Abstract
Background/objectives
Dysregulation of molecular pathways associated with mechanistic target of rapamycin (mTOR) and elevated rates of neurodevelopmental disorders are implicated in the genetic syndromes neurofibromatosis type 1 (NF1), tuberous sclerosis complex (TSC), fragile X syndrome (FXS), and Noonan syndrome (NS). Given shared molecular and clinical features, understanding convergent and divergent implications of these syndromes on brain development may offer unique insights into disease mechanisms. While an increasing number of studies have examined brain volumes in these syndromes, the effects of each syndrome on global and subcortical brain volumes are unclear. Therefore, the aim of the current study was to conduct a systematic review and meta-analysis to synthesize existing literature on volumetric brain changes across TSC, FXS, NF1, and NS. Study outcomes were the effect sizes of the genetic syndromes on whole brain, gray and white matter, and subcortical volumes compared to typically developing controls.
Subjects/methods
We performed a series of meta-analyses synthesizing data from 23 studies in NF1, TSC, FXS, and NS (pooled N = 1556) reporting whole brain volume, gray and white matter volumes, and volumes of subcortical structures compared to controls.
Results
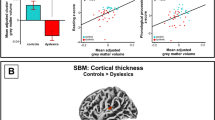
Meta-analyses revealed significantly larger whole brain volume, gray and white matter volumes, and subcortical volumes in NF1 compared to controls. FXS was associated with increased whole brain, and gray and white matter volumes relative to controls, but effect sizes were smaller than those seen in NF1. In contrast, studies in NS indicated smaller whole brain and gray matter volumes, and reduced subcortical volumes compared to controls. For individuals with TSC, there were no significant differences in whole brain, gray matter, and white volumes compared to controls. Volumetric effect sizes were not moderated by age, sex, or full-scale IQ.
Conclusions
This meta-analysis revealed that dysregulation of mTOR signaling across pre- and post-natal periods of development can result in convergent and divergent consequences for brain volume among genetic syndromes. Further research employing advanced disease modeling techniques with human pluripotent stem cell-derived in vitro models is needed to further refine our understanding of between and within syndrome variability on early brain development and identify shared molecular mechanisms for the development of pharmaceutical interventions.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
Data used of the current study were reported in articles as cited in this paper.
References
Stiles J, Jernigan TL. The basics of brain development. Neuropsychol Rev. 2010;20:327–48.
Kostović I, Jovanov-Milosević N. The development of cerebral connections during the first 20-45 weeks’ gestation. Semin Fetal Neonatal Med. 2006;11:415–22.
Gressens P. Mechanisms and disturbances of neuronal migration. Pediatr Res. 2000;48:725–30.
Bae BI, Jayaraman D, Walsh CA. Genetic changes shaping the human brain. Dev Cell. 2015;32:423–34.
Hashem S, Nisar S, Bhat AA, Yadav SK, Azeem MW, Bagga P, et al. Genetics of structural and functional brain changes in autism spectrum disorder. Transl Psychiatry. 2020;10:229.
Betancur C. Etiological heterogeneity in autism spectrum disorders: more than 100 genetic and genomic disorders and still counting. Brain Res. 2011;1380:42–77.
Amor DJ. Investigating the child with intellectual disability. J Paediatr Child Health. 2018;54:1154–8.
Inoki K, Corradetti MN, Guan KL. Dysregulation of the TSC-mTOR pathway in human disease. Nat Genet. 2005;37:19–24.
Veenstra-VanderWeele J, Blakely RD. Networking in autism: leveraging genetic, biomarker and model system findings in the search for new treatments. Neuropsychopharmacol. 2012;37:196–212.
Laplante M, Sabatini DM. mTOR signaling at a glance. J Cell Sci. 2009;122:3589.
Saxton RA, Sabatini DM. mTOR signaling in growth, metabolism, and disease. Cell. 2017;168:960–76.
Takei N, Nawa H. mTOR signaling and its roles in normal and abnormal brain development. Front Mol Neurosci. 2014;7:28.
Switon K, Kotulska K, Janusz-Kaminska A, Zmorzynska J, Jaworski J. Molecular neurobiology of mTOR. Neurosci. 2017;341:112–53.
Lipton JO, Sahin M. The neurology of mTOR. Neuron. 2014;84:275–91.
Lee DY. Roles of mTOR signaling in brain development. Exp Neurobiol. 2015;24:177–85.
Johannessen CM, Reczek EE, James MF, Brems H, Legius E, Cichowski K. The NF1 tumor suppressor critically regulates TSC2 and mTOR. Proc Nat Acad Sci USA. 2005;102:8573–8.
Hobert JA, Eng C. PTEN hamartoma tumor syndrome: an overview. Genet Med. 2009;11:687–94.
Liu W, Yu WM, Zhang J, Chan RJ, Loh ML, Zhang Z, et al. Inhibition of the Gab2/PI3K/mTOR signaling ameliorates myeloid malignancy caused by Ptpn11 (Shp2) gain-of-function mutations. Leukemia. 2017;31:1415–22.
Sharma A, Hoeffer CA, Takayasu Y, Miyawaki T, McBride SM, Klann E, et al. Dysregulation of mTOR signaling in fragile X syndrome. J Neurosci. 2010;30:694–702.
Chaste P, Betancur C, Gérard-Blanluet M, Bargiacchi A, Kuzbari S, Drunat S, et al. High-functioning autism spectrum disorder and fragile X syndrome: report of two affected sisters. Mol Autism. 2012;3:5.
Chisholm AK, Anderson V, Pride NA, Malarbi S, North KN, Payne JM. Social function and autism spectrum disorder in children and adults with neurofibromatosis type 1: a systematic review and meta-analysis. Neuropsychol Rev. 2018;28:317–40.
Crino PB, Nathanson KL, Henske EP. The tuberous sclerosis complex. N Engl J Med. 2006;355:1345–56.
Bruno JL, Romano D, Mazaika P, Lightbody AA, Hazlett HC, Piven J, et al. Longitudinal identification of clinically distinct neurophenotypes in young children with fragile X syndrome. Proc Natl Acad Sci USA. 2017;114:10767–72.
Garg S, Brooks A, Burns A, Burkitt-Wright E, Kerr B, Huson S, et al. Autism spectrum disorder and other neurobehavioural comorbidities in rare disorders of the Ras/MAPK pathway. Dev Med Child Neurol. 2017;59:544–9.
Hansen-Kiss E, Beinkampen S, Adler B, Frazier T, Prior T, Erdman S, et al. A retrospective chart review of the features of PTEN hamartoma tumour syndrome in children. J Med Genet. 2017;54:471–8.
Payne JM, Haebich KH, MacKenzie R, Walsh KS, Hearps SJC, Coghill D, et al. Cognition, ADHD symptoms, and functional impairment in children and adolescents with neurofibromatosis type 1. J Atten Disord. 2021;25:1177–86.
D’Agati E, Moavero R, Cerminara C, Curatolo P. Attention-deficit hyperactivity disorder (ADHD) and tuberous sclerosis complex. J Child Neurol. 2009;24:1282–7.
Grefer M, Flory K, Cornish K, Hatton D, Roberts J. The emergence and stability of attention deficit hyperactivity disorder in boys with fragile X syndrome. J Iintellect Disabil Res. 2016;60:167–78.
Payne JM, Hearps SJC, Walsh KS, Paltin I, Barton B, Ullrich NJ, et al. Reproducibility of cognitive endpoints in clinical trials: lessons from neurofibromatosis type 1. Ann Clin Transl Neurol. 2019;6:2555–65.
van Eeghen AM, Black ME, Pulsifer MB, Kwiatkowski DJ, Thiele EA. Genotype and cognitive phenotype of patients with tuberous sclerosis complex. Eur J Hum Genet. 2012;20:510–5.
Salcedo-Arellano MJ, Dufour B, McLennan Y, Martinez-Cerdeno V, Hagerman R. Fragile X syndrome and associated disorders: Clinical aspects and pathology. Neurobiol Dis. 2020;136:104740.
Santoro C, Bernardo P, Coppola A, Pugliese U, Cirillo M, Giugliano T, et al. Seizures in children with neurofibromatosis type 1: is neurofibromatosis type 1 enough? Ital J Pediatr. 2018;44:41.
Nguyen LH, Mahadeo T, Bordey A. mTOR hyperactivity levels influence the severity of epilepsy and associated neuropathology in an experimental model of tuberous sclerosis complex and focal cortical dysplasia. J Neurosci. 2019;39:2762.
Payne JM, Moharir MD, Webster R, North KN. Brain structure and function in neurofibromatosis type 1: current concepts and future directions. J Neurol Neurosurg Psychiatry. 2010;81:304–9.
Schapiro MB, Murphy DG, Hagerman RJ, Azari NP, Alexander GE, Miezejeski CM, et al. Adult fragile X syndrome: neuropsychology, brain anatomy, and metabolism. Am J Med Genet. 1995;60:480–93.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097.
Hazlett HC, Poe MD, Lightbody AA, Styner M, MacFall JR, Reiss AL, et al. Trajectories of early brain volume development in fragile X syndrome and autism. J Am Acad Child Adolesc Psychiatry. 2012;51:921–33.
Hedges LV. Distribution theory for Glass’s estimator of effect size and related estimators. J Ed Stat. 1981;6:107–28.
Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale: Lawrence Erlbaum; 1988.
Borenstein M. Introduction to meta-analysis. Chichester, U.K.: John Wiley & Sons; 2009.
Duval S, Tweedie R. Trim and Fill: A simple funnel-plot–based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56:455–63.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60.
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2013, https://www.ohri.ca//programs/clinical_epidemiology/oxford.asp.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–6.
Cutting LE, Koth CW, Burnette CP, Abrams MT, Kaufmann WE, Denckla MB. Relationship of cognitive functioning, whole brain volumes, and T2-weighted hyperintensities in neurofibromatosis-1. J Child Neurol. 2000;15:157–60.
Siqueiros-Sanchez M, Rai B, Chowdhury S, Reiss AL, Green T. Syndrome-specific neuroanatomical phenotypes in girls With Turner and Noonan syndromes. Biol Psychiatry Cogn Neurosci Neuroimaging. 2024;9:146–55.
Wilson LB, Tregellas JR, Hagerman RJ, Rogers SJ, Rojas DC. A voxel-based morphometry comparison of regional gray matter between fragile X syndrome and autism. Psychiatry Res. 2009;174:138–45.
Duarte JV, Ribeiro MJ, Violante IR, Cunha G, Silva E, Castelo-Branco M. Multivariate pattern analysis reveals subtle brain anomalies relevant to the cognitive phenotype in neurofibromatosis type 1. Hum Brain Mapp. 2014;35:89–106.
Lee CH, Bartholomay KL, Marzelli MJ, Miller JG, Bruno JL, Lightbody AA, et al. Neuroanatomical profile of young females with Fragile X syndrome: a voxel-based morphometry analysis. Cereb Cortex. 2021;32:2310–20.
Barkovich MJ, Tan CH, Nillo RM, Li Y, Xu D, Glastonbury CM, et al. Abnormal morphology of select cortical and subcortical regions in neurofibromatosis type 1. Radiology. 2018;289:499–508.
Greenwood RS, Tupler LA, Whitt JK, Buu A, Dombeck CB, Harp AG, et al. Brain morphometry, T2-weighted hyperintensities, and IQ in children with neurofibromatosis type 1. Arch Neurol. 2005;62:1904–8.
Said SM, Yeh TL, Greenwood RS, Whitt JK, Tupler LA, Krishnan KR. MRI morphometric analysis and neuropsychological function in patients with neurofibromatosis. Neuroreport. 1996;7:1941–4.
Eliez S, Blasey CM, Freund LS, Hastie T, Reiss AL. Brain anatomy, gender and IQ in children and adolescents with fragile X syndrome. Brain. 2001;124:1610–8.
Hallahan BP, Craig MC, Toal F, Daly EM, Moore CJ, Ambikapathy A, et al. In vivo brain anatomy of adult males with Fragile X syndrome: an MRI study. Neuroimage. 2011;54:16–24.
Pride NA, Korgaonkar MS, Barton B, Payne JM, Vucic S, North KN. The genetic and neuroanatomical basis of social dysfunction: lessons from neurofibromatosis type 1. Hum Brain Mapp. 2014;35:2372–82.
Huijbregts S, Loitfelder M, Rombouts SA, Swaab H, Verbist BM, Arkink EB, et al. Cerebral volumetric abnormalities in neurofibromatosis type 1: associations with parent ratings of social and attention problems, executive dysfunction, and autistic mannerisms. J Neurodev Disord. 2015;7:32.
Parenti I, Rabaneda LG, Schoen H, Novarino G. Neurodevelopmental disorders: from genetics to functional pathways. Trends Neurosci. 2020;43:608–21.
Vorstman JAS, Spooren W, Persico AM, Collier DA, Aigner S, Jagasia R, et al. Using genetic findings in autism for the development of new pharmaceutical compounds. Psychopharmacol. 2014;231:1063–78.
Payne JM. Bridging the gap between mouse behavior and human cognition in neurofibromatosis type 1. EBioMedicine. 2015;2:1290–1.
Chisholm AK, Haebich KM, Pride NA, Walsh KS, Lami F, Ure A, et al. Delineating the autistic phenotype in children with neurofibromatosis type 1. Mol Autism. 2022;13:3.
Kaufmann WE, Kidd SA, Andrews HF, Budimirovic DB, Esler A, Haas-Givler B, et al. Autism spectrum disorder in fragile X syndrome: cooccurring conditions and current treatment. Pediatrics. 2017;139:S194–S206.
Mitchell RA, Barton SM, Harvey AS, Ure AM, Williams K. Factors associated with autism spectrum disorder in children with tuberous sclerosis complex: a systematic review and meta-analysis. Dev Med Child Neurol. 2021;63:791–801.
Ridler K, Bullmore ET, De Vries PJ, Suckling J, Barker GJ, Meara SJ, et al. Widespread anatomical abnormalities of grey and white matter structure in tuberous sclerosis. Psychol Med. 2001;31:1437–46.
Ridler K, Suckling J, Higgins NJ, de Vries PJ, Stephenson CM, Bolton PF, et al. Neuroanatomical correlates of memory deficits in tuberous sclerosis complex. Cereb Cortex. 2007;17:261–71.
Tye C, McEwen FS, Liang H, Underwood L, Woodhouse E, Barker ED, et al. Long-term cognitive outcomes in tuberous sclerosis complex. Dev Med Child Neurol. 2020;62:322–9.
Johnson EM, Ishak AD, Naylor PE, Stevenson DA, Reiss AL, Green T. PTPN11 gain-of-function mutations affect the developing human brain, memory, and attention. Cereb Cortex. 2019;29:2915–23.
Gauthier AS, Furstoss O, Araki T, Chan R, Neel BG, Kaplan DR, et al. Control of CNS cell-fate decisions by SHP-2 and its dysregulation in Noonan syndrome. Neuron. 2007;54:245–62.
Bartholomay KL, Lee CH, Bruno JL, Lightbody AA, Reiss AL. Closing the gender gap in fragile X syndrome: review on females with FXS and preliminary research findings. Brain Sci. 2019;9:11.
Anastasaki C, Orozco P, Gutmann DH. RAS and beyond: the many faces of the neurofibromatosis type 1 protein. Dis Model Mech. 2022;15:dmm049362.
Richter JD, Zhao X. The molecular biology of FMRP: new insights into fragile X syndrome. Nat Rev Neurosci. 2021;22:209–22.
Li W, Cui Y, Kushner SA, Brown RA, Jentsch JD, Frankland PW, et al. The HMG-CoA reductase inhibitor lovastatin reverses the learning and attention deficits in a mouse model of neurofibromatosis type 1. Curr Biol. 2005;15:1961–7.
Cui Y, Costa RM, Murphy GG, Elgersma Y, Zhu Y, Gutmann DH, et al. Neurofibromin regulation of ERK signaling modulates GABA release and learning. Cell. 2008;135:549–60.
Molosh AI, Johnson PL, Spence JP, Arendt D, Federici LM, Bernabe C, et al. Social learning and amygdala disruptions in Nf1 mice are rescued by blocking p21-activated kinase. Nat Neurosci. 2014;17:1583–90.
Scheffzek K, Ahmadian MR, Wiesmüller L, Kabsch W, Stege P, Schmitz F, et al. Structural analysis of the GAP-related domain from neurofibromin and its implications. Embo J. 1998;17:4313–27.
Guo HF, Tong J, Hannan F, Luo L, Zhong Y. A neurofibromatosis-1-regulated pathway is required for learning in Drosophila. Nature. 2000;403:895–8.
Anastasaki C, Woo AS, Messiaen LM, Gutmann DH. Elucidating the impact of neurofibromatosis-1 germline mutations on neurofibromin function and dopamine-based learning. Hum Mol Genet. 2015;24:3518–28.
Anastasaki C, Gutmann DH. Neuronal NF1/RAS regulation of cyclic AMP requires atypical PKC activation. Hum Mol Genet. 2014;23:6712–21.
Omrani A, van der Vaart T, Mientjes E, van Woerden GM, Hojjati MR, Li KW, et al. HCN channels are a novel therapeutic target for cognitive dysfunction in Neurofibromatosis type 1. Mol Psychiatry. 2015;20:1311–21.
Morris SM, Gutmann DH. A genotype-phenotype correlation for quantitative autistic trait burden in neurofibromatosis 1. Neurology. 2018;90:377–9.
Pigoni M, Uzquiano A, Paulsen B, Kedaigle AJ, Yang SM, Symvoulidis P, et al. Cell-type specific defects in PTEN-mutant cortical organoids converge on abnormal circuit activity. Hum Mol Genet. 2023;32:2773–86.
Li Y, Zhao X. Concise review: fragile X proteins in stem cell maintenance and differentiation. Stem Cells. 2014;32:1724–33.
Wang Y, Kim E, Wang X, Novitch BG, Yoshikawa K, Chang LS, et al. ERK inhibition rescues defects in fate specification of Nf1-deficient neural Ppogenitors and brain abnormalities. Cell. 2012;150:816–30.
Andrews MG, Subramanian L, Kriegstein AR. mTOR signaling regulates the morphology and migration of outer radial glia in developing human cortex. eLife. 2020;9:e58737.
Richter JD, Bassell GJ, Klann E. Dysregulation and restoration of translational homeostasis in fragile X syndrome. Nat Rev Neurosci. 2015;16:595–605.
Dasgupta B. Gutmann DH. Neurofibromin regulates neural stem cell proliferation, survival, and astroglial differentiation in vitro and in vivo. J Neurosci. 2005;25:5584–94.
Cheng Y, Corbin JG, Levy RJ. Programmed cell death is impaired in the developing brain of FMR1 mutants. Dev Neurosci. 2013;35:347–58.
Bockaert J, Marin P. mTOR in brain physiology and pathologies. Physiol Rev. 2015;95:1157–87.
Kosodo Y, Huttner WB. Basal process and cell divisions of neural progenitors in the developing brain. Dev Growth Differ. 2009;51:251–61.
Lafourcade CA, Lin TV, Feliciano DM, Zhang L, Hsieh LS, Bordey A. Rheb activation in subventricular zone progenitors leads to heterotopia, ectopic neuronal differentiation, and rapamycin-sensitive olfactory micronodules and dendrite hypertrophy of newborn neurons. J Neurosci. 2013;33:2419–31.
Pride N, Payne JM, Webster R, Shores EA, Rae C, North KN. Corpus callosum morphology and its relationship to cognitive function in neurofibromatosis type 1. J Child Neurol. 2010;25:834–41.
Nie D, Di Nardo A, Han JM, Baharanyi H, Kramvis I, Huynh T, et al. Tsc2-Rheb signaling regulates EphA-mediated axon guidance. Nat Neurosci. 2010;13:163–72.
Piper M, Lee AC, van Horck FP, McNeilly H, Lu TB, Harris WA, et al. Differential requirement of F-actin and microtubule cytoskeleton in cue-induced local protein synthesis in axonal growth cones. Neural Dev. 2015;10:3.
Choi YJ, Di Nardo A, Kramvis I, Meikle L, Kwiatkowski DJ, Sahin M, et al. Tuberous sclerosis complex proteins control axon formation. Genes Dev. 2008;22:2485–95.
Kumar V, Zhang MZ, Swank MW, Kunz J, Wu GY. Regulation of dendritic morphogenesis by Ras–PI3K–Akt–mTOR and Ras–MAPK signaling pathways. J Neurosci. 2005;25:11288.
Eichmüller OL, Corsini NS, Vértesy Á, Morassut I, Scholl T, Gruber VE, et al. Amplification of human interneuron progenitors promotes brain tumors and neurological defects. Science. 2022;375:eabf5546.
He Z, Maynard A, Jain A, Gerber T, Petri R, Lin HC, et al. Lineage recording in human cerebral organoids. Nat Methods. 2022;19:90–9.
Blair JD, Hockemeyer D, Bateup HS. Genetically engineered human cortical spheroid models of tuberous sclerosis. Nature Med. 2018;24:1568–78.
Paulsen B, Velasco S, Kedaigle AJ, Pigoni M, Quadrato G, Deo A, et al. Autist genes converge on asynchronous development of shared neuron clases. Nature. 2022;602:268–73.
Villa CE, Cheroni C, Dotter CP, López-Tóbon A, Oliveira B, Sacco R, et al. CHD8 haploinsufficiency links autism to transient alterations in excitatory and inhibitory trajectories. Cell Rep. 2022;39:110615.
Urresti J, Zhang P, Moran-Losada P, Yu NK, Negraes PD, Trujillo CA, et al. Cortical organoids model early brain development disrupted by 16p11.2 copy number variants in autism. Mol Psychiatry. 2021;26:7560–80.
Zhang W, Ma L, Yang M, Shao Q, Xu J, Lu Z, et al. Cerebral organoid and mouse models reveal a RAB39b-PI3K-mTOR pathway-dependent dysregulation of cortical development leading to macrocephaly/autism phenotypes. Genes Dev. 2020;34:580–97.
Dang LT, Vaid S, Lin G, Swaminathan P, Safran J, Loughman A, et al. STRADA-mutant human cortical organoids model megalencephaly and exhibit delayed neuronal differentiation. Dev Neurobiol. 2021;81:696–709.
Li Y, Muffat J, Omer A, Bosch I, Lancaster MA, Sur M, et al. Induction of expansion and folding in human cerebral organoids. Cell Stem Cell. 2017;20:385–96.e3.
Hagerman RJ, Berry-Kravis E, Hazlett HC, Bailey DB, Moine H, Kooy RF, et al. Fragile X syndrome. Nat Rev Dis Primers. 2017;3:17065.
Cornish K, Cole V, Longhi E, Karmiloff-Smith A, Scerif G. Mapping developmental trajectories of attention and working memory in fragile X syndrome: developmental freeze or developmental change? Dev Psychopathol. 2013;25:365–76.
Summers MA, Quinlan KG, Payne JM, Little DG, North KN, Schindeler A. Skeletal muscle and motor deficits in Neurofibromatosis Type 1. J Musculoskelet Neuronal Interact. 2015;15:161–70.
Hyman SL, Shores EA, North KN. The nature and frequency of cognitive deficits in children with neurofibromatosis type 1. Neurology. 2005;65:1037–44.
Mautner VF, Kluwe L, Thakker SD, Leark RA. Treatment of ADHD in neurofibromatosis type 1. Dev Med Child Neurol. 2002;44:164–70.
Payne JM, Hyman SL, Shores EA, North KN. Assessment of executive function and attention in children with neurofibromatosis type 1: relationships between cognitive measures and real-world behavior. Child Neuropsychol. 2011;17:313–29.
Garg S, Green J, Leadbitter K, Emsley R, Lehtonen A, Evans DG, et al. Neurofibromatosis type 1 and autism spectrum disorder. Pediatrics. 2013;132:e1642–e8.
Green T, Naylor PE, Davies W. Attention deficit hyperactivity disorder (ADHD) in phenotypically similar neurogenetic conditions: Turner syndrome and the RASopathies. J Neurodev Disord. 2017;9:25.
Ciaccio C, Saletti V, D’Arrigo S, Esposito S, Alfei E, Moroni I, et al. Clinical spectrum of PTEN mutation in pediatric patients. A bicenter experience. Eur J Med Genet. 2019;62:103596.
Joinson C, O’Callaghan FJ, Osborne JP, Martyn C, Harris T, Bolton PF. Learning disability and epilepsy in an epidemiological sample of individuals with tuberous sclerosis complex. Psychol Med. 2003;33:335–44.
Henske EP, Jóźwiak S, Kingswood JC, Sampson JR, Thiele EA. Tuberous sclerosis complex. Nat Rev Dis Primers. 2016;2:16035.
Numis AL, Major P, Montenegro MA, Muzykewicz DA, Pulsifer MB, Thiele EA. Identification of risk factors for autism spectrum disorders in tuberous sclerosis complex. Neurology. 2011;76:981–7.
Cohen JD, Nichols T, Brignone L, Hall SS, Reiss AL. Insular volume reduction in fragile X syndrome. Int J Dev Neurosci. 2011;29:489–94.
Gothelf D, Furfaro JA, Hoeft F, Eckert MA, Hall SS, O’Hara R, et al. Neuroanatomy of fragile X syndrome is associated with aberrant behavior and the fragile X mental retardation protein (FMRP). Ann Neurol. 2008;63:40–51.
Lee AD, Leow AD, Lu A, Reiss AL, Hall S, Chiang MC, et al. 3D pattern of brain abnormalities in Fragile X syndrome visualized using tensor-based morphometry. Neuroimage. 2007;34:924–38.
Baudou E, Nemmi F, Biotteau M, Maziero S, Assaiante C, Cignetti F, et al. Are morphological and structural MRI characteristics related to specific cognitive impairments in neurofibromatosis type 1 (NF1) children? Eur J Paediatr Neurol. 2020;28:89–100.
Karlsgodt KH, Rosser T, Lutkenhoff ES, Cannon TD, Silva A, Bearden CE. Alterations in white matter microstructure in neurofibromatosis-1. PLoS ONE. 2012;7:e47854.
Moore BD 3rd, Slopis JM, Jackson EF, De Winter AE, Leeds NE. Brain volume in children with neurofibromatosis type 1: relation to neuropsychological status. Neurology. 2000;54:914–20.
Violante IR, Ribeiro MJ, Silva ED, Castelo-Branco M. Gyrification, cortical and subcortical morphometry in neurofibromatosis type 1: An uneven profile of developmental abnormalities. J Neurodev Disord. 2013;5:3.
Acknowledgements
JMP is funded by a Murdoch Children’s Research Institute Clinician-Scientist Fellowship. DRH is supported by a Discovery Early Career Researcher Award (DE160100042). SV is supported by the Novo Nordisk Foundation Center for Stem Cell Medicine (reNEW), funded by the Novo Nordisk Foundation grant NNF21CC0073719. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
JMP and KMH had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the analysis. All authors approved the final version before submission. Study concept and design: JMP, DRH. Acquisition, of data: JMP, EG, KMH, RM, AM. Interpretation of data: JMP, KMH, RM, KB, EG, PJL, AM, SV, GB, KNN, DRH. Drafting of manuscript: JMP, EG. Critical revision of the manuscript for important intellectual content: KMH, RM, KB, PJL, AM, SV, GB, KNN, DRH. Statistical analysis: KMH, EG. Study supervision: JMP, DRH. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Payne, J.M., Haebich, K.M., Mitchell, R. et al. Brain volumes in genetic syndromes associated with mTOR dysregulation: a systematic review and meta-analysis. Mol Psychiatry 30, 1676–1688 (2025). https://doi.org/10.1038/s41380-024-02863-4
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41380-024-02863-4
This article is cited by
-
Academic Achievement of Children and Adolescents with Neurofibromatosis Type 1: A Systematic Review and Meta-Analysis
Neuropsychology Review (2025)