Abstract
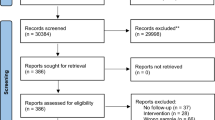
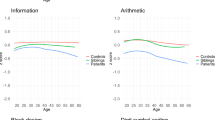
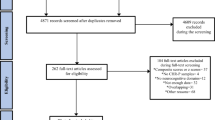
Earlier research suggested that psychotic experiences (PEs), the extended-psychosis phenotype, are associated with cognitive impairment. Recent studies, however, revealed more mixed findings, and patterns and magnitude of cognitive deficits in PEs remain uncertain. We aimed to systematically review and quantitatively synthesize estimates of cognitive functioning covering a wide array of domains in individuals with versus without PEs. We systematically searched four databases from inception to 6 July 2023. We generated pooled effect size (Hedges’g) using random-effects models. Subgroup analyses and meta-regression examining the moderating effect of sex, age at PE assessment, study design, cognitive task, and PE assessment instrument on cognitive functioning were performed when applicable. The study was registered with PROSPERO (CRD42023442528). Twenty-seven and six studies were included for meta-analysis of cognitive functioning comparing individuals with versus without PEs (n = 82,561; 10,251 individuals with PEs) and individuals with high-level versus low-level PEs (n = 8062; 813 individuals with high-level PEs), respectively. Individuals with PEs exhibited worse cognitive performance in general cognition (Hedges’g = −0.10 [95%CI = −0.18 to −0.02]), verbal fluency (Hedges’g = −0.05 [95%CI = −0.10 to −0.00]), visual memory (Hedges’g = −0.21 [95%CI = −0.38 to −0.03]), and working memory (Hedges’g = −0.16 [95%CI = −0.28 to −0.04]). Meta-regression revealed that general cognition associated with PEs was related to younger age (z = 3.37, p = 0.001), male sex (z = −2.59, p = 0.010), and cognitive assessment before PE assessment (z = −2.15, p = 0.031), whereas working memory in individuals with PEs was associated with concurrent cognitive and PE assessment (z = 6.19, p < 0.001). We failed to find moderating effect of the choice of PE assessment instrument or cognitive task on cognitive functioning in PEs. Additional analysis showed no significant difference in the performance of any cognitive domains between individuals with high-level versus low-level PEs. Limitations included studies primarily derived from Western countries, no social-cognitive domains, and varied PE measurement. In sum, PEs are associated with milder and more circumscribed cognitive impairment relative to psychotic disorders. Future research is required to clarify differential cognitive trajectories between individuals with transient PEs and persistent/recurrent-PEs.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Rajji TK, Ismail Z, Mulsant BH. Age at onset and cognition in schizophrenia: meta-analysis. BJPsych. 2009;195:286–93.
Mesholam-Gately RI, Giuliano AJ, Goff KP, Faraone SV, Seidman LJ. Neurocognition in first-episode schizophrenia: a meta-analytic review. Neuropsychology. 2009;23:315.
Szöke A, Trandafir A, Dupont ME, Méary A, Schürhoff F, Leboyer M. Longitudinal studies of cognition in schizophrenia: meta-analysis. BJPsych. 2008;192:248–57.
McCutcheon RA, Keefe RSE, McGuire PK. Cognitive impairment in schizophrenia: aetiology, pathophysiology, and treatment. Mol Psychiatry. 2023;28:1902–18.
Fett AKJ, Reichenberg A, Velthorst E. Lifespan evolution of neurocognitive impairment in schizophrenia - a narrative review. Schizophr Res Cogn. 2022;28:100237.
Catalan A, Salazar De Pablo G, Aymerich C, Damiani S, Sordi V, Radua J, et al. Neurocognitive functioning in individuals at clinical high risk for psychosis: a systematic review and meta-analysis. JAMA Psychiatry. 2021;78:859–67.
Fusar-Poli P, Deste G, Smieskova R, Barlati S, Yung AR, Howes Oliver, et al. Cognitive functioning in prodromal psychosis: a meta-analysis. Arch Gen Psychiatry. 2012;69:562–71.
Snitz BE, MacDonald AW, Carter CS. Cognitive deficits in unaffected first-degree relatives of schizophrenia patients: a meta-analytic review of putative endophenotypes. Schizophr Bull. 2006;32:179–94.
Mollon J, Reichenberg A. Cognitive development prior to onset of psychosis. Psychol Med. 2018;48:392–403.
Lewis R. Should cognitive deficit be a diagnostic criterion for schizophrenia? J. Psychiatry Neurosci. 2004;29:102–13.
Bowie CR, Harvey PD. Cognitive deficits and functional outcome in schizophrenia. Neuropsychiatr Dis Treat. 2006;2:531–6.
Linscott RJ, Van Os J. An updated and conservative systematic review and meta-analysis of epidemiological evidence on psychotic experiences in children and adults: on the pathway from proneness to persistence to dimensional expression across mental disorders. Psychol Med. 2013;43:1133–49.
Kelleher I, Connor D, Clarke MC, Devlin N, Harley M, Cannon M. Prevalence of psychotic symptoms in childhood and adolescence: a systematic review and meta-analysis of population-based studies. Psychol Med. 2012;42:1857–63.
Staines L, Healy C, Murphy F, Byrne J, Murphy J, Kelleher I, et al. Incidence and persistence of psychotic experiences in the general population: systematic review and meta-analysis. Schizophr Bull. 2023. https://doi.org/10.1093/schbul/sbad056.
Van Os J. Is there a continuum of psychotic experiences in the general population? Epidemiol Psichiatr Soc. 2003;12:242–52.
Van Os J, Linscott RJ, Myin-Germeys I, Delespaul P, Krabbendam L. A systematic review and meta-analysis of the psychosis continuum: evidence for a psychosis proneness-persistence-impairment model of psychotic disorder. Psychol Med. 2009;39:179–95.
Healy C, Brannigan R, Dooley N, Coughlan H, Clarke M, Kelleher I, et al. Childhood and adolescent psychotic experiences and risk of mental disorder: a systematic review and meta-analysis. Psychol Med. 2019;49:1589–99.
Kelleher I, Cannon M. Psychotic-like experiences in the general population: characterizing a high-risk group for psychosis. Psychol Med. 2011;41:1–6.
Staines L, Healy C, Coughlan H, Clarke M, Kelleher I, Cotter D, et al. Psychotic experiences in the general population, a review; definition, risk factors, outcomes and interventions. Psychol Med. 2022;52:3297–308.
McGorry PD, Hartmann JA, Spooner R, Nelson B. Beyond the “at risk mental state” concept: transitioning to transdiagnostic psychiatry. World Psychiatry. 2018;17:133–42.
Van Os J, Reininghaus U. Psychosis as a transdiagnostic and extended phenotype in the general population. World Psychiatry. 2016;15:118–24.
Scott KM, Saha S, Lim CCW, Aguilar-Gaxiola S, Al-Hamzawi A, Alonso J, et al. Psychotic experiences and general medical conditions: a cross-national analysis based on 28 002 respondents from 16 countries in the WHO World Mental Health Surveys. Psychol Med. 2018;48:2730–9.
Alonso J, Saha S, Lim CCW, Aguilar-Gaxiola S, Al-Hamzawi A, Benjet C, et al. The association between psychotic experiences and health-related quality of life: a cross-national analysis based on World Mental Health Surveys. Schizophr Res. 2018;201:46–53.
Mollon J, David AS, Morgan C, Frissa S, Glahn D, Pilecka I, et al. Psychotic experiences and neuropsychological functioning in a population-based sample. JAMA Psychiatry. 2016;73:129–38.
Mollon J, David AS, Zammit S, Lewis G, Reichenberg A. Course of cognitive development from infancy to early adulthood in the psychosis spectrum. JAMA Psychiatry. 2018;75:270–9.
Reininghaus U, Rauschenberg C, Ten Have M, De Graaf R, Van Dorsselaer S, Simons CJP, et al. Reasoning bias, working memory performance and a transdiagnostic phenotype of affective disturbances and psychotic experiences in the general population. Psychol Med. 2019;49:1799–809.
Newbury JB, Arseneault L, Moffitt TE, Odgers CL, Howe LD, Bakolis I, et al. Socioenvironmental adversity and adolescent psychotic experiences: Exploring potential mechanisms in a UK longitudinal cohort. Schizophr Bull. 2023;49:1042–54.
Guerrero-Jiménez M, Gutiérrez B, Ruiz I, Rodríguez-Barranco M, Ibanez-Casas I, Perez-Garcia M, et al. A cross-sectional survey of psychotic symptoms in the community: The GRANAD∑P psychosis study. Eur J Psychiatry. 2018;32:87–96.
Carey E, Gillan D, Burke T, Burns A, Murphy TM, Kelleher I, et al. Social cognition and self-reported ASD traits in young adults who have reported psychotic experiences: A population-based, longitudinal study. Schizophr Res. 2021;237:54–61.
Carey E, Gillan D, Healy C, Dooley N, Campbell D, McGrane J, et al. Early adult mental health, functional and neuropsychological outcomes of young people who have reported psychotic experiences: a 10-year longitudinal study. Psychol Med. 2021;51:1861–9.
Bosma MJ, Cox SR, Ziermans T, Buchanan CR, Shen X, Tucker-Drob EM, et al. White matter, cognition and psychotic-like experiences in UK Biobank. Psychol Med. 2023;53:2370–9.
Pignon B, Geoffroy PA, Gharib A, Thomas P, Moutot D, Brabant W, et al. Very early hallucinatory experiences: a school-based study. J Child Psychol Psychiatry. 2018;59:68–75.
McCarthy-Jones S. Post-traumatic symptomatology and compulsions as potential mediators of the relation between child sexual abuse and auditory verbal hallucinations. Behav Cogn Psychother. 2018;46:318–31.
Soulas T, Cleret de Langavant L, Monod V, Fénelon G. The prevalence and characteristics of hallucinations, delusions and minor phenomena in a non-demented population sample aged 60 years and over. Int J Geriatr Psychiatry. 2016;31:1322–8.
Peters E, Ward T, Jackson M, Morgan C, Charalambides M, McGuire P, et al. Clinical, socio-demographic and psychological characteristics in individuals with persistent psychotic experiences with and without a ‘need for care. World Psychiatry. 2016;15:41–52.
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analysis. 2000.
Kern RS, Nuechterlein KH, Green MF, Baade LE, Fenton WS, Gold JM, et al. The MATRICS Consensus Cognitive Battery, part 2: co-norming and standardization. Am J Psychiatry. 2008;165:214–20.
Nuechterlein KH, Green MF, Kern RS, Baade LE, Barch DM, Cohen JD, et al. The MATRICS Consensus Cognitive Battery, part 1: test selection, reliability, and validity. Am J Psychiatry. 2008;165:203–13.
Dijkstra L, Vermeulen J, de Haan L, Schirmbeck F. Meta-analysis of cognitive functioning in patients with psychotic disorders and obsessive–compulsive symptoms. Eur Arch Psychiatry Clin Neurosci. 2021;271:689–706.
Watson AJ, Harrison L, Preti A, Wykes T, Cella M. Cognitive trajectories following onset of psychosis: a meta-analysis. BJPsych. 2022;221:714–21.
Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. Br Med J. 1997;315:629–34.
Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Softw. 2010;36:1–48.
Cannon M, Caspi A, Moffitt TE, Harrington H, Taylor A, Murray RM, et al. Evidence for early-childhood, pan-developmental impairment specific to schizophreniform disorder: results from a longitudinal birth cohort. Arch Gen Psychiatry. 2002;59:449–56.
Horwood J, Salvi G, Thomas K, Duffy L, Gunnell D, Hollis C, et al. IQ and non-clinical psychotic symptoms in 12-year-olds: Results from the ALSPAC birth cohort. BJPsych. 2008;193:185–91.
Barnett JH, McDougall F, Xu MK, Croudace TJ, Richards M, Jones PB. Childhood cognitive function and adult psychopathology: Associations with psychotic and non-psychotic symptoms in the general population. BJPsych. 2012;201:124–30.
Polanczyk G, Moffitt TE, Arseneault L, Cannon M, Ambler A, Keefe RSE, et al. Etiological and clinical features of childhood psychotic symptoms results from a birth cohort. Arch Gen Psychiatry. 2010;67:328–38.
Wikström A, Tuulio-Henriksson A, Perälä J, Saarni S, Suvisaari J. Psychotic like experiences (PLE’s) in middle-aged adults. Schizophr Res. 2015;169:313–7.
Bourque J, Afzali MH, O’Leary-Barrett M, Conrod P. Cannabis use and psychotic-like experiences trajectories during early adolescence: the coevolution and potential mediators. J Child Psychol Psychiatry. 2017;58:1360–9.
Ibanez-Casas I, Carmen Maura C de AC, Gutiérrez B, Cervilla JA. A population-based cross-sectional study of cognitive deficits in paranoia. Psychiatry Res. 2021;299:113820.
Woodberry KA, Anthony Giuliano AJ, Seidman LJ. Premorbid IQ in schizophrenia: a meta-analytic review. Am J Psychiatry. 2008;165:579–87.
Dickinson D. Digit symbol coding and general cognitive ability in schizophrenia: Worth another look? BJPsych. 2008;193:354–6.
Knowles EE, David AS, Reichenberg A. Processing speed deficits in schizophrenia: reexamining the evidence. Am J Psychiatry. 2010;167:828–35.
Dickinson D, Ramsey ME, Gold JM. Overlooking the obvious: a meta-analytic comparison of digit symbol coding tasks and other cognitive measures in schizophrenia. Arch Gen Psychiatry. 2007;64:532–42.
Chu AOK, Chang WC, Chan SKW, Lee EHM, Hui CLM, Chen EYH. Comparison of cognitive functions between first-episode schizophrenia patients, their unaffected siblings and individuals at clinical high-risk for psychosis. Psychol Med. 2019;49:1929–36.
Millman ZB, Roemer C, Vargas T, Schiffman J, Mittal VA, Gold JM. Neuropsychological performance among individuals at clinical high-risk for psychosis vs putatively low-risk peers with other psychopathology: a systematic review and meta-analysis. Schizophr Bull. 2022;48:999–1010.
Dominguez MDG, Wichers M, Lieb R, Wittchen HU, Van Os J. Evidence that onset of clinical psychosis is an outcome of progressively more persistent subclinical psychotic experiences: an 8-year cohort study. Schizophr Bull. 2011;37:84–93.
Rammos A, Sullivan SA, Kounali D, Jones HJ, Hammerton G, Hines LA, et al. Precursors and correlates of transient and persistent longitudinal profiles of psychotic experiences from late childhood through early adulthood. BJPsych. 2022;220:330–8.
Kelleher I, Clarke MC, Rawdon C, Murphy J, Cannon M. Neurocognition in the extended psychosis phenotype: Performance of a community sample of adolescents with psychotic symptoms on the matrics neurocognitive battery. Schizophr Bull. 2013;39:1018–26.
Krabbendam L, Myin-Germeys I, Hanssen M, Van Os J. Familial covariation of the subclinical psychosis phenotype and verbal fluency in the general population. Schizophr Res. 2005;74:37–41.
Mendrek A, Mancini-Marïe A. Sex/gender differences in the brain and cognition in schizophrenia. Neurosci Biobehav Rev. 2016;67:57–78.
Fatouros-Bergman H, Cervenka S, Flyckt L, Edman G, Farde L. Meta-analysis of cognitive performance in drug-naïve patients with schizophrenia. Schizophr Res. 2014;158:156–62.
Leger M, Neill JC. A systematic review comparing sex differences in cognitive function in schizophrenia and in rodent models for schizophrenia, implications for improved therapeutic strategies. Neurosci Biobehav Rev. 2016;68:979–1000.
Johns LC, Cannon M, Singleton N, Murray RM, Farrell M, Brugha T, et al. Prevalence and correlates of self-reported psychotic symptoms in the British population. Br J Psychiatry. 2004;185:298–305.
Daalman K, van Zandvoort M, Bootsman F, Boks M, Kahn R, Sommer I. Auditory verbal hallucinations and cognitive functioning in healthy individuals. Schizophr Res. 2011;132:203–7.
Koenen KC, Moffitt TE, Roberts AL, Martin LT, Kubzansky L, Harrington H, et al. Childhood IQ and adult mental disorders: a test of the cognitive reserve hypothesis. Am. J. Psychiatry. 2009;166:50–57.
Urfer-Parnas A, Lykke Mortensen E, Sbye D, Parnas J. Pre-morbid IQ in mental disorders: a Danish draft-board study of 7486 psychiatric patients. Psychol Med. 2010;40:547–56.
Chavez-Baldini U, Nieman DH, Keestra A, Lok A, Mocking RJT, De Koning P, et al. The relationship between cognitive functioning and psychopathology in patients with psychiatric disorders: a transdiagnostic network analysis. Psychol Med. 2023;53:476–85.
Köhler S, Allardyce J, Verhey FRJ, McKeith IG, Matthews F, Brayne C, et al. Cognitive decline and dementia risk in older adults with psychotic symptoms: a prospective cohort study. Am J Geriatr Psychiatry. 2013;21:119–28.
Östling S, Gustafson D, Blennow K, Börjesson-Hanson A, Waern M. Psychotic symptoms in a population-based sample of 85-year-old individuals with dementia. J Geriatr Psychiatry Neurol. 2011;24:3–8.
Lee KW, Chan KW, Chang WC, Lee EHM, Hui CLM, Chen EYH. A systematic review on definitions and assessments of psychotic-like experiences. Early Interv Psychiatry. 2016;10:3–16.
Seiler N, Nguyen T, Yung A, O’Donoghue B. Terminology and assessment tools of psychosis: a systematic narrative review. Psychiatry Clin Neurosci. 2020;74:226–46.
Maitra R, Horne CM, O’Daly O, Papanastasiou E, Gaser C, Banaschewski T, et al. Psychotic like experiences in healthy adolescents are underpinned by lower fronto-temporal cortical gyrification: a study from the IMAGEN Consortium. Schizophr Bull. 2023;49:309–18.
Korponay C, Nitzburg GC, Malhotra AK, DeRosse P. Positive and negative subclinical symptoms and MCCB performance in non-psychiatric controls. Schizophr Res Cogn. 2014;1:175–9.
Livet A, Navarri X, Potvin S, Conrod P. Cognitive biases in individuals with psychotic-like experiences: a systematic review and a meta-analysis. Schizophr Res. 2020;222:10–22.
McGrath JJ, Saha S, Al-Hamzawi A, Alonso J, Bromet EJ, Bruffaerts R, et al. Psychotic experiences in the general population: a cross- national analysis based on 31,261 respondents from 18 countries. JAMA Psychiatry. 2015;72:697–705.
Henderson AS, Korten AE, Levings C, Jorm AF, Christensen H, Jacomb PA, et al. Psychotic symptoms in the elderly: a prospective study in a population sample. Int J Geriatr Psychiatry. 1998;13:484–92.
Östling S, Johansson B, Skoog I. Cognitive test performance in relation to psychotic symptoms and paranoid ideation in non-demented 85-year-olds. Psychol Med. 2004;34:443–50.
Thompson A, Sullivan S, Heron J, Thomas K, Zammit S, Horwood J, et al. Childhood facial emotion recognition and psychosis-like symptoms in a nonclinical population at 12 years of age: Results from the ALSPAC birth cohort. Cogn Neuropsychiatry. 2011;16:136–57.
Niarchou M, Zammit S, Walters J, Lewis G, John Owen M, Bernadette van den Bree M. Defective processing speed and nonclinical psychotic experiences in children: longitudinal analyses in a large birth cohort. Am J Psychiatry. 2013;170:550–7.
Clemmensen L, Van Os J, Skovgaard AM, Væver M, Blijd-Hoogewys EMA, Bartels-Velthuis AA, et al. Hyper-theory-of-mind in children with psychotic experiences. PLoS ONE. 2014;9:e113082.
Gur RC, Calkins ME, Satterthwaite TD, Ruparel K, Bilker WB, Moore TM, et al. Neurocognitive growth charting in psychosis spectrum youths. JAMA Psychiatry. 2014;71:366–74.
Byrne GJ, Steele SJ, Pachana NA, Oude VoshaarRC. Delusion-like experiences in older people with anxiety disorders. Int Psychogeriatr. 2015;27:1191–6.
Grossman M, Best MW, Harrison AG, Bowie CR. Comparison of the neurocognitive profiles of individuals with elevated psychotic or depressive symptoms. Early Interv Psychiatry. 2019;13:928–34.
de Leede-Smith S, Roodenrys S, Horsley L, Matrini S, Mison E, Barkus E. Role for positive schizotypy and hallucination proneness in semantic processing. Front Psychol. 2020;11:542002.
Funding
The study was supported by the Health and Medical Research Fund (HMRF) (grant number: 07181776), the Food and Health Bureau, and the Hong Kong SAR Government. The funders had no role in study design, data collection, data analysis, interpretation of the data, manuscript preparation, or journal submission.
Author information
Authors and Affiliations
Contributions
WCC and RSTC conceptualized and proposed the topic. RSTC and WCC developed the protocol, designed the search strategy, and defined the inclusion criteria. RSTC, IWLC, and EYCY screened the literature research, and extracted data from included studies. RSTC and IWLC did the quality assessment of the included studies. RSTC did the statistical analyses. RSTC, WCC, JKNC, and CSMW interpreted the study data. RSTC wrote the first draft. WCC and RSTC finalized the manuscript. All authors critically reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chu, R.S.T., Chu, I.W.L., Yip, E.WC. et al. Cognitive functioning in people with psychotic experiences: a systematic review and meta-analysis study. Mol Psychiatry 30, 1184–1194 (2025). https://doi.org/10.1038/s41380-024-02823-y
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41380-024-02823-y