Abstract
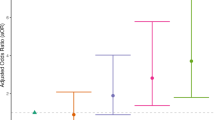
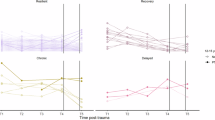
Posttraumatic stress disorder (PTSD) is persistent over time, thus identifying risk factors for chronic PTSD is crucial for clinical research. Trauma exposure severity and polygenic liability are two established predictors of PTSD onset and severity, but their contributions to the long-term course of PTSD remain largely unknown. In this prospective longitudinal cohort study, we tested whether severity of trauma exposure and polygenic risk for symptoms of PTSD independently predict long-term trajectories of PTSD symptoms. Data included 49,402 observations, spanning July 2002 to December 2022, from n = 5687 World Trade Center responders who had predominately European ancestry (baseline mean age = 37.74, SD = 8.19, range = 16–75; 92.89% male). First, the best-fitting model of 20-year PTSD trajectories was determined. Next, a polygenic risk score and a sum score of traumatic exposures were included as predictors of individual differences in intercepts (initial levels) and slopes (rates of change), adjusting for demographic covariates. The polygenic risk score significantly predicted rates of change in PTSD symptoms, independent of the intercept, such that higher polygenic risk was associated with more rapid increases in the years after trauma and a steeper arch-shaped trajectory. Exposure severity predicted initial levels and rates of change in symptoms, with more pronounced effects on initial levels. These findings indicate that polygenic liability and exposure severity predict the long-term prognosis of PTSD and have the potential to inform future clinical studies in trauma-exposed populations.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
Data not provided in the article because of space limitations are not publicly shared due to ethical considerations. Study participants provided consent for their data to be analyzed by study personnel. To respect the autonomy and privacy of the WTC responders, the data underlying the reported results will be made available to qualified investigators whose proposed use of the data has been approved by an internal review committee and the Institutional Review Board at Stony Brook University. This access will be granted up to 4 years after publication of this study following rigorous de-identification of sensitive information. Requests for data access will be reviewed, and a response will be provided within 60 days of submission.
Code availability
Correspondence concerning this article should be addressed to the first author, frank.mann@stonybrookmedicine.edu, including requests for a copy of the code that was used to conduct analyses.
References
Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Archives of General Psychiatry. 2005;62:593–602.
Kilpatrick DG, Resnick HS, Milanak ME, Miller MW, Keyes KM, Friedman MJ. National estimates of exposure to traumatic events and PTSD prevalence using DSM‐IV and DSM‐5 criteria. Journal of traumatic stress. 2013;26:537–47.
Fulton JJ, Calhoun PS, Wagner HR, Schry AR, Hair LP, Feeling N, et al. The prevalence of posttraumatic stress disorder in operation enduring freedom/operation iraqi freedom (OEF/OIF) veterans: a meta-analysis. Journal of anxiety disorders. 2015;31:98–107.
Schein J, Houle C, Urganus A, Cloutier M, Patterson-Lomba O, Wang Y, et al. Prevalence of post-traumatic stress disorder in the United States: a systematic literature review. Current medical research and opinion. 2021;37:2151–61.
Petrie K, Milligan-Saville J, Gayed A, Deady M, Phelps A, Dell L, et al. Prevalence of PTSD and common mental disorders amongst ambulance personnel: a systematic review and meta-analysis. Social psychiatry and psychiatric epidemiology. 2018;53:897–909.
Syed S, Ashwick R, Schlosser M, Jones R, Rowe S, Billings J. Global prevalence and risk factors for mental health problems in police personnel: a systematic review and meta-analysis. Occupational and environmental medicine. 2020;77:737–47.
Bowler RM, Adams SW, Gocheva VV, Li J, Mergler D, Brackbill R, et al. Posttraumatic stress disorder, gender, and risk factors: World Trade Center tower survivors 10 to 11 years after the September 11, 2001 attacks. Journal of Traumatic Stress. 2017;30:564–70.
Bromet EJ, Hobbs MJ, Clouston SA, Gonzalez A, Kotov R, Luft BJ. DSM-IV post-traumatic stress disorder among World Trade Center responders 11–13 years after the disaster of 11 September 2001 (9/11). Psychological medicine. 2016;46:771–83.
Berger W, Coutinho ESF, Figueira I, Marques-Portella C, Luz MP, Neylan TC, et al. Rescuers at risk: a systematic review and meta-regression analysis of the worldwide current prevalence and correlates of PTSD in rescue workers. Social psychiatry and psychiatric epidemiology. 2012;47:1001–11.
Kessler RC, Aguilar-Gaxiola S, Alonso J, Benjet C, Bromet EJ, Cardoso G, et al. Trauma and PTSD in the WHO world mental health surveys. European journal of psychotraumatology. 2017;8:1353383.
Morina N, Wicherts JM, Lobbrecht J, Priebe S. Remission from post-traumatic stress disorder in adults: a systematic review and meta-analysis of long term outcome studies. Clinical psychology review. 2014;34:249–55.
Diamond PR, Airdrie JN, Hiller R, Fraser A, Hiscox LV, Hamilton-Giachritsis C, et al. Change in prevalence of post-traumatic stress disorder in the two years following trauma: a meta-analytic study. European Journal of Psychotraumatology. 2022;13:2066456.
Burback L, Brult-Phillips S, Nijdam MJ, McFarlane A, Vermetten E. Treatment of posttraumatic stress disorder: a state-of-the-art review. Current Neuropharmacology. 2024;22:557–635.
Lewis C, Roberts NP, Gibson S, Bisson JI. Dropout from psychological therapies for post-traumatic stress disorder (PTSD) in adults: systematic review and meta-analysis. European journal of psychotraumatology. 2020;11:1709709.
Steenkamp MM, Litz BT, Hoge CW, Marmar CR. Psychotherapy for military-related PTSD: a review of randomized clinical trials. Jama. 2015;314:489–500.
Ryder AL, Azcarate PM, Cohen BE. PTSD and physical health. Current Psychiatry Reports. 2018;20:1–8.
Kessler RC. Posttraumatic stress disorder: the burden to the individual and to society. Journal of Clinical Psychiatry. 2000;61:4–14.
Davis LL, Schein J, Cloutier M, Guerin A, Schein J, Gagnon-Sanschagrin P, et al. The economic burden of posttraumatic stress disorder in the United States from a societal perspective. The Journal of Clinical Psychiatry. 2022;83:40672.
Duncan L, Cooper BN, Shen H. Robust findings from 25 years of PSTD genetics research. Current Psychiatry Reports. 2018;20:115.
Duncan L, Ratanatharathorn A, Aiello AE, Almli LM, Amstadter AB, Ashley-Koch AE, et al. Largest GWAS of PTSD (N=20 070) yields genetic overlap with schizophrenia and sex differences in heritability. Original Article. Mol Psychiatry. 2017;23:666–73. https://doi.org/10.1038/mp.2017.77
Nievergelt CM, Maihofer AX, Klengel T, Atkinson EG, Chen CY, Choi KW, et al. International meta-analysis of PTSD genome-wide association studies identifies sex-and ancestry-specific genetic risk loci. Nature communications. 2019;10:1–16.
Gelernter J, Sun N, Polimanti R, Pietrzak R, Levey DF, Bryois J, et al. Genome-wide association study of post-traumatic stress disorder reexperiencing symptoms in> 165,000 US veterans. Nature neuroscience. 2019;22:1394–401.
Waszczuk MA, Docherty AR, Shabalin AA, Miao J, Yang X, Kuan P, et al. Polygenic prediction of PTSD trajectories in 9/11 responders. Psychological medicine. 2022;52:1981–9.
Weber H, Maihofer AX, Jaksic N, Bojic EF, Kucukalic S, Dzananovic ES, et al. Association of polygenic risk scores, traumatic life events and coping strategies with war-related PTSD diagnosis and symptom severity in the South Eastern Europe (SEE)-PTSD cohort. Journal of Neural Transmission. 2022;129:1–14.
Lobo JJ, McLean SA, Tungate AS, Peak DA, Swor RA, Rathlev NK, et al. Polygenic risk scoring to assess genetic overlap and protective factors influencing posttraumatic stress, depression, and chronic pain after motor vehicle collision trauma. Translational Psychiatry. 2021;11:359.
Stein MB, Jain S, Parodi L, Choi KW, Maihofer AX, Nelson LD, et al. Polygenic risk for mental disorders as predictors of posttraumatic stress disorder after mild traumatic brain injury. Translational psychiatry. 2023;13:24.
Campbell-Sills L, Sun X, Choi KW, He F, Ursano RJ, Kesssler RC, et al. Dissecting the heterogeneity of posttraumatic stress disorder: differences in polygenic risk, stress exposures, and course of PTSD subtypes. Psychological medicine. 2022;52:3646–54.
Misganaw B, Guffanti G, Lori A, Abu-Amara D, Flory JD, Mueller S, et al. Polygenic risk associated with post-traumatic stress disorder onset and severity. Translational psychiatry. 2019;9:165.
Campbell-Sills L, Papini S, Norman SB, Choi KW, He F, Sun Xiaoying, et al. Associations of polygenic risk scores with posttraumatic stress symptom trajectories following combat deployment. Psychological medicine. 2023;53:1–10.
Pingault JB, Allegrini AG, Odigie T, Frach L, Baldwin JR, Rijsdijk F, et al. Research review: how to interpret associations between polygenic scores, environmental risks, and phenotypes. Journal of Child Psychology and Psychiatry. 2022;63:1125–39.
Sayed S, Iacoviello BM, Charney DS. Risk factors for the development of psychopathology following trauma. Current psychiatry reports. 2015;17:1–7.
Tortella-Feliu M, Fullana MA, Pérez-Vigil A, Torres X, Chamorro J, Littarelli SA, et al. Risk factors for posttraumatic stress disorder: an umbrella review of systematic reviews and meta-analyses. Neuroscience & Biobehavioral Reviews. 2019;107:154–65.
Mann FD, Waszczuk MA, Clouston SAP, Feltman S, Ruggero CJ, Marx BP, et al. Long-Term Trajectories of Posttraumatic Stress Disorder Symptoms: A 20-Year Longitudinal Study of World Trade Center Responders. Nature Mental Health. 2025;3:789–802.
Ge T, Chen C-Y, Ni Y, Feng Y-CA, Smoller JW. Polygenic prediction via bayesian regression and continuous shrinkage priors. Nature Communications. 2019;10:1776–85.
Stein MB, Levey DF, Cheng Z, Wendt FR, Harrington K, Pathak GA, et al. Genome-wide association analyses of post-traumatic stress disorder and its symptom subdomains in the million veteran program. Nature genetics. 2021;53:174–84.
Pietrzak R, Feder A, Singh R, Schechter CB, Bromet EJ, Katz CL, et al. Trajectories of PTSD risk and resilience in World Trade Center responders: an 8-year prospective cohort study. Psychological medicine. 2014;44:205–19.
Zvolensky MJ, Kotov R, Schechter CB, Gonzalez A, Vujanovic A, Pietrzak RH, et al. Post-disaster stressful life events and WTC-related posttraumatic stress, depressive symptoms, and overall functioning among responders to the World Trade Center disaster. Journal of Psychiatric Research. 2015;61:97–105.
R Core Team. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing. Vienna, Austria; 2023
Bates, D., Mächler, M., Bolker, B., & Walker, S. Fitting linear mixed-effects models using lme4. Journal of Statistical Software. 2015;67:1–48.
Pinheiro J, Bates D, DebRoy S. Package ‘nlme’. linear and Nonlinear Mixed Effects Models, Version. 2017;3:274.
Proust-Lima C, Philipps V, Liquet B. Estimation of extended mixed models using latent classes and latent processes: the R package lcmm. Journal of Statistical Software. 2017;78:1–56.
Grimm KJ, Ram N, Estabrook R. Growth modeling: structural equation and multilevel modeling approaches. Guilford Publications; New York; 2016.
Kendler K, Gardner C, Lichtenstein P. A developmental twin study of symptoms of anxiety and depression: evidence for genetic innovation and attenuation. Psychological medicine. 2008;38:1567–75.
Chang Z, Lichtenstein P, Asherson PJ, Larsson H. Developmental twin study of attention problems: high heritabilities throughout development. JAMA psychiatry. 2013;70:311–8.
Waszczuk M, Zavos H, Gregory AM, Eley TC. The stability and change of etiological influences on depression, anxiety symptoms and their co-occurrence across adolescence and young adulthood. Psychological medicine. 2016;46:161–75.
Moreno-Grau S, Vernekar M, Lopez-Pineda A, Mas-Montserrat D, Barrabés M, Quinto-Cortés CD, et al. Polygenic risk score portability for common diseases across genetically diverse populations. Human Genomics. 2024;18:93.
Ndong Sima CAA, Step K, Swart Y, Schurz H, Uren C, Möller M. Methodologies underpinning polygenic risk scores estimation: a comprehensive overview. Human Genetics. 2024;143:1265–80.
Kandaswamy R, Allegrini A, Nancarrow AF, Cave SN, Plomin R, Von Stumm S. Predicting alcohol use from genome-wide polygenic scores, environmental factors, and their interactions in young adulthood. Psychosomatic medicine. 2022;84:244–50.
Plomin R, Gidziela A, Malanchini M, Von Stumm S. Gene–environment interaction using polygenic scores: Do polygenic scores for psychopathology moderate predictions from environmental risk to behavior problems? Development and Psychopathology. 2022;34:1816–26.
Acknowledgements
We thank the WTC responders from the General Responder Cohort whose participation was integral to this work. Data collection was funded by CDC 2011-200-39361 awarded to B.J.L. and U01OH011864 awarded to M.A.W, and by the SUNY Research Foundation. The analyses were partially funded by R21AG074705-01 awarded to F.D.M.
Author information
Authors and Affiliations
Contributions
BJL, RK and MAW designed the study. BJL, MAC, and XY. coordinated and supervised data collection. AAS. and ARD. calculated polygenic risk scores. In consultation with RK, FDM. conducted the primary analyses, created tables and figures, and drafted the methods and results. MAW drafted the introduction and discussion. SAP, EJB, BPM, AAS, ARD, PK, MAC, XY, BJL and RK provided critical feedback and revisions, and all authors approved a final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics
Data collection was performed in accordance with ethnical guidelines approved by the Institutional Review Board at Stony Brook University (ethical approval number: 604113; WTC Health and Wellness Study) and all participants provided informed written consent. The participants were provided free screening and treatment for WTC-related health conditions and were not compensated otherwise.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mann, F.D., Waszczuk, M.A., Clouston, S.A.P. et al. Polygenic Risk and Exposure Severity Predict Trajectories of PTSD: A Prospective Cohort Study. Mol Psychiatry 31, 39–47 (2026). https://doi.org/10.1038/s41380-025-03235-2
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41380-025-03235-2