Abstract
Non-suicidal self-injury (NSSI) refers to intentional self-inflicted bodily harm without suicidal intent. NSSI has been linked to various neurobiological dysfunctions, but its precise neural mechanisms have not been fully elucidated. Clinically, conventional pharmacological and psychotherapeutic interventions often exhibit prolonged treatment durations, delayed onset of efficacy, and considerable side effects, limiting their ability to effectively target the core pathological mechanisms of NSSI. These limitations highlight the urgent need for novel therapeutic approaches. Neuromodulation techniques, which have the potential to directly modulate neural activity, have recently been explored as promising interventions for NSSI. However, research in this field remains in its early stages. Existing evidence is limited and heterogeneous, with substantial interindividual variability in treatment response and a lack of high-quality, systematic clinical data. This review synthesizes findings from recent neuroimaging studies to examine the neural circuits potentially involved in NSSI from four key domains: emotion regulation, reward feedback, pain processing, and impulse control. By elucidating the underlying neurobiological mechanisms, summarizing current evidence on neuromodulation, and exploring future directions for therapeutic innovation and optimization, this review aims to provide a foundation for advancing neuromodulation-based treatments for NSSI.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
American Psychiatric Association D. Diagnostic and statistical manual of mental disorders: DSM-5. Washington, DC: American psychiatric association; 2013.
Swannell SV, Martin GE, Page A, Hasking P, St John NJ. Prevalence of nonsuicidal self-injury in nonclinical samples: systematic review, meta-analysis and meta-regression. Suicide Life Threat Behav. 2014;44:273–303.
Moran P, Chandler A, Dudgeon P, Kirtley OJ, Knipe D, Pirkis J, et al. The lancet commission on self-harm. Lancet. 2024;404:1445–92.
Brager-Larsen A, Zeiner P, Klungsøyr O, Mehlum L. Is age of self-harm onset associated with increased frequency of non-suicidal self-injury and suicide attempts in adolescent outpatients? BMC Psychiatry. 2022;22:58.
Muehlenkamp JJ, Claes L, Havertape L, Plener PL. International prevalence of adolescent non-suicidal self-injury and deliberate self-harm. Child Adolesc Psychiatry Ment Health. 2012;6:10.
Denton EG, Álvarez K. The global prevalence of nonsuicidal self-injury among adolescents. JAMA Netw Open. 2024;7:e2415406.
Lowry NJ, Ryan PC, Mournet AM, Snyder DJ, Claassen C, Jobes D, et al. Non-suicidal self-injury and suicide risk among adult medical inpatients. J Affect Disord Rep. 2023;11:100474.
Eggart V, Cordier S, Hasan A, Wagner E. Psychotropic drugs for the treatment of non-suicidal self-injury in children and adolescents: a systematic review and meta-analysis. Eur Arch Psychiatry Clin Neurosci. 2022;272:1559–68.
Karakuła-Juchnowicz H, Banaszek A, Juchnowicz D. Use of the opioid receptor antagonist - naltrexone in the treatment of non-suicidal self-injury. Psychiatr Pol. 2024;58:605–18.
Cook NE, Gorraiz M. Dialectical behavior therapy for nonsuicidal self‐injury and depression among adolescents: preliminary meta‐analytic evidence. Child Adolesc Ment Health. 2016;21:81–9.
Hawton K, Witt KG, Taylor Salisbury TL, Arensman E, Gunnell D, Hazell P, et al. Psychosocial interventions for self-harm in adults. Cochrane Database Syst Rev. 2016;2016:Cd012189.
Turner BJ, Austin SB, Chapman AL. Treating nonsuicidal self-injury: a systematic review of psychological and pharmacological interventions. Can J Psychiatry. 2014;59:576–85.
Auerbach RP, Pagliaccio D, Allison GO, Alqueza KL, Alonso MF. Neural correlates associated with suicide and nonsuicidal self-injury in youth. Biol Psychiatry. 2021;89:119–33.
Koenig J, Höper S, van der Venne P, Mürner-Lavanchy I, Resch F, Kaess M. Resting state prefrontal cortex oxygenation in adolescent non-suicidal self-injury - a near-infrared spectroscopy study. Neuroimage Clin. 2021;31:102704.
Höper S, Kröller F, Heinze AL, Bardtke KF, Kaess M, Koenig J. Prefrontal cortex activation under stress as a function of borderline personality disorder in female adolescents engaging in non-suicidal self-injury. BJPsych Open. 2024;10:e142.
Westlund Schreiner M, Klimes-Dougan B, Mueller BA, Eberly LE, Reigstad KM, Carstedt PA, et al. Multi-modal neuroimaging of adolescents with non-suicidal self-injury: amygdala functional connectivity. J Affect Disord. 2017;221:47–55.
Wang K, He Q, Zhu X, Hu Y, Yao Y, Hommel B, et al. Smaller putamen volumes are associated with greater problems in external emotional regulation in depressed adolescents with nonsuicidal self-injury. J Psychiatr Res. 2022;155:338–46.
Osuch E, Ford K, Wrath A, Bartha R, Neufeld R. Functional MRI of pain application in youth who engaged in repetitive non-suicidal self-injury vs. psychiatric controls. Psychiatry Res. 2014;223:104–12.
Chen X, Chen H, Liu J, Tang H, Zhou J, Liu P, et al. Functional connectivity alterations in reward-related circuits associated with non-suicidal self-injury behaviors in drug-naive adolescents with depression. J Psychiatr Res. 2023;163:270–7.
Vega D, Ripolles P, Soto A, Torrubia R, Ribas J, Monreal JA, et al. Orbitofrontal overactivation in reward processing in borderline personality disorder: the role of non-suicidal self-injury. Brain Imaging Behav. 2018;12:217–28.
Bonenberger M, Plener PL, Groschwitz RC, Gron G, Abler B. Differential neural processing of unpleasant haptic sensations in somatic and affective partitions of the insula in non-suicidal self-injury (NSSI). Psychiatry Res. 2015;234:298–304.
Guo Y, Lu R, Ou Y, Huang Y, Li J, Cui Y, et al. A study on the association between prefrontal functional connectivity and non-suicidal self-injury in adolescents with depression. Front Neurol. 2024;15:1382136.
Lee SE, Shin H, Kim G, Moon H, Hur JW. Decreased gray matter volume in regions associated with affective pain processing in unmedicated individuals with nonsuicidal self-injury. Psychiatry Res. 2023;326:115314.
Malejko K, Neff D, Brown RC, Plener PL, Bonenberger M, Abler B, et al. Somatosensory stimulus intensity encoding in borderline personality disorder. Front Psychol. 2018;9:1853.
Dahlgren MK, Hooley JM, Best SG, Sagar KA, Gonenc A, Gruber SA. Prefrontal cortex activation during cognitive interference in nonsuicidal self-injury. Psychiatry Res Neuroimaging. 2018;277:28–38.
Kim KL, Galvan T, Puzia ME, Cushman GK, Seymour KE, Vanmali R, et al. Psychiatric and self‐injury profiles of adolescent suicide attempters versus adolescents engaged in nonsuicidal self‐injury. Suicide Life Threat Behav. 2015;45:37–50.
Santamarina-Perez P, Romero S, Mendez I, Leslie SM, Packer MM, Sugranyes G, et al. Fronto-limbic connectivity as a predictor of improvement in nonsuicidal self-injury in adolescents following psychotherapy. J Child Adolesc Psychopharmacol. 2019;29:456–65.
Mürner-Lavanchy I, Josi J, Koenig J, Reichl C, Brunner R, Kaess M. Resting-state functional connectivity predicting clinical improvement following treatment in female adolescents with non-suicidal self-injury. J Affect Disord. 2023;327:79–86.
Dai L, Zhang X, Yu R, Wang X, Deng F, Li X, et al. Abnormal brain spontaneous activity in major depressive disorder adolescents with non-suicidal self injury and its changes after sertraline therapy. Front Psychiatry. 2023;14:1177227.
Denison T, Morrell MJ. Neuromodulation in 2035: the neurology future forecasting series. Neurology. 2022;98:65–72.
Liao C, Gu X, Wang J, Li K, Wang X, Zhao M, et al. The relation between neuroticism and non-suicidal self-injury behavior among college students: multiple mediating effects of emotion regulation and depression. Int J Environ Res Public Health. 2022;19:2885.
Kazgan Kılıçaslan A, Yıldız S, Kurt O, Atmaca M. Comparison of non-suicidal self-injury and suicide attempts in relation to anger rumination. Alpha Psychiatry. 2022;23:82–8.
Savla HY, Sutar D. A qualitative study on understanding the process of nonsuicidal self-injury. Ann Indian Psychiatry. 2024;8:217–25.
Gratz KL. Risk factors for and functions of deliberate self-harm: an empirical and conceptual review. Clin Psychol: Sci Pract. 2003;10:192.
Başgöze Z, Demers L, Thai M, Falke CA, Mueller BA, Fiecas MB, et al. A multilevel examination of cognitive control in adolescents with nonsuicidal self-injury. Biol Psychiatry Glob Open Sci. 2023;3:855–66.
Zahid Z, McMahon L, Lynch M. Neural activity across the dorsolateral prefrontal cortex and risk for suicidal ideation and self-injury. Arch Suicide Res. 2022;26:187–207.
Luu P, Tucker DM. Self-regulation by the medial frontal cortex. In: Beauregard M, ed. Consciousness, Emotional Self-Regulation and the Brain. 2004:123-9.
Bush G, Shin L, Holmes J, Rosen B, Vogt B. The multi-source interference task: validation study with fMRI in individual subjects. Mol Psychiatry. 2003;8:60–70.
Drevets WC. Neuroimaging abnormalities in the amygdala in mood disorders. Ann N Y Acad Sci. 2003;985:420–44.
Başgöze Z, Mirza SA, Silamongkol T, Hill D, Falke C, Thai M, et al. Multimodal assessment of sustained threat in adolescents with nonsuicidal self-injury. Dev Psychopathol. 2021;33:1774–92.
Clewett D, Schoeke A, Mather M. Amygdala functional connectivity is reduced after the cold pressor task. Cogn Affect Behav Neurosci. 2013;13:501–18.
Fountoulakis KN, Giannakopoulos P, Kövari E, Bouras C. Assessing the role of cingulate cortex in bipolar disorder: neuropathological, structural and functional imaging data. Brain Res Rev. 2008;59:9–21.
Nam G, Moon H, Lee JH, Hur JW. Self-referential processing in individuals with nonsuicidal self-injury: an fMRI study. Neuroimage Clin. 2022;35:103058.
Craig AD. How do you feel—now? The anterior insula and human awareness. Nat Rev Neurosci. 2009;10:59–70.
Mayo LM, Perini I, Gustafsson PA, Hamilton JP, Kämpe R, Heilig M, et al. Psychophysiological and neural support for enhanced emotional reactivity in female adolescents with nonsuicidal self-injury. Biol Psychiatry Cogn Neurosci Neuroimaging. 2021;6:682–91.
Chapman AL, Gratz KL, Brown MZ. Solving the puzzle of deliberate self-harm: the experiential avoidance model. Behav Res Ther. 2006;44:371–94.
Selby EA, Nock MK, Kranzler A. How does self-injury feel? Examining automatic positive reinforcement in adolescent self-injurers with experience sampling. Psychiatry Res. 2014;215:417–23.
Stacy SE, Bandel SL, Lear MK, Pepper CM. Before, during, and after self injury: the practice patterns of nonsuicidal self injury. J Nerv Ment Dis. 2018;206:522–7.
Ando A, Reichl C, Scheu F, Bykova A, Parzer P, Resch F, et al. Regional grey matter volume reduction in adolescents engaging in non-suicidal self-injury. Psychiatry Res Neuroimaging. 2018;280:48–55.
Poon JA, Thompson JC, Forbes EE, Chaplin TM. Adolescents’ reward-related neural activation: links to thoughts of nonsuicidal self-injury. Suicide Life Threat Behav. 2019;49:76–89.
Sauder CL, Derbidge CM, Beauchaine TP. Neural responses to monetary incentives among self-injuring adolescent girls. Dev Psychopathol. 2016;28:277–91.
Case JAC, Mattoni M, Olino TM. Examining the neurobiology of non-suicidal self-injury in children and adolescents: the role of reward responsivity. J Clin Med. 2021;10:3561.
Bonica JJ. The relation of injury to pain. Pain. 1979;7:203–7.
Eisenberger NI. Social pain and the brain: controversies, questions, and where to go from here. Annu Rev Psychol. 2015;66:601–29.
Yao M, Lei Y, Li P, Ye Q, Liu Y, Li X, et al. Shared sensitivity to physical pain and social evaluation. J Pain. 2020;21:677–88.
Kim DJ, Job A, Gokarakonda S, Huang C, Chekuri L, Carbajal JM, et al. Synergistic effect of chronic pain and nonsuicidal self-harm on pain sensitivity. Eur Arch Psychiatry Clin Neurosci. 2022;272:371–80.
Brown RC, Plener PL, Groen G, Neff D, Bonenberger M, Abler B. Differential neural processing of social exclusion and inclusion in adolescents with non-suicidal self-injury and young adults with borderline personality disorder. Front Psychiatry. 2017;8:267.
Lalouni M, Fust J, Bjureberg J, Kastrati G, Fondberg R, Fransson P, et al. Augmented pain inhibition and higher integration of pain modulatory brain networks in women with self-injury behavior. Mol Psychiatry. 2022;27:3452–9.
Koenig J, Rinnewitz L, Warth M, Hillecke TK, Brunner R, Resch F, et al. Psychobiological response to pain in female adolescents with nonsuicidal self-injury. J Psychiatry Neurosci. 2017;42:189–99.
Ghashghaei HT, Barbas H. Pathways for emotion: interactions of prefrontal and anterior temporal pathways in the amygdala of the rhesus monkey. Neuroscience. 2002;115:1261–79.
Allman JM, Hakeem A, Erwin JM, Nimchinsky E, Hof P. The anterior cingulate cortex. The evolution of an interface between emotion and cognition. Ann N Y Acad Sci. 2001;935:107–17.
Ballard E, Bosk A, Pao M. Invited commentary: understanding brain mechanisms of pain processing in adolescents’ non-suicidal self-injury. J Youth Adolesc. 2010;39:327–34.
Eisenberger NI. The neural bases of social pain: evidence for shared representations with physical pain. Psychosom Med. 2012;74:126–35.
Zubieta JK, Smith YR, Bueller JA, Xu Y, Kilbourn MR, Jewett DM, et al. Regional mu opioid receptor regulation of sensory and affective dimensions of pain. Science. 2001;293:311–5.
Bresin K, Gordon KH. Endogenous opioids and nonsuicidal self-injury: a mechanism of affect regulation. Neurosci Biobehav Rev. 2013;37:374–83.
Blasco-Fontecilla H, Herranz-Herrer J, Ponte-Lopez T, Gil-Benito E, Donoso-Navarro E, Hernandez-Alvarez E, et al. Serum beta-endorphin levels are associated with addiction to suicidal behavior: a pilot study. Eur Neuropsychopharmacol. 2020;40:38–51.
Roy A, Roy M, Deb S, Unwin G, Roy A. Are opioid antagonists effective in reducing self-injury in adults with intellectual disability? A systematic review. J Intellect Disabil Res. 2015;59:55–67.
Schmahl C, Baumgartner U. Pain in borderline personality disorder. Mod Trends Pharmacopsychiatry. 2015;30:166–75.
Reitz S, Kluetsch R, Niedtfeld I, Knorz T, Lis S, Paret C, et al. Incision and stress regulation in borderline personality disorder: neurobiological mechanisms of self-injurious behaviour. Br J Psychiatry. 2015;207:165–72.
He S, Li F, Gu T, Ma H, Li X, Zou S, et al. Reduced corticostriatal functional connectivity in temporomandibular disorders. Hum Brain Mapp. 2018;39:2563–72.
Mazzola L, Isnard J, Peyron R, Mauguiere F. Stimulation of the human cortex and the experience of pain: Wilder Penfield’s observations revisited. Brain. 2012;135:631–40.
Hamza CA, Willoughby T, Heffer T. Impulsivity and nonsuicidal self-injury: a review and meta-analysis. Clin Psychol Rev. 2015;38:13–24.
Oldham JM. Impulsivity and compulsivity. American Psychiatric Pub: Washington, DC; 1996.
Pournaghash-Tehrani S. Infidelity, impulsivity, and marital ad-justment. J Psychiatry Depress Anxiety. 2019;5:020.
Cassels M, Neufeld S, van Harmelen A-L, Goodyer I, Wilkinson P. Prospective pathways from impulsivity to non-suicidal self-injury among youth. Arch Suicide Res. 2022;26:534–47.
Herman AM, Critchley HD, Duka T. Risk-taking and impulsivity: the role of mood states and interoception. Front Psychol. 2018;9:1625.
Behan B, Stone A, Garavan H. Right prefrontal and ventral striatum interactions underlying impulsive choice and impulsive responding. Hum Brain Mapp. 2015;36:187–98.
Hallett M. Transcranial magnetic stimulation: a primer. Neuron. 2007;55:187–99.
O’Reardon JP, Solvason HB, Janicak PG, Sampson S, Isenberg KE, Nahas Z, et al. Efficacy and safety of transcranial magnetic stimulation in the acute treatment of major depression: a multisite randomized controlled trial. Biol Psychiatry. 2007;62:1208–16.
Gao C, Liu J, Tan Y, Chen S. Freezing of gait in Parkinson’s disease: pathophysiology, risk factors and treatments. Transl Neurodegener. 2020;9:12.
Koch G, Casula EP, Bonnì S, Borghi I, Assogna M, Minei M, et al. Precuneus magnetic stimulation for Alzheimer’s disease: a randomized, sham-controlled trial. Brain. 2022;145:3776–86.
Liu J, Guan J, Xiong J, Wang F. Effects of transcranial magnetic stimulation combined with sertraline on cognitive level, inflammatory response and neurological function in depressive disorder patients with non-suicidal self-injury behavior. Actas Esp Psiquiatr. 2024;52:28–36.
Gao J, Xiao X, Li A, Chu N, Yongjin N, editors. Effect of low frequency repetitive transcranial magnetic stimulation treatment on non-suicidal self-injury behaviour and intention of depressed adolescents. International conference on mental health and humanities education (ICMHHE 2020). Atlantis Press; 2020.
Cash RFH, Cocchi L, Lv J, Fitzgerald PB, Zalesky A. Functional magnetic resonance imaging-guided personalization of transcranial magnetic stimulation treatment for depression. JAMA Psychiatry. 2021;78:337–9.
Huang YZ, Edwards MJ, Rounis E, Bhatia KP, Rothwell JC. Theta burst stimulation of the human motor cortex. Neuron. 2005;45:201–6.
Zhang M, Li W, Ye Y, Hu Z, Zhou Y, Ning Y. Efficacy and safety of intermittent theta burst stimulation on adolescents and young adults with major depressive disorder: a randomized, double blinded, controlled trial. J Affect Disord. 2024;350:214–21.
Voigt JD, Leuchter AF, Carpenter LL. Theta burst stimulation for the acute treatment of major depressive disorder: a systematic review and meta-analysis. Transl Psychiatry. 2021;11:330.
Plewnia C, Pasqualetti P, Grosse S, Schlipf S, Wasserka B, Zwissler B, et al. Treatment of major depression with bilateral theta burst stimulation: a randomized controlled pilot trial. J Affect Disord. 2014;156:219–23.
Mitra A, Raichle ME, Geoly AD, Kratter IH, Williams NR. Targeted neurostimulation reverses a spatiotemporal biomarker of treatment-resistant depression. Proc Natl Acad Sci USA. 2023;120:e2218958120.
Cole EJ, Phillips AL, Bentzley BS, Stimpson KH, Nejad R, Barmak F, et al. Stanford neuromodulation therapy (SNT): a double-blind randomized controlled trial. Am J Psychiatry. 2022;179:132–41.
Liu A, Vöröslakos M, Kronberg G, Henin S, Krause MR, Huang Y, et al. Immediate neurophysiological effects of transcranial electrical stimulation. Nat Commun. 2018;9:5092.
Yavari F, Jamil A, Mosayebi Samani M, Vidor LP, Nitsche MA. Basic and functional effects of transcranial electrical stimulation (tES)-an introduction. Neurosci Biobehav Rev. 2018;85:81–92.
Makowska I, Rymarczyk K, Puzio D, Pałka-Szafraniec K, Garnier J. Emotional regulation in non-suicidal self-injury–research on the use of transcranial direct current stimulation (tDCS). Eur Psychiatry. 2022;65:S445–S6.
Edwards D, Cortes M, Datta A, Minhas P, Wassermann EM, Bikson M. Physiological and modeling evidence for focal transcranial electrical brain stimulation in humans: a basis for high-definition tDCS. Neuroimage. 2013;74:266–75.
Helfrich RF, Knepper H, Nolte G, Strüber D, Rach S, Herrmann CS, et al. Selective modulation of interhemispheric functional connectivity by HD-tACS shapes perception. PLoS Biol. 2014;12:e1002031.
Grossman N, Bono D, Dedic N, Kodandaramaiah SB, Rudenko A, Suk HJ, et al. Noninvasive deep brain stimulation via temporally interfering electric fields. Cell. 2017;169:1029–41.e16
Sackeim HA. Modern electroconvulsive therapy: vastly improved yet greatly underused. JAMA Psychiatry. 2017;74:779–80.
Espinoza RT, Kellner CH. Electroconvulsive therapy. N Engl J Med. 2022;386:667–72.
Rönnqvist I, Nilsson FK, Nordenskjöld A. Electroconvulsive therapy and the risk of suicide in hospitalized patients with major depressive disorder. JAMA Netw Open. 2021;4:e2116589.
Tor PC, Tan XW, Martin D, Loo C. Comparative outcomes in electroconvulsive therapy (ECT): a naturalistic comparison between outcomes in psychosis, mania, depression, psychotic depression and catatonia. Eur Neuropsychopharmacol. 2021;51:43–54.
McCall WV, Lisanby SH, Rosenquist PB, Dooley M, Husain MM, Knapp RG, et al. Effects of continuation electroconvulsive therapy on quality of life in elderly depressed patients: a randomized clinical trial. J Psychiatr Res. 2018;97:65–9.
Mutz J, Vipulananthan V, Carter B, Hurlemann R, Fu CHY, Young AH. Comparative efficacy and acceptability of non-surgical brain stimulation for the acute treatment of major depressive episodes in adults: systematic review and network meta-analysis. BMJ. 2019;364:l1079.
Rootes-Murdy K, Carlucci M, Tibbs M, Wachtel LE, Sherman MF, Zandi PP, et al. Non-suicidal self-injury and electroconvulsive therapy: outcomes in adolescent and young adult populations. J Affect Disord. 2019;250:94–8.
Lisanby SH. Update on magnetic seizure therapy: a novel form of convulsive therapy. J ECT. 2002;18:182–8.
Lisanby SH, Schlaepfer TE, Fisch H-U, Sackeim HA. Magnetic seizure therapy of major depression. Arch Gen Psychiatry. 2001;58:303–5.
Daskalakis ZJ, Dimitrova J, McClintock SM, Sun Y, Voineskos D, Rajji TK, et al. Magnetic seizure therapy (MST) for major depressive disorder. Neuropsychopharmacology. 2020;45:276–82.
Deng ZD, Luber B, McClintock SM, Weiner RD, Husain MM, Lisanby SH. Clinical outcomes of magnetic seizure therapy vs electroconvulsive therapy for major depressive episode: a randomized clinical trial. JAMA Psychiatry. 2024;81:240–9.
Sun Y, Blumberger DM, Mulsant BH, Rajji TK, Fitzgerald PB, Barr MS, et al. Magnetic seizure therapy reduces suicidal ideation and produces neuroplasticity in treatment-resistant depression. Transl Psychiatry. 2018;8:253.
Sun Y, Farzan F, Mulsant BH, Rajji TK, Fitzgerald PB, Barr MS, et al. Indicators for remission of suicidal ideation following magnetic seizure therapy in patients with treatment-resistant depression. JAMA Psychiatry. 2016;73:337–45.
Weissman CR, Blumberger DM, Dimitrova J, Throop A, Voineskos D, Downar J, et al. Magnetic seizure therapy for suicidality in treatment-resistant depression. JAMA Network Open. 2020;3:e207434.e.
Gorodetsky C, Mithani K, Breitbart S, Yan H, Zhang K, Gouveia FV, et al. Deep brain stimulation of the nucleus accumbens for severe self-injurious behavior in children: a phase I pilot trial. Biol Psychiatry. 2024;97:1116–26.
Zhou D, Li X, Wei S, Yu C, Wang D, Li Y, et al. Transcranial direct current stimulation combined with repetitive transcranial magnetic stimulation for depression: a randomized clinical trial. JAMA Netw Open. 2024;7:e2444306.
Zhou Q, Liu Z, Yu C, Wang Q, Zhuang W, Tang Y, et al. Effect of combined treatment with transcranial direct current stimulation and repetitive transcranial magnetic stimulation compared to monotherapy for the treatment of chronic insomnia: a randomised, double-blind, parallel-group, controlled trial. BMC Med. 2024;22:538.
Kaess M, Koenig J, Bauer S, Moessner M, Fischer-Waldschmidt G, Mattern M, et al. Self-injury: treatment, assessment, recovery (STAR): online intervention for adolescent non-suicidal self-injury - study protocol for a randomized controlled trial. Trials. 2019;20:425.
Slee N, Arensman E, Garnefski N, Spinhoven P. Cognitive-behavioral therapy for deliberate self-harm. Crisis. 2007;28:175–82.
Taylor LM, Oldershaw A, Richards C, Davidson K, Schmidt U, Simic M. Development and pilot evaluation of a manualized cognitive-behavioural treatment package for adolescent self-harm. Behav Cogn Psychother. 2011;39:619–25.
Di Vincenzo JD, Siegel A, Lipsitz O, Ho R, Teopiz KM, Ng J, et al. The effectiveness, safety and tolerability of ketamine for depression in adolescents and older adults: a systematic review. J Psychiatr Res. 2021;137:232–41.
Yang JW, Jung SW, Lee H. Low-dose clozapine monotherapy for recurrent non-suicidal self-injury: a case report. Asian J Psychiatr. 2022;73:103113.
Yovell Y, Bar G, Mashiah M, Baruch Y, Briskman I, Asherov J, et al. Ultra-low-dose buprenorphine as a time-limited treatment for severe suicidal ideation: a randomized controlled trial. Am J Psychiatry. 2016;173:491–8.
Zrenner C, Belardinelli P, Müller-Dahlhaus F, Ziemann U. Closed-loop neuroscience and non-invasive brain stimulation: a tale of two loops. Front Cell Neurosci. 2016;10:92.
Lo MC, Widge AS. Closed-loop neuromodulation systems: next-generation treatments for psychiatric illness. Int Rev Psychiatry. 2017;29:191–204.
Oxley T, Opie N. Closed-loop neuromodulation: listen to the body. World Neurosurg. 2019;122:415–6.
Harland T, Elliott T, Telkes I, Pilitsis JG. Machine learning in pain neuromodulation. Adv Exp Med Biol. 2024;1462:499–512.
Wang DX, Ng N, Seger SE, Ekstrom AD, Kriegel JL, Lega BC. Machine learning classifiers for electrode selection in the design of closed-loop neuromodulation devices for episodic memory improvement. Cereb Cortex. 2023;33:8150–63.
De Ridder D, Maciaczyk J, Vanneste S. The future of neuromodulation: smart neuromodulation. Expert Rev Med Devices. 2021;18:307–17.
Acknowledgements
The authors would like to thank Prof. Yuhui Wan, Department of Health Promotion and Behavioral Sciences, Anhui Medical University, Prof. Jiajia Zhu, Department of Radiology, The First Affiliated Hospital of Anhui Medical University, and Dr. Bing Leng, Anhui Medical University, for their collective contributions to this work.
Funding
This work was supported by National Natural Science Foundation of China (Grant Nos. U24A20702 and 32071054) and Research Fund of Anhui Institute of Translational Medicine (Grant No. 2021zhyx-B10).
Author information
Authors and Affiliations
Contributions
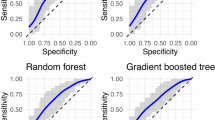
DW, SW, and HW conducted the literature search, drafted the initial manuscript, and contributed to manuscript editing. DW and JZ were responsible for figure preparation and assisted with figure interpretation. YT oversaw the entire review process, ensuring its accuracy and completeness, and was responsible for the final submission. All authors critically reviewed the manuscript and approved the final submitted version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wu, D., Wang, S., Wang, H. et al. Neural mechanisms and neuromodulation therapies for non-suicidal self-injury. Mol Psychiatry 30, 5513–5522 (2025). https://doi.org/10.1038/s41380-025-03125-7
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41380-025-03125-7