Abstract
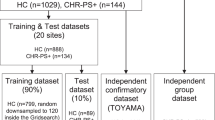
Deficits in mediodorsal thalamus-dorsolateral prefrontal cortex (MDT-DLPFC) resting-state functional magnetic resonance imaging (rs-fMRI) connectivity and prefrontal sleep spindles have been reported in chronic and early course schizophrenia. However, the presence of these alterations in clinical high-risk for psychosis (CHR), alongside their relationships with underlying neurotransmission and cognitive function, remains to be established. Thirty-one CHR and thirty-two HC underwent: 1) 7 T rs-fMRI; 2) 7 T magnetic resonance spectroscopy imaging (MRSI); and 3) sleep electroencephalography (EEG). Rs-fMRI connectivity was analyzed by seeding the whole thalamus (WT) and seven thalamic subsections. Spindle duration was computed across all EEG channels. GABA/creatine (Cr) and glutamate/Cr were calculated in DLPFC and MDT. Relative to HC, CHR showed WT-DLPFC hypoconnectivity (p-FDR = 0.001), especially involving MDT-DLPFC (p-FDR < 0.001) and reduced prefrontal spindle duration (t-stat = −2.64, p = 0.010), while no differences were found for MRSI neuro-metabolites. We then performed clustering analysis using rs-fMRI connectivity and spindle duration to identify CHR and HC subgroups and predict their working memory (WM) performance. A cluster with intact rs-fMRI and spindle duration included mostly HC (83.33% purity), while a cluster with both measures altered involved almost entirely CHR (91.66% purity) and showed worse WM performances. We also examined MRSI metabolites’ contribution to spindles and rs-fMRI connectivity with a within-group multivariable regression analysis. In HC, but not in CHR, MDT glutamate/Cr negatively predicted spindle duration and positively predicted MDT-DLPFC connectivity. Combined, these findings indicate that a multimodal neuroimaging approach can identify distinct thalamocortical dysfunctions in CHR individuals, thus informing future research aimed at developing personalized interventions in these individuals.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The data supporting the findings of this study are included in the main article and its supplementary materials. Additional details will be provided upon request by contacting the corresponding author.
References
Ferrarelli F, Tononi G. Reduced sleep spindle activity point to a TRN-MD thalamus-PFC circuit dysfunction in schizophrenia. Schizophr Res. 2017;180:36–43.
Danos P, Schmidt A, Baumann B, Bernstein H-G, Northoff G, Stauch R, et al. Volume and neuron number of the mediodorsal thalamic nucleus in schizophrenia: a replication study. Psychiatry Res. 2005;140:281–9.
Byne W, Buchsbaum MS, Mattiace LA, Hazlett EA, Kemether E, Elhakem SL, et al. Postmortem assessment of thalamic nuclear volumes in subjects with schizophrenia. Am J Psychiatry. 2002;159:59–65.
Woodward ND, Heckers S. Mapping thalamocortical functional connectivity in chronic and early stages of psychotic disorders. Biol Psychiatry. 2016;79:1016–25.
Woodward ND, Karbasforoushan H, Heckers S. Thalamocortical dysconnectivity in schizophrenia. Am J Psychiatry. 2012;169:1092–9.
Anticevic A, Cole MW, Repovs G, Murray JD, Brumbaugh MS, Winkler AM, et al. Characterizing thalamo-cortical disturbances in schizophrenia and bipolar illness. Cereb Cortex. 2014;24:3116–30.
Marenco S, Stein JL, Savostyanova AA, Sambataro F, Tan H-Y, Goldman AL, et al. Investigation of anatomical thalamo-cortical connectivity and FMRI activation in schizophrenia. Neuropsychopharmacology. 2012;37:499–507.
Uhlhaas PJ, Roux F, Singer W. Thalamocortical synchronization and cognition: implications for schizophrenia? Neuron. 2013;77:997–9.
Eryilmaz H, Tanner AS, Ho NF, Nitenson AZ, Silverstein NJ, Petruzzi LJ, et al. Disrupted working memory circuitry in schizophrenia: disentangling fMRI markers of core pathology vs other aspects of impaired performance. Neuropsychopharmacology. 2016;41:2411–20.
Fernandez LM, Lüthi A. Sleep spindles: mechanisms and functions. Physiol Rev. 2020;100:805–68.
Kozhemiako N, Wang J, Jiang C, Wang LA, Gai G, Zou K, et al. Non-rapid eye movement sleep and wake neurophysiology in schizophrenia. Elife. 2022;11:e76211.
Ferrarelli F, Huber R, Peterson MJ, Massimini M, Murphy M, Riedner BA, et al. Reduced sleep spindle activity in schizophrenia patients. Am J Psychiatry. 2007;164:483–92.
Ferrarelli F, Peterson MJ, Sarasso S, Riedner BA, Murphy MJ, Benca RM, et al. Thalamic dysfunction in schizophrenia suggested by whole-night deficits in slow and fast spindles. Am J Psychiatry. 2010;167:1339–48.
Bagautdinova J, Mayeli A, Wilson JD, Donati FL, Colacot RM, Meyer N, et al. Sleep abnormalities in different clinical stages of psychosis: a systematic review and meta-analysis. JAMA Psychiatry. 2023;80:202–10.
Manoach DS, Demanuele C, Wamsley EJ, Vangel M, Montrose DM, Miewald J, et al. Sleep spindle deficits in antipsychotic-naïve early course schizophrenia and in non-psychotic first-degree relatives. Front Hum Neurosci. 2014;8:762.
Buchmann A, Dentico D, Peterson MJ, Riedner BA, Sarasso S, Massimini M, et al. Reduced mediodorsal thalamic volume and prefrontal cortical spindle activity in schizophrenia. Neuroimage. 2014;102:540–7.
McCormick DA. Neurotransmitter actions in the thalamus and cerebral cortex. J Clin Neurophysiol. 1992;9:212–23.
Sanchez-Vives MV, Barbero-Castillo A, Perez-Zabalza M, Reig R. GABAB receptors: modulation of thalamocortical dynamics and synaptic plasticity. Neuroscience. 2021;456:131–42.
Just N, Sonnay S. Investigating the role of glutamate and GABA in the modulation of transthalamic activity: a combined fMRI-fMRS study. Front Physiol. 2017;8:30.
Bartho P, Slezia A, Matyas F, Faradzs-Zade L, Ulbert I, Harris KD, et al. Ongoing network state controls the length of sleep spindles via inhibitory activity. Neuron. 2014;82:1367–79.
Krosigk von M, Bal T, McCormick DA. Cellular mechanisms of a synchronized oscillation in the thalamus. Science. 1993;261:361–4.
Lustenberger C, O’Gorman RL, Pugin F, Tüshaus L, Wehrle F, Achermann P, et al. Sleep spindles are related to schizotypal personality traits and thalamic glutamine/glutamate in healthy subjects. Schizophr Bull. 2015;41:522–31.
Kiemes A, Davies C, Kempton MJ, Lukow PB, Bennallick C, Stone JM, et al. GABA, glutamate and neural activity: a systematic review with meta-analysis of multimodal 1H-MRS-fMRI studies. Front Psychiatry. 2021;12:644315.
Kraguljac NV, White DM, Reid MA, Lahti AC. Increased hippocampal glutamate and volumetric deficits in unmedicated patients with schizophrenia. JAMA Psychiatry. 2013;70:1294–302.
Kim S-Y, Kaufman MJ, Cohen BM, Jensen JE, Coyle JT, Du F, et al. In vivo brain glycine and glutamate concentrations in patients with first-episode psychosis measured by echo time–averaged proton magnetic resonance spectroscopy at 4T. Biol Psychiatry. 2018;83:484–91.
Birur B, Kraguljac NV, Shelton RC, Lahti AC. Brain structure, function, and neurochemistry in schizophrenia and bipolar disorder—a systematic review of the magnetic resonance neuroimaging literature. NPJ Schizophr. 2017;3:15.
Merritt K, McGuire PK, Egerton A, Aleman A, Block W, Bloemen OJ, et al. Association of age, antipsychotic medication, and symptom severity in schizophrenia with proton magnetic resonance spectroscopy brain glutamate level: a mega-analysis of individual participant-level data. JAMA psychiatry. 2021;78:667–81.
Iwata Y, Nakajima S, Plitman E, Caravaggio F, Kim J, Shah P, et al. Glutamatergic neurometabolite levels in patients with ultra-treatment-resistant schizophrenia: a cross-sectional 3T proton magnetic resonance spectroscopy study. Biol Psychiatry. 2019;85:596–605.
Kaminski J, Gleich T, Fukuda Y, Katthagen T, Gallinat J, Heinz A, et al. Association of cortical glutamate and working memory activation in patients with schizophrenia: a multimodal proton magnetic resonance spectroscopy and functional magnetic resonance imaging study. Biol Psychiatry. 2020;87:225–33.
Kumar V, Vajawat B, Rao NP. Frontal GABA in schizophrenia: A meta-analysis of 1H-MRS studies. World J Biol Psychiatry. 2021;22:1–13.
Kegeles LS, Mao X, Stanford AD, Girgis R, Ojeil N, Xu X, et al. Elevated prefrontal cortex γ-aminobutyric acid and glutamate-glutamine levels in schizophrenia measured in vivo with proton magnetic resonance spectroscopy. Arch Gen Psychiatry. 2012;69:449–59.
Mayeli A, Sonnenschein SF, Yushmanov VE, Wilson JD, Blazer A, Foran W, et al. Dorsolateral prefrontal cortex glutamate/gamma-aminobutyric acid (GABA) alterations in clinical high risk and first-episode schizophrenia: a preliminary 7-T magnetic resonance spectroscopy imaging study. Int J Mol Sci. 2022;23:15846.
Quiñones GM, Mayeli A, Yushmanov VE, Hetherington HP, Ferrarelli F. Reduced GABA/glutamate in the thalamus of individuals at clinical high risk for psychosis. Neuropsychopharmacology. 2021;46:1133–9.
Fusar-Poli P. The clinical high-risk state for psychosis (CHR-P), version II. Schizophr Bull. 2017;43:44–47.
Nelson B, Yuen HP, Wood SJ, Lin A, Spiliotacopoulos D, Bruxner A, et al. Long-term follow-up of a group at ultra high risk (“prodromal”) for psychosis: the PACE 400 study. JAMA Psychiatry. 2013;70:793–802.
Fusar-Poli P, Bechdolf A, Taylor MJ, Bonoldi I, Carpenter WT, Yung AR, et al. At risk for schizophrenic or affective psychoses? A meta-analysis of DSM/ICD diagnostic outcomes in individuals at high clinical risk. Schizophr Bull. 2013;39:923–32.
Cannon TD. The current state of the clinical high risk for psychosis research paradigm. Biol Psychiatry. 2020;88:284–6.
Anticevic A, Haut K, Murray JD, Repovs G, Yang GJ, Diehl C, et al. Association of thalamic dysconnectivity and conversion to psychosis in youth and young adults at elevated clinical risk. JAMA Psychiatry. 2015;72:882–91.
Mayeli A, Wilson JD, Donati FL, LaGoy AD, Ferrarelli F. Sleep spindle alterations relate to working memory deficits in individuals at clinical high-risk for psychosis. Sleep. 2022;45:zsac193.
Miller TJ, McGlashan TH, Rosen JL, Cadenhead K, Ventura J, McFarlane W, et al. Prodromal assessment with the structured interview for prodromal syndromes and the scale of prodromal symptoms: predictive validity, interrater reliability, and training to reliability. Schizophr Bull. 2003;29:703–15.
Whitfield-Gabrieli S, Nieto-Castanon A. Conn: a functional connectivity toolbox for correlated and anticorrelated brain networks. Brain Connect. 2012;2:125–41.
https://www.nitrc.org/projects/wfu_pickatlas/, Date Accessed, 2023.
Najdenovska E, Alemán-Gómez Y, Battistella G, Descoteaux M, Hagmann P, Jacquemont S, et al. In-vivo probabilistic atlas of human thalamic nuclei based on diffusion-weighted magnetic resonance imaging. Sci Data. 2018;5:1–11.
Baran B, Karahanoğlu FI, Mylonas D, Demanuele C, Vangel M, Stickgold R, et al. Increased thalamocortical connectivity in schizophrenia correlates with sleep spindle deficits: evidence for a common pathophysiology. Biol Psychiatry Cogn Neurosci Neuroimaging. 2019;4:706–14.
Silber MH, Ancoli-Israel S, Bonnet MH, Chokroverty S, Grigg-Damberger MM, Hirshkowitz M, et al. The visual scoring of sleep in adults. J Clin Sleep Med. 2007;3:121–31.
Fraley C, Raftery AE. Model-based clustering, discriminant analysis, and density estimation. J Am Stat Assoc. 2002;97:611–31.
Nuechterlein KH, Green MF, Kern RS, Baade LE, Barch DM, Cohen JD, et al. The MATRICS consensus cognitive battery, part 1: test selection, reliability, and validity. Am J Psychiatry. 2008;165:203–13.
Younis S, Hougaard A, Christensen CE, Vestergaard MB, Petersen ET, Boer VO, et al. Feasibility of glutamate and GABA detection in pons and thalamus at 3T and 7T by proton magnetic resonance spectroscopy. Front Neurosci. 2020;14:559314.
Pradhan S, Bonekamp S, Gillen JS, Rowland LM, Wijtenburg SA, Edden RA, et al. Comparison of single voxel brain MRS AT 3 T and 7 T using 32-channel head coils. Magn Reson Imaging. 2015;33:1013–8.
Pan JW, Avdievich N, Hetherington HP. J-refocused coherence transfer spectroscopic imaging at 7 T in human brain. Magn Reson Med. 2010;64:1237–46.
Lacadie CM, Fulbright RK, Rajeevan N, Constable RT, Papademetris X. More accurate talairach coordinates for neuroimaging using non-linear registration. Neuroimage. 2008;42:717–25.
Provencher SW. Automatic quantitation of localized in vivo 1H spectra with LCModel. NMR Biomed. 2001;14:260–4.
Lloyd S. Least squares quantization in PCM. IEEE Trans Inf Theory. 1982;28:129–37.
Kodinariya TM, Makwana PR. Review on determining number of cluster in K-means clustering. Int J. 2013;1:90–95.
Zhang ZY, Campbell IG, Dhayagude P, Espino HC, Feinberg I. Longitudinal analysis of sleep spindle maturation from childhood through late adolescence. J Neurosci. 2021;41:4253–61.
Purcell S, Manoach D, Demanuele C, Cade B, Mariani S, Cox R, et al. Characterizing sleep spindles in 11,630 individuals from the national sleep research resource. Nat Commun. 2017;8:15930.
Goldman‐Rakic PS, Porrino LJ. The primate mediodorsal (MD) nucleus and its projection to the frontal lobe. J Comp Neurol. 1985;242:535–60.
Ha M, Park SH, Park I, Kim T, Lee J, Kim M, et al. Aberrant cortico-thalamo-cerebellar network interactions and their association with impaired cognitive functioning in patients with schizophrenia. Schizophrenia. 2023;9:50.
Messina A, Cuccì G, Crescimanno C, Signorelli MS. Clinical anatomy of the precuneus and pathogenesis of the schizophrenia. Anat Sci Int. 2023;98:473–81.
Lai M, Hegde R, Kelly S, Bannai D, Lizano P, Stickgold R, et al. Investigating sleep spindle density and schizophrenia: a meta-analysis. Psychiatry Res. 2022;307:114265.
Ruhrmann S, Schultze-Lutter F, Salokangas RK, Heinimaa M, Linszen D, Dingemans P, et al. Prediction of psychosis in adolescents and young adults at high risk: results from the prospective European prediction of psychosis study. Arch Gen Psychiatry. 2010;67:241–51.
Zaks N, Velikonja T, Parvaz MA, Zinberg J, Done M, Mathalon DH, et al. Sleep disturbance in individuals at clinical high risk for psychosis. Schizophr Bull. 2022;48:111–21.
Donati FL, D’Agostino A, Ferrarelli F. Neurocognitive and neurophysiological endophenotypes in schizophrenia: an overview. Biomark Neuropsychiatry. 2020;3:100017.
Manoach DS, Stickgold R. Abnormal sleep spindles, memory consolidation, and schizophrenia. Annu Rev Clin Psychol. 2019;15:451–79.
Schreiner T, Kaufmann E, Noachtar S, Mehrkens J-H, Staudigl T. The human thalamus orchestrates neocortical oscillations during NREM sleep. Nat Commun. 2022;13:5231.
Lesh TA, Niendam TA, Minzenberg MJ, Carter CS. Cognitive control deficits in schizophrenia: mechanisms and meaning. Neuropsychopharmacology. 2011;36:316–38.
Reichenberg A. The assessment of neuropsychological functioning in schizophrenia. Dialogues Clin Neurosci. 2010;12:383–92.
Catalan A, de Pablo GS, Aymerich C, Damiani S, Sordi V, Radua J, et al. Neurocognitive functioning in individuals at clinical high risk for psychosis: a systematic review and meta-analysis. JAMA Psychiatry. 2021;78:859–67.
Lewis DA. Inhibitory neurons in human cortical circuits: substrate for cognitive dysfunction in schizophrenia. Curr Opin Neurobiol. 2014;26:22–26.
Hoftman GD, Dienel SJ, Bazmi HH, Zhang Y, Chen K, Lewis DA. Altered gradients of glutamate and gamma-aminobutyric acid transcripts in the cortical visuospatial working memory network in schizophrenia. Biol Psychiatry. 2018;83:670–9.
Baldwin H, Radua J, Antoniades M, Haas SS, Frangou S, Agartz I, et al. Neuroanatomical heterogeneity and homogeneity in individuals at clinical high risk for psychosis. Transl Psychiatry. 2022;12:297.
Fusar-Poli P, Cappucciati M, Borgwardt S, Woods SW, Addington J, Nelson B, et al. Heterogeneity of psychosis risk within individuals at clinical high risk: a meta-analytical stratification. JAMA Psychiatry. 2016;73:113–20.
Carney R, Cotter J, Firth J, Bradshaw T, Yung AR. Cannabis use and symptom severity in individuals at ultra high risk for psychosis: a meta‐analysis. Acta Psychiatr Scand. 2017;136:5–15.
Gates PJ, Albertella L, Copeland J. The effects of cannabinoid administration on sleep: a systematic review of human studies. Sleep Med Rev. 2014;18:477–87.
Kesner AJ, Lovinger DM. Cannabinoids, endocannabinoids and sleep. Front Mol Neurosci. 2020;13:125.
Garcia AN, Salloum IM. Polysomnographic sleep disturbances in nicotine, caffeine, alcohol, cocaine, opioid, and cannabis use: a focused review. Am J Addict. 2015;24:590–8.
Tassinari C, Ambrosetto G, Peraita-Adrado M, Gastaut H. The neuropsychiatric syndrome of Δ9-tetrahydrocannabinol and cannabis intoxication in naïve subjects: a clinical and polygraphic study during wakefulness and sleep. Marihuana and Medicine. New York: Raven Press; 1999, pp 649–64.
Mondino A, Cavelli M, González J, Santana N, Castro-Zaballa S, Mechoso B, et al. Acute effect of vaporized cannabis on sleep and electrocortical activity. Pharmacol Biochem Behav. 2019;179:113–23.
Samanta A, Aleman-Zapata A, Agarwal K, Özsezer P, Alonso A, van der Meij J, et al. CBD lengthens sleep but shortens ripples and leads to intact simple but worse cumulative memory. Iscience. 2023;26:108327.
Lavender I, McCartney D, Marshall N, Suraev A, Irwin C, D’Rozario AL, et al. Cannabinol (CBN; 30 and 300 mg) effects on sleep and next-day function in insomnia disorder (‘CUPID’study): protocol for a randomised, double-blind, placebo-controlled, cross-over, three-arm, proof-of-concept trial. BMJ Open. 2023;13:e071148.
Thomson AR, Hwa H, Pasanta D, Hopwood B, Powell HJ, Lawrence R, et al. The developmental trajectory of 1H-MRS brain metabolites from childhood to adulthood. Cereb Cortex. 2024;34:bhae046.
Perica MI, Calabro FJ, Larsen B, Foran W, Yushmanov VE, Hetherington H, et al. Development of frontal GABA and glutamate supports excitation/inhibition balance from adolescence into adulthood. Prog Neurobiol. 2022;219:102370.
Fair D, Bathula D, Mills KL, Costa Dias TG, Blythe MS, Zhang D, et al. Maturing thalamocortical functional connectivity across development. Front Syst Neurosci. 2010;4:1422.
Abitz M, Nielsen RD, Jones EG, Laursen H, Graem N, Pakkenberg B. Excess of neurons in the human newborn mediodorsal thalamus compared with that of the adult. Cereb Cortex. 2007;17:2573–8.
Nguyen TT, Eyler LT, Jeste DV. Systemic biomarkers of accelerated aging in schizophrenia: a critical review and future directions. Schizophr Bull. 2018;44:398–408.
Baliga SP, Mehta UM. A review of studies leveraging multimodal TMS-fMRI applications in the pathophysiology and treatment of schizophrenia. Front Hum Neurosci. 2021;15:662976.
Fröhlich F, Lustenberger C. Neuromodulation of sleep rhythms in schizophrenia: towards the rational design of non-invasive brain stimulation. Schizophr Res. 2020;221:71–80.
Acknowledgements
This work was supported by the NIMH R01MH113827 BRAINS award. We would also like to thank all the individuals who participated in the study.
Author information
Authors and Affiliations
Contributions
AK, FD, AM, and FF helped with conceptualization, data curation, visualization, methodology and data analysis, investigation, validation, project administration, writing – review and editing. SJ and CH helped with running experiments, data curation and writing – review and editing. CM, HH helped with conceptualization, methodology and writing – review and editing. JW helped with methodology, conceptualization and writing – review and editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Keihani, A., Donati, F.L., Janssen, S.A. et al. Multimodal evidence of mediodorsal thalamus-prefrontal circuit dysfunctions in clinical high-risk for psychosis: findings from a combined 7T fMRI, MRSI and sleep Hd-EEG study. Mol Psychiatry 30, 3384–3392 (2025). https://doi.org/10.1038/s41380-025-02924-2
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41380-025-02924-2