Abstract
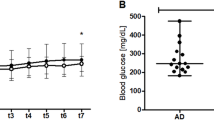
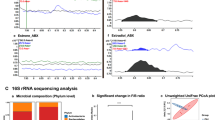
While our understanding of the molecular biology of Alzheimer’s disease (AD) has grown, the etiology of the disease, especially the involvement of peripheral infection, remains a challenge. In this study, we hypothesize that peripheral infection represents a risk factor for AD pathology. To test our hypothesis, APP/PS1 mice underwent cecal ligation and puncture (CLP) surgery to develop a polymicrobial infection or non-CLP surgery. Mice were euthanized at 3, 30, and 120 days after surgery to evaluate the inflammatory mediators, glial cell markers, amyloid burden, gut microbiome, gut morphology, and short-chain fatty acids (SCFAs) levels. The novel object recognition (NOR) task was performed 30 and 120 days after the surgery, and sepsis accelerated the cognitive decline in APP/PS1 mice at both time points. At 120 days, the insoluble Aβ increased in the sepsis group, and sepsis modulated the cytokines/chemokines, decreasing the cytokines associated with brain homeostasis IL-10 and IL-13 and increasing the eotaxin known to influence cognitive function. At 120 days, we found an increased density of IBA-1-positive microglia in the vicinity of Aβ dense-core plaques, compared with the control group confirming the predictable clustering of reactive glia around dense-core plaques within 15 μm near Aβ deposits in the brain. In the gut, sepsis negatively modulated the α- and β-diversity indices evaluated by 16S rRNA sequencing, decreased the levels of SCFAs, and significantly affected ileum and colon morphology in CLP mice. Our data suggest that sepsis-induced peripheral infection accelerates cognitive decline and AD pathology in the AD mouse model.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Data availability
The datasets during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Change history
22 January 2024
A Correction to this paper has been published: https://doi.org/10.1038/s41380-024-02416-9
References
GBD 2019 Dementia Forecasting Collaborators. Estimation of the global prevalence of dementia in 2019 and forecasted prevalence in 2050: an analysis for the Global Burden of Disease Study 2019. Lancet Public Health. 2022;7:e105–e125.
Brookmeyer R, Johnson E, Ziegler-Graham K, Arrighi HM. Forecasting the global burden of Alzheimer’s disease. Alzheimer’s Dement. 2007;3:186–91.
Bateman RJ, Aisen PS, De Strooper B, Fox NC, Lemere CA, Ringman JM, et al. Autosomal-dominant Alzheimer’s disease: a review and proposal for the prevention of Alzheimer’s disease. Alzheimer’s Res Therap. 2011;3:1.
Duncombe J, Kitamura A, Hase Y, Ihara M, Kalaria RN, Horsburgh K. Chronic cerebral hypoperfusion: a key mechanism leading to vascular cognitive impairment and dementia. Closing the translational gap between rodent models and human vascular cognitive impairment and dementia. Clin Sci. 2017;131:2451–68.
Liao J, Chen G, Liu X, Wei ZZ, Yu SP, Chen Q, et al. C/EBPβ/AEP signaling couples atherosclerosis to the pathogenesis of Alzheimer’s disease. Mol Psychiat. 2022;27:3034–46.
Licastro F. Special Issue Editorial: "Infections, Inflammation and Neurodegeneration in Alzheimer Disease" Infections, Neuronal Senescence, and Dementia. Int J Mol Sci. 2022;23:5865.
Jiang M, Zhang X, Yan X, Mizutani S, Kashiwazaki H, Ni J, et al. GSK3β is involved in promoting Alzheimer’s disease pathologies following chronic systemic exposure to Porphyromonas gingivalis lipopolysaccharide in amyloid precursor protein(NL-F/NL-F) knock-in mice. Brain behav Immun. 2021;98:1–12.
Ackermans NL, Varghese M, Williams TM, Grimaldi N, Selmanovic E, Alipour A, et al. Evidence of traumatic brain injury in headbutting bovids. Acta Neuropathol. 2022;144:5–26.
Iwashyna TJ, Ely EW, Smith DM, Langa KM. Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA. 2010;304:1787–94.
Readhead B, Haure-Mirande JV, Funk CC, Richards MA, Shannon P, Haroutunian V, et al. Multiscale Analysis of Independent Alzheimer’s Cohorts Finds Disruption of Molecular, Genetic, and Clinical Networks by Human Herpesvirus. Neuron. 2018;99:64–82.e67.
Tzeng NS, Chung CH, Lin FH, Chiang CP, Yeh CB, Huang SY, et al. Anti-herpetic Medications and Reduced Risk of Dementia in Patients with Herpes Simplex Virus Infections-a Nationwide, Population-Based Cohort Study in Taiwan. Neurotherapeutics. 2018;15:417–29.
Moreno-Gonzalez I, Morales R, Baglietto-Vargas D, Sanchez-Varo R. Editorial: Risk Factors for Alzheimer’s Disease. Front Agin Neurosci. 2020;12:124.
Doifode T, Giridharan VV, Generoso JS, Bhatti G, Collodel A, Schulz PE, et al. The impact of the microbiota-gut-brain axis on Alzheimer’s disease pathophysiology. Pharmacol Res. 2021;164:105314.
Barichello T, Generoso JS, Collodel A, Petronilho F, Dal-Pizzol F. The blood-brain barrier dysfunction in sepsis. Tissue Barriers. 2021;9:1840912.
Licinio J, Wong ML. Molecular Psychiatry special issue: advances in Alzheimer’s disease. Mol Psychiat. 2021;26:5467–70.
Moir RD, Lathe R, Tanzi RE. The antimicrobial protection hypothesis of Alzheimer’s disease. Alzheimer’s & Dement. 2018;14:1602–14.
Hur JY, Frost GR, Wu X, Crump C, Pan SJ, Wong E, et al. The innate immunity protein IFITM3 modulates γ-secretase in Alzheimer’s disease. Nature. 2020;586:735–40.
Holmes C, Cotterell D. Role of infection in the pathogenesis of Alzheimer’s disease: implications for treatment. CNS Drugs. 2009;23:993–1002.
Miklossy J. Chronic inflammation and amyloidogenesis in Alzheimer’s disease - role of Spirochetes. J Alzheimer’s Dis. 2008;13:381–91.
Grant I, Franklin DR Jr, Deutsch R, Woods SP, Vaida F, Ellis RJ, et al. Asymptomatic HIV-associated neurocognitive impairment increases risk for symptomatic decline. Neurology. 2014;82:2055–62.
Itzhaki RF, Wozniak MA. Herpes simplex virus type 1 in Alzheimer’s disease: the enemy within. J Alzheimer’s Dis. 2008;13:393–405.
Gasparotto J, Girardi CS, Somensi N, Ribeiro CT, Moreira JCF, Michels M, et al. Receptor for advanced glycation end products mediates sepsis-triggered amyloid-β accumulation, Tau phosphorylation, and cognitive impairment. J Biol Chem. 2018;293:226–44.
Giridharan VV, Generoso JS, Lence L, Candiotto G, Streck E, Petronilho F, et al. A crosstalk between gut and brain in sepsis-induced cognitive decline. J Neuroinflamm. 2022;19:114.
Basak JM, Ferreiro A, Cohen LS, Sheehan PW, Nadarajah CJ, Kanan MF, et al. Bacterial sepsis increases hippocampal fibrillar amyloid plaque load and neuroinflammation in a mouse model of Alzheimer’s disease. Neurobiol Dis. 2021;152:105292.
Giridharan VV, Generoso JS, Collodel A, Dominguini D, Faller CJ, Tardin F, et al. Receptor for Advanced Glycation End Products (RAGE) Mediates Cognitive Impairment Triggered by Pneumococcal Meningitis. Neurotherapeutics. 2021;18:640–53.
Barichello T, Giridharan VV, Comim CM, Morales R. What is the role of microbial infection in Alzheimer’s disease? Revista brasileira de psiquiatria (Sao Paulo, Brazil : 1999) 2021.
Garcia-Alloza M, Robbins EM, Zhang-Nunes SX, Purcell SM, Betensky RA, Raju S, et al. Characterization of amyloid deposition in the APPswe/PS1dE9 mouse model of Alzheimer disease. Neurobiol Dis. 2006;24:516–24.
Heming N, Mazeraud A, Verdonk F, Bozza FA, Chrétien F, Sharshar T. Neuroanatomy of sepsis-associated encephalopathy. Critic Care. 2017;21:65.
Ehler J, Barrett LK, Taylor V, Groves M, Scaravilli F, Wittstock M, et al. Translational evidence for two distinct patterns of neuroaxonal injury in sepsis: a longitudinal, prospective translational study. Critic Care. 2017;21:262.
Rittirsch D, Huber-Lang MS, Flierl MA, Ward PA. Immunodesign of experimental sepsis by cecal ligation and puncture. Nat Protoc. 2009;4:31–36.
Idris N, Neill J, Grayson B, Bang-Andersen B, Witten LM, Brennum LT, et al. Sertindole improves sub-chronic PCP-induced reversal learning and episodic memory deficits in rodents: involvement of 5-HT(6) and 5-HT (2 A) receptor mechanisms. Psychopharmacology. 2010;208:23–36.
Scaini G, Fries GR, Valvassori SS, Zeni CP, Zunta-Soares G, Berk M, et al. Perturbations in the apoptotic pathway and mitochondrial network dynamics in peripheral blood mononuclear cells from bipolar disorder patients. Transl Psychiat. 2017;7:e1111.
Kawarabayashi T, Younkin LH, Saido TC, Shoji M, Ashe KH, Younkin SG. Age-dependent changes in brain, CSF, and plasma amyloid (beta) protein in the Tg2576 transgenic mouse model of Alzheimer’s disease. J Neurosci. 2001;21:372–81.
Bolyen E, Rideout JR, Dillon MR, Bokulich NA, Abnet CC, Al-Ghalith GA, et al. Reproducible, interactive, scalable and extensible microbiome data science using QIIME 2. Nature Biotechnol. 2019;37:852–7.
Zhao G, Nyman M, Jönsson JA. Rapid determination of short-chain fatty acids in colonic contents and faeces of humans and rats by acidified water-extraction and direct-injection gas chromatography. Biomed Chromatogr 2006;20:674–82.
Radde R, Bolmont T, Kaeser SA, Coomaraswamy J, Lindau D, Stoltze L, et al. Abeta42-driven cerebral amyloidosis in transgenic mice reveals early and robust pathology. EMBO Rep. 2006;7:940–6.
Serneels L, Van Biervliet J, Craessaerts K, Dejaegere T, Horré K, Van Houtvin T, et al. gamma-Secretase heterogeneity in the Aph1 subunit: relevance for Alzheimer’s disease. Science. 2009;324:639–42.
Wang J, Dickson DW, Trojanowski JQ, Lee VM. The levels of soluble versus insoluble brain Abeta distinguish Alzheimer’s disease from normal and pathologic aging. Exp Neurol. 1999;158:328–37.
Sofroniew MV, Vinters HV. Astrocytes: biology and pathology. Acta Neuropathol. 2010;119:7–35.
Bird CM, Burgess N. The hippocampus and memory: insights from spatial processing. Nature Rev Neurosci. 2008;9:182–94.
Sun Q, Zhang J, Li A, Yao M, Liu G, Chen S, et al. Acetylcholine deficiency disrupts extratelencephalic projection neurons in the prefrontal cortex in a mouse model of Alzheimer’s disease. Nature Commun. 2022;13:998.
Zhurakovskaya E, Ishchenko I, Gureviciene I, Aliev R, Gröhn O, Tanila H. Impaired hippocampal-cortical coupling but preserved local synchrony during sleep in APP/PS1 mice modeling Alzheimer’s disease. Sci Rep. 2019;9:5380.
Vogt NM, Kerby RL, Dill-McFarland KA, Harding SJ, Merluzzi AP, Johnson SC, et al. Gut microbiome alterations in Alzheimer’s disease. Sci Reports. 2017;7:13537.
Adelman MW, Woodworth MH, Langelier C, Busch LM, Kempker JA, Kraft CS, et al. The gut microbiome’s role in the development, maintenance, and outcomes of sepsis. Critic Care. 2020;24:278.
Liu P, Wu L, Peng G, Han Y, Tang R, Ge J, et al. Altered microbiomes distinguish Alzheimer’s disease from amnestic mild cognitive impairment and health in a Chinese cohort. Brain Behav Immun. 2019;80:633–43.
Wu L, Han Y, Zheng Z, Peng G, Liu P, Yue S, et al. Altered Gut Microbial Metabolites in Amnestic Mild Cognitive Impairment and Alzheimer’s Disease: Signals in Host-Microbe Interplay. Nutrients. 2021;13:228.
Wen C, Xie T, Pan K, Deng Y, Zhao Z, Li N, et al. Acetate attenuates perioperative neurocognitive disorders in aged mice. Aging. 2020;12:3862–79.
Yende S, Austin S, Rhodes A, Finfer S, Opal S, Thompson T, et al. Long-Term Quality of Life Among Survivors of Severe Sepsis: Analyses of Two International Trials. Critic Care Med. 2016;44:1461–7.
Buchman TG, Simpson SQ, Sciarretta KL, Finne KP, Sowers N, Collier M, et al. Sepsis Among Medicare Beneficiaries: 1. The Burdens of Sepsis, 2012-2018. Critic Care Med. 2020;48:276–88.
Gracner T, Agarwal M, Murali KP, Stone PW, Larson EL, Furuya EY, et al. Association of Infection-Related Hospitalization With Cognitive Impairment Among Nursing Home Residents. JAMA Network Open. 2021;4:e217528–e217528.
Hanseeuw BJ, Betensky RA, Jacobs HIL, Schultz AP, Sepulcre J, Becker JA, et al. Association of Amyloid and Tau With Cognition in Preclinical Alzheimer Disease: A Longitudinal Study. JAMA Neurol. 2019;76:915–24.
Kumar DK, Choi SH, Washicosky KJ, Eimer WA, Tucker S, Ghofrani J, et al. Amyloid-β peptide protects against microbial infection in mouse and worm models of Alzheimer’s disease. Sci Transl Med. 2016;8:340ra372.
Licinio J, Wong M-L. Advances in Molecular Psychiatry – March 2023: mitochondrial function, stress, neuroinflammation – bipolar disorder, psychosis, and Alzheimer’s disease. Mol Psychiat. 2023;28:968–71.
Haage V, De Jager PL. Neuroimmune contributions to Alzheimer’s disease: a focus on human data. Mol Psychiat. 2022;27:3164–81.
Giridharan VV, Masud F, Petronilho F, Dal-Pizzol F, Barichello T. Infection-Induced Systemic Inflammation Is a Potential Driver of Alzheimer’s Disease Progression. Front Agin Neurosci. 2019;11:122.
Comim CM, Vilela MC, Constantino LS, Petronilho F, Vuolo F, Lacerda-Queiroz N, et al. Traffic of leukocytes and cytokine up-regulation in the central nervous system in sepsis. Intens Care Med. 2011;37:711–8.
Barichello T, Generoso JS, Silvestre C, Costa CS, Carrodore MM, Cipriano AL, et al. Circulating concentrations, cerebral output of the CINC-1 and blood–brain barrier disruption in Wistar rats after pneumococcal meningitis induction. Eur J Clin Microbiol Infect Dis. 2012;31:2005–9.
Lin Z, Sur S, Liu P, Li Y, Jiang D, Hou X, et al. Blood-Brain Barrier Breakdown in Relationship to Alzheimer and Vascular Disease. Annal Neurol. 2021;90:227–38.
Shin WH, Lee DY, Park KW, Kim SU, Yang MS, Joe EH, et al. Microglia expressing interleukin-13 undergo cell death and contribute to neuronal survival in vivo. Glia. 2004;46:142–52.
Barichello T. The role of innate lymphoid cells (ILCs) in mental health. Discov Mental Health. 2022;2:2.
Miao W, Zhao Y, Huang Y, Chen D, Luo C, Su W, et al. IL-13 Ameliorates Neuroinflammation and Promotes Functional Recovery after Traumatic Brain Injury. J Immunol. 2020;204:1486–98.
Kolosowska N, Keuters MH, Wojciechowski S, Keksa-Goldsteine V, Laine M, Malm T, et al. Peripheral Administration of IL-13 Induces Anti-inflammatory Microglial/Macrophage Responses and Provides Neuroprotection in Ischemic Stroke. Neurotherapeutics. 2019;16:1304–19.
Brombacher TM, Nono JK, De Gouveia KS, Makena N, Darby M, Womersley J, et al. IL-13-Mediated Regulation of Learning and Memory. J Immunol. 2017;198:2681–8.
Villeda SA, Luo J, Mosher KI, Zou B, Britschgi M, Bieri G, et al. The ageing systemic milieu negatively regulates neurogenesis and cognitive function. Nature. 2011;477:90–94.
Choi C, Jeong JH, Jang JS, Choi K, Lee J, Kwon J, et al. Multiplex analysis of cytokines in the serum and cerebrospinal fluid of patients with Alzheimer’s disease by color-coded bead technology. J Clin Neurol. 2008;4:84–88.
Kong Y, Li HD, Wang D, Gao X, Yang C, Li M, et al. Group 2 innate lymphoid cells suppress the pathology of neuromyelitis optica spectrum disorder. FASEB J. 2021;35:e21856.
Nazarinia D, Behzadifard M, Gholampour J, Karimi R, Gholampour M. Eotaxin-1 (CCL11) in neuroinflammatory disorders and possible role in COVID-19 neurologic complications. Acta Neurol Belg. 2022;122:865–9.
Zhang L, Wang Y, Xiayu X, Shi C, Chen W, Song N, et al. Altered Gut Microbiota in a Mouse Model of Alzheimer’s Disease. J Alzheimer’s Dis. 2017;60:1241–57.
Marizzoni M, Cattaneo A, Mirabelli P, Festari C, Lopizzo N, Nicolosi V, et al. Short-Chain Fatty Acids and Lipopolysaccharide as Mediators Between Gut Dysbiosis and Amyloid Pathology in Alzheimer’s Disease. J Alzheimer’s Dis. 2020;78:683–97.
Shin NR, Whon TW, Bae JW. Proteobacteria: microbial signature of dysbiosis in gut microbiota. Trend Biotechnol. 2015;33:496–503.
Stojanov S, Berlec A, Štrukelj B. The Influence of Probiotics on the Firmicutes/Bacteroidetes Ratio in the Treatment of Obesity and Inflammatory Bowel disease. Microorganisms. 2020;8:1715.
Carvalho FA, Koren O, Goodrich JK, Johansson ME, Nalbantoglu I, Aitken JD, et al. Transient inability to manage proteobacteria promotes chronic gut inflammation in TLR5-deficient mice. Cell Host Microbe. 2012;12:139–52.
Cryan JF, O’Riordan KJ, Sandhu K, Peterson V, Dinan TG. The gut microbiome in neurological disorders. Lancet Neurol. 2020;19:179–94.
Ganesh BP, Klopfleisch R, Loh G, Blaut M. Commensal Akkermansia muciniphila exacerbates gut inflammation in Salmonella Typhimurium-infected gnotobiotic mice. PloS One. 2013;8:e74963.
Jasper H. Intestinal Stem Cell Aging: Origins and Interventions. Annu Rev Physiol. 2020;82:203–26.
Rothhammer V, Quintana FJ. The aryl hydrocarbon receptor: an environmental sensor integrating immune responses in health and disease. Nature Rev Immunol. 2019;19:184–97.
Acknowledgements
We acknowledge MD Anderson Advanced Microscopy Core Facility, NIH grant (S10RR029552) and Microbiome Insights Inc., Vancouver, Canada (SCFAs analysis), and the infrastructure and support of the Alkek Center for Metagenomics and Microbiome Research – CMMR (16S rRNA sequencing). This work was supported by startup funds from The University of Texas Health Science Center at Houston to RM and TB, Alzheimer’s Association® AARGDNTF-19-619645 and TARCC 2022-24 to TB, NIH/NIA grant 1RF1AG072491 to RM and TB, and FAPESP grant 21/06496-4 to CHRC.
Author information
Authors and Affiliations
Contributions
Conception and design of the work, TB, RM, and VVG; acquisition, analysis, interpretation of data, VVG; brain and gut amyloid-beta evaluation, CSGC; gut microbiome analysis, VVG and JL; gut immunofluorescence and analysis, BPG; and have drafted the work TB and VVG; substantively revised the manuscript CHRC, FP, FD, RM, TB and VG.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: In this article the wrong figure appeared as Fig. 3F and 3J.; the figure should have appeared as shown below.The original article has been corrected.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Giridharan, V.V., Catumbela, C.S.G., Catalão, C.H.R. et al. Sepsis exacerbates Alzheimer’s disease pathophysiology, modulates the gut microbiome, increases neuroinflammation and amyloid burden. Mol Psychiatry 28, 4463–4473 (2023). https://doi.org/10.1038/s41380-023-02172-2
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41380-023-02172-2
This article is cited by
-
The Crosstalk Between Sepsis-Associated Encephalopathy and Alzheimer’s Disease: Identifying Potential Biomarkers and Therapeutic Targets for Cognition
Molecular Neurobiology (2025)
-
The endotoxin hypothesis of Alzheimer’s disease
Molecular Neurodegeneration (2024)