Abstract
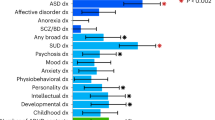
Childhood attention deficit hyperactivity disorder (ADHD) shows a highly variable course with age: some individuals show improving, others stable or worsening symptoms. The ability to predict symptom course could help individualize treatment and guide interventions. By studying a cohort of 362 youth, we ask if polygenic risk for ADHD, combined with baseline neural and cognitive features could aid in the prediction of the course of symptoms over an average period of 4.8 years. Compared to a never-affected comparison group, we find that participants with worsening symptoms carried the highest polygenic risk for ADHD, followed by those with stable symptoms, then those whose symptoms improved. Participants with worsening symptoms also showed atypical baseline cognition. Atypical microstructure of the cingulum bundle and anterior thalamic radiation was associated with improving symptoms while reduction of thalamic volume was found in those with stable symptoms. Machine-learning algorithms, trained and tested on independent groups, performed well in classifying those never affected against groups with worsening, stable, and improving symptoms (area under the curve >0.79). We conclude that some measures of polygenic risk, cognition, and neuroimaging show significant associations with the future course of ADHD symptoms and may have modest predictive power. These features warrant further exploration as prognostic tools.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Sibley MH, Mitchell JT, Becker SP. Method of adult diagnosis influences estimated persistence of childhood ADHD: a systematic review of longitudinal studies. Lancet Psychiatry. 2016;3:1157–65.
Faraone SV, Biederman J, Mick E. The age-dependent decline of attention deficit hyperactivity disorder: a meta-analysis of follow-up studies. Psychol Med. 2006;36:159–65.
Caye A, Spadini AV, Karam RG, Grevet EH, Rovaris DL, Bau CH, et al. Predictors of persistence of ADHD into adulthood: a systematic review of the literature and meta-analysis. Eur Child Adolesc Psychiatry. 2016;25:1151–9.
Demontis D, Walters RK, Martin J, Mattheisen M, Als TD, Agerbo E, et al. Discovery of the first genome-wide significant risk loci for ADHD. bioRxiv. 2017. https://doi.org/10.1101/145581.
Wray NR, Goddard ME, Visscher PM. Prediction of individual genetic risk to disease from genome-wide. Genome Res. 2007;17:1520–8.
Pingault JB, Viding E, Galera C, Greven C, Zheng YRP, et al. Genetic and environmental influences on the developmental course of attention-deficit/hyperactivity disorder symptoms from childhood to adolescence. JAMA Psychiatry. 2015. https://doi.org/10.1001/jamapsychiatry.2015.0469T.
Riglin L, Collishaw S, Thapar AK, Dalsgaard S, Langley K, Smith GD, et al. Association of genetic risk variants with attention-deficit/hyperactivity disorder trajectories in the general population. JAMA Psychiatry. 2016;73:1285–92.
Mackie S, Shaw P, Lenroot R, Pierson R, Greenstein DK, Nugent TF 3rd, et al. Cerebellar development and clinical outcome in attention deficit hyperactivity disorder. Am J Psychiatry. 2007;164:647–55.
Shaw P, Lerch J, Greenstein D, Sharp W, Clasen L, Evans A, et al. Longitudinal mapping of cortical thickness and clinical outcome in children and adolescents with attention deficit/hyperactivity disorder. Arch Gen Psychiatry. 2006;63:540–9.
Clarke AR, Barry RJ, Dupuy FE, McCarthy R, Selikowitz M, Heaven PC. Childhood EEG as a predictor of adult attention-deficit/hyperactivity disorder. Clin Neurophysiol. 2011;122:73–80.
Whitfield-Gabrieli S, Wendelken C, Nieto-Castañón A, Bailey SK, Anteraper SA, Lee YJ, et al. Association of intrinsic brain architecture with changes in attentional and mood symptoms during development. JAMA Psychiatry. 2020;77:378–86. https://doi.org/10.1001/jamapsychiatry.2019.4208.
Martinussen R, Hayden J, Hogg-Johnson S, Tannock R. A meta-analysis of working memory impairments in children with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2005;44:377–84.
Willcutt EG, Doyle AE, Nigg JT, Faraone SV, Pennington BF. Validity of the executive function theory of attention-deficit/hyperactivity disorder: a meta-analytic review. Biol Psychiatry. 2005;57:1336–46.
Cook NE, Braaten EB, Surman CB. Clinical and functional correlates of processing speed in pediatric attention-deficit/hyperactivity disorder: a systematic review and meta-analysis. Child Neuropsychol. 2018;24:598–616.
Reich W, Welner Z, Herkanic B. Diagnostic interview for children and adolescents (DICA-IV). North Tonawanda, NY: Multi-Health Systems; 1997.
Euesden J, Lewis CM, O’Reilly PF. PRSice: polygenic risk score software. Bioinformatics. 2014;31:1466–8.
Demontis D, Walters RK, Martin J, Mattheisen M, Als TD, Agerbo E, et al. Discovery of the first genome-wide significant risk loci for attention deficit/hyperactivity disorder. Nat Genet. 2019;51:63–75. https://doi.org/10.1038/s41588-018-0269-7.
Fischl B. FreeSurfer. Neuroimage. 2012;62:774–81.
Shaw P, Ishii-Takahashi A, Park MT, Devenyi GA, Zibman C, Kasparek S, et al. A multicohort, longitudinal study of cerebellar development in attention deficit hyperactivity disorder. J Child Psychol Psychiatry. 2018;59:1114–23. https://doi.org/10.1111/jcpp.12920.
Hoogman M, Muetzel R, Guimaraes JP, Shumskaya E, Mennes M, Zwiers MP, et al. Brain imaging of the cortex in ADHD: a coordinated analysis of large-scale clinical and population-based samples. Am J Psychiatry. 2019;176:531–42.
Hoogman M, Buitelaar JK, Faraone SV, Shaw P, Franke B. Subcortical brain volume differences in participants with attention deficit hyperactivity disorder in children and adults—authors’ reply. Lancet Psychiatry. 2017;4:440–1.
Rubia K. Cognitive neuroscience of attention deficit hyperactivity disorder (ADHD) and Its clinical translation. Front Hum Neurosci. 2018;12:100.
Hua K, Zhang J, Wakana S, Jiang H, Li X, Reich DS, et al. Tract probability maps in stereotaxic spaces: analyses of white matter anatomy and tract-specific quantification. Neuroimage. 2008;39:336–47.
Wechsler, D. Wechsler abbreviated scale of intelligence, Second Edition (WASI-II). San Antonio, TX. NCS Pearson; 2011.
Wechsler D. Wechsler preschool and primary scale of intelligence, Fourth edition. San Antonio, TX: Psychological Corporation; 2012.
Wechsler, D. Wechsler Intelligence Scale for Children—Fourth Edition. San Antonio, TX. Psychological Corporation; 2003.
Beery KE. Beery VMI: the Beery-Buktenica developmental test of visual-motor integration. Minneapolis, MN: Pearson; 2004.
Woodcock RW, McGrew KS, Mather N. Woodcock-Johnson III: tests of achievement. Itasca, IL. Riverside Publishing Company; 2001.
Hollingshead A. Four factor index of social status. New Haven: Yale University Department of Sociology; 1975.
Rosnow RL, Rosenthal R. Computing contrasts, effect sizes, and counternulls on other people’s published data: General procedures for research consumers. Psychol Methods. 1996;1:331.
Hothorn T, Hornik K, Zeileis A. Unbiased recursive partitioning: a conditional inference framework. J Comput Graph Stat. 2006;15:651–74.
Vuijk PJ, Martin J, Braaten EB, Genovese G, Capawana MR, O’Keefe SM, et al. Translating Discoveries in Attention-Deficit/Hyperactivity Disorder Genomics to an Outpatient Child and Adolescent Psychiatric Cohort. J Am Acad Child Adolesc Psychiatry. 2020;59:964–77. https://doi.org/10.1016/j.jaac.2019.08.004.
Nigg JT, Gustafsson HC, Karalunas SL, Ryabinin P, McWeeney SK, Faraone SV, et al. Working memory and vigilance as multivariate endophenotypes related to common genetic risk for attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2018;57:175–82.
Sudre G, Frederick J, Sharp W, Ishii-Takahashi A, Mangalmurti A, Choudhury S, et al. Mapping associations between polygenic risks for childhood neuropsychiatric disorders, symptoms of attention deficit hyperactivity disorder, cognition, and the brain. Mol Psychiatry. 2020;25:2482–92. https://doi.org/10.1038/s41380-019-0350-3.
Martin J, Hamshere ML, Stergiakouli E, O’Donovan MC, Thapar A. Genetic risk for attention-deficit/hyperactivity disorder contributes to neurodevelopmental traits in the general population. Biol Psychiatry. 2014;76:664–71.
Carr LA, Nigg JT, Henderson JM. Attentional versus motor inhibition in adults with attention-deficit/hyperactivity disorder. Neuropsychology. 2006;20:430–41. https://doi.org/10.1037/0894-4105.20.4.430.
van Lieshout M, Luman M, Twisk JWR, Faraone SV, Heslenfeld DJ, Hartman CA, et al. Neurocognitive predictors of ADHD outcome: a 6-year follow-up study. J Abnorm Child Psychol. 2017;45:261–72.
Sjöwall D, Bohlin G, Rydell A-M, Thorell LB. Neuropsychological deficits in preschool as predictors of ADHD symptoms and academic achievement in late adolescence. Child Neuropsychol. 2017;23:111–28.
Karalunas SL, Gustafsson HC, Dieckmann NF, Tipsord J, Mitchell SH, Nigg JT. Heterogeneity in development of aspects of working memory predicts longitudinal attention deficit hyperactivity disorder symptom change. J Abnorm Psychol. 2017;126:774.
Makris N, Buka SL, Biederman J, Papadimitriou GM, Hodge SM, Valera EM, et al. Attention and executive systems abnormalities in adults with childhood ADHD: A DT-MRI study of connections. Cereb Cortex. 2008;18:1210–20.
Chiang H-L, Chen Y-J, Lo Y-C, Tseng W-YI, Gau SS-F. Altered white matter tract property related to impaired focused attention, sustained attention, cognitive impulsivity and vigilance in attention-deficit/hyperactivity disorder. J Psychiatry Neurosci. 2015;40:325.
Lebel C, Gee M, Camicioli R, Wieler M, Martin W, Beaulieu C. Diffusion tensor imaging of white matter tract evolution over the lifespan. Neuroimage. 2012;60:340–52.
Kuriyan AB, Pelham WE Jr, Molina BS, Waschbusch DA, Sibley MH, Gnagy EM. Concordance between parent and physician medication histories for children and adolescents with attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol. 2014;24:269–74.
Owens EB, Cardoos SL, Hinshaw SP. Developmental progression and gender differences among individuals with ADHD. In: Barkley RA, editor. Attention-deficit hyperactivity disorder: a handbook for diagnosis and treatment. New York, NY. The Guilford Press; 2015.
Dalsgaard S, Mortensen PB, Frydenberg M, Thomsen PH. Conduct problems, gender and adult psychiatric outcome of children with attention-deficit hyperactivity disorder. Br J Psychiatry. 2002;181:416–21.
Wolfers T, Buitelaar JK, Beckmann CF, Franke B, Marquand AF. From estimating activation locality to predicting disorder: a review of pattern recognition for neuroimaging-based psychiatric diagnostics. Neurosci Biobehav Rev. 2015;57:328–49.
Kim JW, Sharma V, Ryan ND. Predicting Methylphenidate Response in ADHD Using Machine Learning Approaches. Int J Neuropsychopharmacol. 2015;18:pyv052.
Luo Y, Alvarez TL, Halperin JM, Li X. Multimodal neuroimaging-based prediction of adult outcomes in childhood-onset ADHD using ensemble learning techniques. NeuroImage: Clin. 2020;26:102238. https://doi.org/10.1016/j.nicl.2020.102238.
Caye A, Agnew-Blais J, Arseneault L, Gonçalves H, Kieling C, Langley K, et al. A risk calculator to predict adult attention-deficit/hyperactivity disorder: generation and external validation in three birth cohorts and one clinical sample. Epidemiol Psychiatr Sci. 2019;29:e37. https://doi.org/10.1017/S2045796019000283.
Acknowledgements
Research is supported by the intramural programs of the National Human Genome Research Institute and National Institute of Mental Health. This work utilized the computational resources of the NIH HPC Biowulf cluster (http://hpc.nih.gov).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Sudre, G., Sharp, W., Kundzicz, P. et al. Predicting the course of ADHD symptoms through the integration of childhood genomic, neural, and cognitive features. Mol Psychiatry 26, 4046–4054 (2021). https://doi.org/10.1038/s41380-020-00941-x
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41380-020-00941-x
This article is cited by
-
Evidence from “big data” for the default-mode hypothesis of ADHD: a mega-analysis of multiple large samples
Neuropsychopharmacology (2023)
-
Machine learning in attention-deficit/hyperactivity disorder: new approaches toward understanding the neural mechanisms
Translational Psychiatry (2023)
-
Is genetic risk of ADHD mediated via dopaminergic mechanism? A study of functional connectivity in ADHD and pharmacologically challenged healthy volunteers with a genetic risk profile
Translational Psychiatry (2022)