Abstract
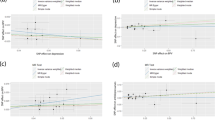
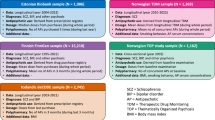
This study explores the genetic and epidemiologic correlates of long-term photoplethysmography-derived pulse rate variability (PRV) measurements with anxiety disorders. Individuals with whole-genome sequencing, Fitbit, and electronic health record data (N = 920; 61,333 data points) were selected from the All of Us Research Program. Anxiety polygenic risk scores (PRS) were derived with PRS-CS after meta-analyzing anxiety genome-wide association studies from three major cohorts- UK Biobank, FinnGen, and the Million Veterans Program (NTotal =364,550). PRV was estimated as the standard deviation of average five-minute pulse wave intervals over full 24-hour pulse rate measurements (SDANN). Antidepressant exposure was defined as an active antidepressant prescription at the time of the PRV measurement in the EHR. Anxiety PRS and antidepressant use were tested for association with daily SDANN. The potential causal effect of anxiety on PRV was assessed with one-sample Mendelian randomization (MR). Anxiety PRS was independently associated with reduced SDANN (beta = −0.08; p = 0.003). Of the eight antidepressant medications and four classes tested, venlafaxine (beta = −0.12, p = 0.002) and bupropion (beta = −0.071, p = 0.01), tricyclic antidepressants (beta = −0.177, p = 0.0008), selective serotonin reuptake inhibitors (beta = −0.069; p = 0.0008) and serotonin and norepinephrine reuptake inhibitors (beta = −0.16; p = 2×10−6) were associated with decreased SDANN. One-sample MR indicated an inverse effect of anxiety on SDANN (beta = −2.22, p = 0.03). Anxiety and antidepressants are independently associated with decreased PRV, and anxiety appears to exert a causal effect on reduced PRV. Those observational findings provide insights into the impact of anxiety on PRV.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
All data generated in the present study are reported in the manuscript and its supplemental material. All of Us Research Program data are available at https://allofus.nih.gov/get-involved/opportunities-researchers. UK Biobank genome-wide association statistics are available at https://pan.ukbb.broadinstitute.org/. FinnGen genome-wide association statistics are available at https://www.finngen.fi/en/access_results. Million Veteran Program genome-wide association statistics are available at https://www.ncbi.nlm.nih.gov/projects/gap/cgi-bin/study.cgi?study_id=phs001672.v11.p1.
References
Mejía-Mejía E, May JM, Torres R, Kyriacou PA. Pulse rate variability in cardiovascular health: a review on its applications and relationship with heart rate variability. Physiol Meas. 2020;41:07TR01.
Chalmers JA, Quintana DS, Abbott MJ, Kemp AH. Anxiety disorders are associated with reduced heart rate variability: a meta-analysis. Front Psychiatry. 2014;5:80.
Prieto-Avalos G, Cruz-Ramos NA, Alor-Hernández G, Sánchez-Cervantes JL, Rodríguez-Mazahua L, Guarneros-Nolasco LR. Wearable devices for physical monitoring of heart: a review. Biosensors 2022;12:292.
Cheng YC, Su MI, Liu CW, Huang YC, Huang WL. Heart rate variability in patients with anxiety disorders: a systematic review and meta-analysis. Psychiatry Clin Neurosci. 2022;76:292–302.
Fiani D, Campbell H, Solmi M, Fiedorowicz JG, Calarge CA. Impact of antidepressant use on the autonomic nervous system: a meta-analysis and systematic review. Eur Neuropsychopharmacol. 2023;71:75–95.
Hu MX, Milaneschi Y, Lamers F, Nolte IM, Snieder H, Dolan CV, et al. The association of depression and anxiety with cardiac autonomic activity: the role of confounding effects of antidepressants. Depress Anxiety. 2019;36:1163–72.
Kemp AH, Fráguas R, Brunoni AR, Bittencourt MS, Nunes MA, Dantas EM, et al. Differential associations of specific selective serotonin reuptake inhibitors with resting-state heart rate and heart rate variability: implications for health and well-being. Psychosom Med. 2016;78:810–8.
Giurgi-Oncu C, Tudoran C, Enatescu VR, Tudoran M, Pop GN, Bredicean C. Evolution of heart rate variability and heart rate turbulence in patients with depressive illness treated with selective serotonin reuptake inhibitors. Medicina 2020;56:590.
Can YS, Chalabianloo N, Ekiz D, Ersoy C. Continuous stress detection using wearable sensors in real life: algorithmic programming contest case study. Sensors 2019;19:1849.
Kobayashi M, Guanghao S, Shinba T, Matsui T, Kirimoto T. Simple and objective screening of major depressive disorder by heart rate variability analysis during paced respiration and mental task conditions. Annu Int Conf IEEE Eng Med Biol Soc. 2017;2017:1316–9.
Ask H, Cheesman R, Jami ES, Levey DF, Purves KL, Weber H. Genetic contributions to anxiety disorders: where we are and where we are heading. Psychol Med. 2021;51:2231–46.
Bycroft C, Freeman C, Petkova D, Band G, Elliott LT, Sharp K, et al. The UK Biobank resource with deep phenotyping and genomic data. Nature. 2018;562:203–9.
Gaziano JM, Concato J, Brophy M, Fiore L, Pyarajan S, Breeling J, et al. Million Veteran Program: a mega-biobank to study genetic influences on health and disease. J Clin Epidemiol. 2016;70:214–23.
Kurki MI, Karjalainen J, Palta P, Sipilä TP, Kristiansson K, Donner KM, et al. FinnGen provides genetic insights from a well-phenotyped isolated population. Nature. 2023;613:508–18.
Denny JC, Rutter JL, Goldstein DB, Philippakis A, Smoller JW, Jenkins G, et al. The “All of Us” research program. N Engl J Med. 2019;381:668–76.
Natarajan A, Pantelopoulos A, Emir-Farinas H, Natarajan P. Heart rate variability with photoplethysmography in 8 million individuals: a cross-sectional study. Lancet Digit Health. 2020;2:e650–e657.
Klann JG, Joss MAH, Embree K, Murphy SN. Data model harmonization for the All Of Us Research Program: transforming i2b2 data into the OMOP common data model. PLoS One. 2019;14:e0212463.
Stein KM, Borer JS, Hochreiter C, Okin PM, Herrold EM, Devereux RB, et al. Prognostic value and physiological correlates of heart rate variability in chronic severe mitral regurgitation. Circulation. 1993;88:127–35.
Huang M, Shah A, Su S, Goldberg J, Lampert RJ, Levantsevych OM, et al. Association of depressive symptoms and heart rate variability in Vietnam War-Era Twins: a longitudinal twin difference study. JAMA Psychiatry. 2018;75:705–12.
Longenecker JC, Zubaid M, Johny KV, Attia AI, Ali J, Rashed W, et al. Association of low heart rate variability with atherosclerotic cardiovascular disease in hemodialysis patients. Med Princ Pract. 2009;18:85–92.
Benichou T, Pereira B, Mermillod M, Tauveron I, Pfabigan D, Maqdasy S, et al. Heart rate variability in type 2 diabetes mellitus: a systematic review and meta-analysis. PLoS One. 2018;13:e0195166.
Karczewski KJ, Gupta R, Kanai M, Lu W, Tsuo K, Wang Y et al. Pan-UK Biobank GWAS improves discovery, analysis of genetic architecture, and resolution into ancestry-enriched effects. medRxiv 2024: 2024.2003.2013.24303864.
Mbatchou J, Barnard L, Backman J, Marcketta A, Kosmicki JA, Ziyatdinov A, et al. Computationally efficient whole-genome regression for quantitative and binary traits. Nat Genet. 2021;53:1097–103.
Levey DF, Gelernter J, Polimanti R, Zhou H, Cheng Z, Aslan M, et al. Reproducible genetic risk loci for anxiety: results from ∼200,000 participants in the Million Veteran Program. Am J Psychiatry. 2020;177:223–32.
Bulik-Sullivan BK, Loh P-R, Finucane HK, Ripke S, Yang J, Patterson N, et al. LD Score regression distinguishes confounding from polygenicity in genome-wide association studies. Nat Genet. 2015;47:291–5.
Willer CJ, Li Y, Abecasis GR. METAL: fast and efficient meta-analysis of genomewide association scans. Bioinformatics. 2010;26:2190–1.
Lee CH, Cook S, Lee JS, Han B. Comparison of two meta-analysis methods: inverse-variance-weighted average and weighted sum of Z-scores. Genom Inform. 2016;14:173–80.
Ge T, Chen C-Y, Ni Y, Feng Y-CA, Smoller JW. Polygenic prediction via Bayesian regression and continuous shrinkage priors. Nat Commun. 2019;10:1776.
Purcell S, Neale B, Todd-Brown K, Thomas L, Ferreira MA, Bender D, et al. PLINK: a tool set for whole-genome association and population-based linkage analyses. Am J Hum Genet. 2007;81:559–75.
Dekker JM, Crow RS, Folsom AR, Hannan PJ, Liao D, Swenne CA, et al. Low heart rate variability in a 2-min rhythm strip predicts risk of coronary heart disease and mortality from several causes: the ARIC Study. Atherosclerosis risk in communities. Circulation. 2000;102:1239–44.
Davey Smith G, Hemani G. Mendelian randomization: genetic anchors for causal inference in epidemiological studies. Hum Mol Genet. 2014;23:R89–98.
Nagin DS, Jones BL, Lima Passos V, Tremblay RE. Group-based multi-trajectory modeling. Stat Methods Med Res. 2018;27:2015–23.
Santomauro DF, Mantilla Herrera AM, Shadid J, Zheng P, Ashbaugh C, Pigott DM, et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021;398:1700–12.
Kircanski K, Williams LM, Gotlib IH. Heart rate variability as a biomarker of anxious depression response to antidepressant medication. Depress Anxiety. 2019;36:63–71.
Jacobson NC, Feng B. Digital phenotyping of generalized anxiety disorder: using artificial intelligence to accurately predict symptom severity using wearable sensors in daily life. Transl Psychiatry. 2022;12:336.
Nolte IM, Munoz ML, Tragante V, Amare AT, Jansen R, Vaez A, et al. Genetic loci associated with heart rate variability and their effects on cardiac disease risk. Nat Commun. 2017;8:15805.
Frey B, Heinz G, Binder T, Wutte M, Schneider B, Schmidinger H, et al. Diurnal variation of ventricular response to atrial fibrillation in patients with advanced heart failure. Am Heart J. 1995;129:58–65.
Roach D, Wilson W, Ritchie D, Sheldon R. Dissection of long-range heart rate variability: controlled induction of prognostic measures by activity in the laboratory. J Am Coll Cardiol. 2004;43:2271–7.
Davidson J, Watkins L, Owens M, Krulewicz S, Connor K, Carpenter D, et al. Effects of paroxetine and venlafaxine XR on heart rate variability in depression. J Clin Psychopharmacol. 2005;25:480–4.
Siepmann M, Werner K, Schindler C, Mück-Weymann M, Kirch W. The effects of bupropion on heart rate variability in healthy volunteers. J Clin Psychopharmacol. 2005;25:283–5.
Patrone LGA, Capalbo AC, Marques DA, Bícego KC, Gargaglioni LH. An age- and sex-dependent role of catecholaminergic neurons in the control of breathing and hypoxic chemoreflex during postnatal development. Brain Res. 2020;1726:146508.
Leong C, Alessi-Severini S, Enns MW, Nie Y, Sareen J, Bolton J, et al. Cerebrovascular, cardiovascular, and mortality events in new users of selective serotonin reuptake inhibitors and serotonin norepinephrine reuptake inhibitors: a propensity score-matched population-based study. J Clin Psychopharmacol. 2017;37:332–40.
Kleiger RE, Bigger JT, Bosner MS, Chung MK, Cook JR, Rolnitzky LM, et al. Stability over time of variables measuring heart rate variability in normal subjects. Am J Cardiol. 1991;68:626–30.
Zhao R, Li D, Zuo P, Bai R, Zhou Q, Fan J, et al. Influences of age, gender, and circadian rhythm on deceleration capacity in subjects without evident heart diseases. Ann Noninvasive Electrocardiol. 2015;20:158–66.
Acknowledgements
The authors thank the participants and the investigators involved in the UK Biobank, the FinnGen Project, the Million Veteran Program, and the All of Us Research Program. This study was supported by grants from One Mind and the National Institutes of Health (RF1 MH132337, R33 DA047527, T32 MH014276, and K99 AG078503). The All of Us Research Program is supported by the National Institutes of Health, Office of the Director: Regional Medical Centers: 1 OT2 OD026549; 1 OT2 OD026554; 1 OT2 OD026557; 1 OT2 OD026556; 1 OT2 OD026550; 1 OT2 OD 026552; 1 OT2 OD026553; 1 OT2 OD026548; 1 OT2 OD026551; 1 OT2 OD026555; IAA #: AOD 16037; Federally Qualified Health Centers: HHSN 263201600085U; Data and Research Center: 5 U2C OD023196; Biobank: 1 U24 OD023121; The Participant Center: U24 OD023176; Participant Technology Systems Center: 1 U24 OD023163; Communications and Engagement: 3 OT2 OD023205; 3 OT2 OD023206; and Community Partners: 1 OT2 OD025277; 3 OT2 OD025315; 1 OT2 OD025337; 1 OT2 OD025276. In addition, the All of Us Research Program would not be possible without the partnership of its participants.
Author information
Authors and Affiliations
Contributions
EF and RP designed the study. EF analyzed the data. DK and GAP supported the statistical analyses. EJM, RL, and MBS supported the analyses of the clinical variables. EF and RP wrote the manuscript. All the other authors provided critical feedback, context interpretation, draft revision, and editing. RP supervised the study and received the primary funding that supported the study.
Corresponding authors
Ethics declarations
Competing interests
RP reported receiving personal fees for editorial work on the journal Complex Psychiatry from Karger Publishers and a research grant from Alkermes outside the submitted work. MBS reported consulting for Acadia Pharmaceuticals Inc., Aptinyx Inc., ATAI Life Sciences, Biogen Inc., Bionomics, BigHealth, BioXcel Therapeutics Inc, Boehringer Ingelheim, Clexio Biosciences Ltd, Eisai Co Ltd, EmpowerPharm, Engrail Therapeutics, Janssen Pharmaceuticals, Jazz Pharmaceuticals, NeuroTrauma Sciences LLC, PureTech Health, Sage Therapeutics, Sumitomo Pharma Co Ltd, and Roche-Genentech; and receiving stock options from Oxeia Biopharmaceuticals Inc and EpiVario outside the submitted work; serving as editor in chief for Depression and Anxiety, deputy editor for Biological Psychiatry, and co-editor in chief for Psychiatry for UpToDate for compensation. RL reported receiving speaker honoraria, advisory board fees, and research funding from Medtronic; speaker honoraria and research funding from Abbott/St Jude; and research funding from Boston Scientific. EJM reported consulting for Eidos, Pfizer, Siemens, Alnylam, and Roivant and receiving research funding from Eidos, Pfizer, and Argospect. No other disclosures were reported.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Friligkou, E., Koller, D., Pathak, G.A. et al. Integrating genome-wide information and wearable device data to explore the link of anxiety and antidepressants with pulse rate variability. Mol Psychiatry 30, 2309–2315 (2025). https://doi.org/10.1038/s41380-024-02836-7
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41380-024-02836-7