for breast-cancer. New Engl J Med. 1992;326:1745–51.
Travis LB, Andersson M, Gospodarowicz M, van Leeuwen FE, Bergfeldt K, Lynch CF, et al. Treatment-associated leukemia following testicular cancer. Jnci-J Natl Cancer I. 2000;92:1165–71.
Inskip PD, Monson RR, Wagoner JK, Stovall M, Davis FG, Kleinerman RA, et al. Leukemia following radiotherapy for uterine bleeding. Radiat Res. 1990;122:107–19.
Inskip PD, Kleinerman RA, Stovall M, Cookfair DL, Hadjimichael O, Moloney WC, et al. Leukemia, lymphoma, and multiple-myeloma after pelvic radiotherapy for benign disease. Radiat Res. 1993;135:108–24.
National Research Council (U.S.). Committee to Assess Health Risks from Exposure to Low Level of Ionizing Radiation. Health risks from exposure to low levels of ionizing radiation : BEIR VII Phase 2. National Academies Press: Washington, D.C., 2006, xvi, 406 p.pp.
Cardis E, Vrijheid M, Blettner M, Gilbert E, Hakama M, Hill C, et al. Risk of cancer after low doses of ionising radiation - retrospective cohort study in 15 countries. Bmj-Brit Med J. 2005;331:77–80b.
Cardis E, Vrijheid M, Blettner M, Gilbert E, Hakama M, Hill C, et al. The 15-country collaborative study of cancer risk among radiation workers in the nuclear industry:: Estimates of radiation-related cancer risks. Radiat Res. 2007;167:396–416.
Muirhead CR, O’Hagan JA, Haylock RGE, Phillipson MA, Willcock T, Berridge GLC, et al. Mortality and cancer incidence following occupational radiation exposure: third analysis of the National Registry for Radiation Workers. Brit J Cancer. 2009;100:206–12.
Romanenko AY, Finch SC, Hatch M, Lubin JH, Bebeshko VG, Bazyka DA, et al. The Ukrainian-American study of leukemia and related disorders among chornobyl cleanup workers from Ukraine: III. Radiation risks. Radiat Res. 2008;170:711–20.
Kesminiene A, Evrard AS, Ivanov VK, Malakhova IV, Kurtinaitis J, Stengrevics A, et al. Risk of hematological malignancies among chernobyl liquidators. Radiation Res. 2008;170:721–35.
Chumak VV, Romanenko AY, Voilleque PG, Bakhanova EV, Gudzenko N, Hatch M, et al. The Ukrainian-American study of leukemia and related disorders among chornobyl cleanup workers from Ukraine: II. Estimation of bone marrow doses. Radiation Res. 2008;170:698–710.
Liu N, Peng Y, Zhong XG, Ma Z, He SP, Li Y, et al. Effects of exposure to low-dose ionizing radiation on changing platelets: a prospective cohort study. Environ Health Prev. 2021;26:14.
Baker KS, Leisenring WM, Goodman PJ, Ermoian RP, Flowers ME, Schoch G, et al. Total body irradiation dose and risk of subsequent neoplasms following allogeneic hematopoietic cell transplantation. Blood. 2019;133:2790–9.
United Nations Scientific Committee on the Effects of Atomic Radiation (UNSCEAR). Sources and Effects of Ionizing Radiation; 2008.
Cucinotta FA, Kim MHY, Ren L. Evaluating shielding effectiveness for reducing space radiation cancer risks. Radiat Meas. 2006;41:1173–85.
National Research Council (U.S.). Committee for Evaluation of Space Radiation Cancer Risk Model., National Research Council (U.S.). Space Studies Board. Technical evaluation of the NASA model for cancer risk to astronauts due to space radiation. National Academies Press: Washington, D.C., 2012, x, 75 p.pp.
National Council on Radiation Protection and Measurements. Report No. 132 – Radiation Protection Guidance for Activities in Low-Earth Orbit 2000. Report No.: 132.
National Aeronautics and Space Administration. NASA Space Flight Human System Standard Volume 1: Crew Health; 2015.
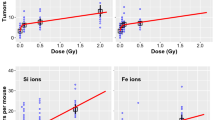
Bielefeldt-Ohmann H, Genik PC, Fallgren CM, Ullrich RL, Weil MM. Animal studies of charged particle-induced carcinogenesis. Health Phys. 2012;103:568–76.
Weil MM, Bedford JS, Bielefeldt-Ohmann H, Ray FA, Genik PC, Ehrhart EJ, et al. Incidence of acute myeloid leukemia and hepatocellular carcinoma in mice irradiated with 1 GeV/nucleon Fe Ions. Radiat Res. 2009;172:213–9.
Patel R, Zhang L, Desai A, Hoenerhoff MJ, Kennedy LH, Radivoyevitch T, et al. Mlh1 deficiency increases the risk of hematopoietic malignancy after simulated space radiation exposure. Leukemia. 2019;33:1135–47.
Dovat S, Song CH, Payne KJ, Li ZJ. Ikaros, CK2 kinase, and the road to leukemia. Mol Cell Biochem. 2011;356:201–7.
Payne KJ, Dovat S. Ikaros and tumor suppression in acute lymphoblastic leukemia. Crit Rev Oncog. 2011;16:3–12.
Gutierrez A, Kentsis A, Sanda T, Holmfeldt L, Chen SC, Zhang JH, et al. The tumor suppressor is mutated across the major molecular subtypes of T-cell acute lymphoblastic leukemia. Blood. 2011;118:4169–73.
Li WX, Wang XY, Dong YP, Huo QD, Yue TP, Wu X, et al. Nicotinamide riboside intervention alleviates hematopoietic system injury of ionizing radiation-induced premature aging mice. Aging Cell 2023;22:13976.
Liao WN, Liu CN, Yang K, Chen J, Wu YD, Zhang S, et al. Aged hematopoietic stem cells entrap regulatory T cells to create a prosurvival microenvironment. Cellular Mol Immunol. 2023;20:1216–31.
Riether C, Schurch CM, Ochsenbein AF. Regulation of hematopoietic and leukemic stem cells by the immune system. Cell Death Differ. 2015;22:187–98.
Rodman C, Almeida-Porada G, George SK, Moon J, Soker S, Pardee T, et al. In vitro and in vivo assessment of direct effects of simulated solar and galactic cosmic radiation on human hematopoietic stem/progenitor cells. Leukemia. 2017;31:1398–407.
Kuhlman BM, Diaz JH, Simon T, Reeves KD, Walker SJ, Atala A, et al. Simulated microgravity impairs human NK cell cytotoxic activity against space radiation-relevant leukemic cells. Npj Microgravity 2024;10:85.
Wei K, Clark AB, Wong E, Kane MF, Mazur DJ, Parris T, et al. Inactivation of Exonuclease 1 in mice results in DNA mismatch repair defects, increased cancer susceptibility, and male and female sterility. Genes Dev. 2003;17:603–14.
Iyer RR, Pluciennik A, Burdett V, Modrich PL. DNA mismatch repair: functions and mechanisms. Chem Rev. 2006;106:302–23.
Piao JS, Nakatsu Y, Ohno M, Taguchi K, Tsuzuki T. Mismatch repair deficient mice show susceptibility to oxidative stress-induced intestinal carcinogenesis. Int J Biol Sci. 2014;10:73–9.
Ma YX, Chen Y, Petersen I. Expression and promoter DNA methylation of MLH1 in colorectal cancer and lung cancer. Pathol Res Pr. 2017;213:333–8.
Gutiérrez VF, Marcos CA, Llorente JL, Guervos MA, Iglesias FD, Tamargo LA, et al. Genetic profile of second primary tumors and recurrences in head and neck squamous cell carcinomas. Head Neck-J Sci Spec. 2012;34:830–9.
Stark AM, Doukas A, Hugo HH, Hedderich J, Hattermann K, Maximilian Mehdorn H, et al. Expression of DNA mismatch repair proteins MLH1, MSH2, and MSH6 in recurrent glioblastoma. Neurol Res. 2015;37:95–105.
Cosgrove CM, Cohn DE, Hampel H, Frankel WL, Jones D, McElroy JP, et al. Epigenetic silencing of MLH1 in endometrial cancers is associated with larger tumor volume, increased rate of lymph node positivity and reduced recurrence-free survival. Gynecol Oncol. 2017;146:588–95.
Kenyon J, Fu P, Lingas K, Thomas E, Saurastri A, Santos Guasch G, et al. Humans accumulate microsatellite instability with acquired loss of MLH1 protein in hematopoietic stem and progenitor cells as a function of age. Blood. 2012;120:3229–36.
Kenyon J, Nickel-Meester G, Qing Y, Santos-Guasch G, Drake E, Fu P, et al. Epigenetic Loss of MLH1 Expression in Normal Human Hematopoietic Stem Cell Clones is Defined by the Promoter CpG Methylation Pattern Observed by High-Throughput Methylation Specific Sequencing. Int J Stem Cell Res Ther. 2016;3:031.
Asada S, Kitamura T. Clonal hematopoiesis and associated diseases: A review of recent findings. Cancer Sci. 2021;112:3962–71.
Brojakowska A, Kour A, Thel MC, Park E, Bisserier M, Garikipati VNS, et al. Retrospective analysis of somatic mutations and clonal hematopoiesis in astronauts (Aug, 2022). Commun Biol. 2022;5:828. https://doi.org/10.1038/s42003-022-03777-z
Liu YQ, Tavana O, Gu W. p53 modifications: exquisite decorations of the powerful guardian. J Mol Cell Biol. 2019;11:564–77.
Sano S, Wang Y, Ogawa H, Horitani K, Sano M, Polizio AH, et al. TP53-mediated therapy-related clonal hematopoiesis contributes to doxorubicin-induced cardiomyopathy by augmenting a neutrophil-mediated cytotoxic response. Jci Insight 2021;6:146076.
Yang LB, Rau R, Goodell MA. DNMT3A in haematological malignancies. Nat Rev Cancer. 2015;15:152–65.
Cucinotta FA, Chappell LJ, Kim MH, Wang M. Radiation carcinogenesis risk assessments for never-smokers. Health Phys. 2012;103:643–51.
Cucinotta FA. Space radiation risks for astronauts on multiple international space station missions. Plos One 2014; 9:96099.
Reynolds R, Little MP, Day S, Charvat J, Blattnig S, Huff J, et al. Cancer incidence and mortality in the USA Astronaut Corps, 1959-2017. Occupational Environ Med. 2021;78:869–75.
Hamm PB, Billica RD, Johnson GS, Wear ML, Pool SL. Risk of cancer mortality among the Longitudinal Study of Astronaut Health (LSAH) participants. Aviat Space Environ Med. 1998;69:142–4.
Hamm PB, Nicogossian AE, Pool SL, Wear ML, Billica RD. Design and current status of the longitudinal study of astronaut health. Aviat Space Environ Med. 2000;71:564–70.
Reynolds RJ, Day SM. Mortality among U.S. astronauts: 1980-2009. Aviat Space Environ Med. 2010;81:1024–7.
Krittanawong C, Singh NK, Scheuring RA, Urquieta E, Bershad EM, Macaulay TR, et al. Human health during space travel: state-of-the-art review. Cells-Basel 2023;12:40.
In: Longnecker DE, Manning FJ, Worth MH, Jr. (eds). Review of NASA’s Longitudinal Study of Astronaut Health: Washington (DC), 2004.
Delp MD, Charvat JM, Limoli CL, Globus RK, Ghosh P. Apollo lunar astronauts show higher cardiovascular disease mortality: possible deep space radiation effects on the vascular endothelium. Sci Rep-Uk 2016;6:29901.
Schaefer HJ, Benton EV, Henke RP, Sullivan JJ. Nuclear track recordings of the astronauts’ radiation exposure on the first lunar landing mission Apollo XI. Radiat Res. 1972;49:245–71.
Fleischer RL, Hart HR Jr, Comstock GM, Carter M, Renshaw A, Hardy A. Apollo 14 and apollo 16 heavy-particle dosimetry experiments. Science. 1973;181:436–8.
Low EK, Brudvik E, Kuhlman B, Wilson PF, Almeida-Porada G, Porada CD. Microgravity impairs DNA damage repair in human hematopoietic stem/progenitor cells and inhibits their differentiation into dendritic cells. Stem Cells Dev. 2018;27:1257–67.
Paez YM, Mudie LI, Subramanian PS. Spaceflight associated neuro-ocular syndrome (SANS): a systematic review and future directions. Eye Brain. 2020;12:105–17.
Welsh JS, Karam PA, Gale RP. Radiation exposure and space exploration. Leukemia 2024;38:1870–71.
Smirnova OA, Cucinotta FA. Dynamical modeling approach to risk assessment for radiogenic leukemia among astronauts engaged in interplanetary space missions. Life Sci Space Res. 2018;16:76–83.
Borak TB, Heilbronn LH, Townsend LW, McBeth RA, de Wet W. Quality factors for space radiation: A new approach. Life Sci Space Res (Amst). 2014;1:96–102.
Acknowledgements
No funding was granted for the study.
Author information
Authors and Affiliations
Contributions
The authors Fay Ghani and Abba C. Zubair contributed equally and have both participated in conceptualizing the research or content of the manuscript, in writing or critically editing the manuscript, and/or in analysis of data presented in the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ghani, F., Zubair, A.C. Possible impacts of cosmic radiation on leukemia development during human deep space exploration. Leukemia 39, 1578–1588 (2025). https://doi.org/10.1038/s41375-025-02624-4
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41375-025-02624-4