Abstract
Objective
Antidepressant use during pregnancy has been increasing in the last few decades. A substantial body of evidence has indicated the increased risks of adverse health outcomes for both pregnant women and their offspring. The association may be biased by uncontrolled confounding of maternity depression or mental health status. We performed a systematic review and meta-analysis to generate comprehensive estimates of the association between depression, antidepressants, and reproductive outcomes.
Methods
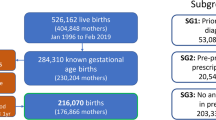
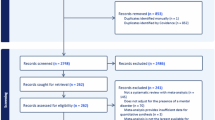
The PubMed and Embase were searched from database inception to Jul 29, 2025, for longitudinal cohort studies of pregnant women with exposure to antidepressant or depression. The Newcastle-Ottawa Scale was used for assessing the methodological quality of included studies. Pooled estimates of risk ratio (RR) were calculated by comparing adverse outcomes between antidepressant-exposed pregnancies and unexposed pregnancies. Subsequently, we analyzed the risks of antidepressant-treated, untreated antenatal depression by adjusting for disease factors. Totally, 20 adverse health outcomes including 6 maternal and 14 children’s outcomes were accessed.
Results
A total of 166 studies with 51,596,405 participants were included. When antidepressant-exposed pregnancies were compared to all unexposed pregnancies (with and without depression), an increased risk for the majority (16/20) of the focused adverse outcomes was found. After adjusting for depression, results shows that certain adverse outcomes remained significant among untreated pregnancies. However, compared with untreated depressed women, the treated by antidepressant for depressed women during pregnancy was associated with the increased risk for limited outcomes of preterm birth and NICU admission.
Conclution
The findings indicated that many of the adverse outcomes observed with medication may be attributable to the underlying depression itself rather than of antidepressants. More attention should be paid to depression, and health professionals should estimate the risk of depression and antidepressant comprehensively during counseling and prenatal health care.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Chatillon O, Even C. Antepartum depression: prevalence, diagnosis and treatment. Encephale. 2010;36:443–51.
Gelaye B, Rondon MB, Araya R, Williams MA. Epidemiology of maternal depression, risk factors, and child outcomes in low-income and middle-income countries. Lancet Psychiatry. 2016;3:973–82.
Hallberg P, Sjöblom V. The use of selective serotonin reuptake inhibitors during pregnancy and breast-feeding: a review and clinical aspects. J Clin Psychopharmacol. 2005;25:59–73.
Abdullah H, Beckmann J, Andonian-Dierks C. Empirical findings on associations between anxiety, depression, and congenital heart disease in adults – a systematic review and meta-analysis. Heart Mind. 2023;7:70–9.
Munir LZ, du Toit EF. Impact of chronic psychological stress on cardiovascular disease risk: a narrative review. Heart Mind. 2024;8:268–78.
Meunier MR, Bennett IM, Coco AS. Use of antidepressant medication in the United States during pregnancy, 2002–2010. Psychiatr Serv. 2013;64:1157–60.
Damkier P, Christensen LS, Broe A. Patterns and predictors for prescription of psychotropics and mood-stabilizing antiepileptics during pregnancy in Denmark 2000–2016. Br J Clin Pharmacol. 2018;84:2651–62.
Latendresse G, Elmore C, Deneris A. Selective serotonin reuptake inhibitors as first-line antidepressant therapy for perinatal depression. J Midwifery Womens Health. 2017;62:317–28.
Bałkowiec-Iskra E, Mirowska-Guzel DM, Wielgoś M. Effect of antidepressants use in pregnancy on foetus development and adverse effects in newborns. Ginekol Pol. 2017;88:36–42.
Mesches GA, Wisner KL, Betcher HK. A common clinical conundrum: antidepressant treatment of depression in pregnant women. Semin Perinatol. 2020;44:151229.
Vlenterie R, van Gelder M, Anderson HR, Andersson L, Broekman BFP, Dubnov-Raz G, et al. Associations between maternal depression, antidepressant use during pregnancy, and adverse pregnancy outcomes: an individual participant data meta-analysis. Obstet Gynecol. 2021;138:633–46.
Ghimire U, Papabathini SS, Kawuki J, Obore N, Musa TH. Depression during pregnancy and the risk of low birth weight, preterm birth and intrauterine growth restriction- an updated meta-analysis. Early Hum Dev. 2021;152:105243.
Guan HB, Wei Y, Wang LL, Qiao C, Liu CX. Prenatal selective serotonin reuptake inhibitor use and associated risk for gestational hypertension and preeclampsia: a Meta-analysis of Cohort studies. J Womens Health (Larchmt). 2018;27:791–800.
Arafa A, Dong JY. Depression and risk of gestational diabetes: a meta-analysis of cohort studies. Diabetes Res Clin Pract. 2019;156:107826.
Leshem R, Bar-Oz B, Diav-Citrin O, Gbaly S, Soliman J, Renoux C, et al. Selective Serotonin Reuptake Inhibitors (SSRIs) and Serotonin Norepinephrine ReuptakeInhibitors (SNRIs) During Pregnancy and the Risk for Autism Spectrum Disorder (ASD) and Attention Deficit Hyperactivity Disorder (ADHD) in the offspring: a true effect or a bias? A systematic review & meta-analysis. Curr Neuropharmacol. 2021;19:896–906.
Jarde A, Morais M, Kingston D, Giallo R, MacQueen GM, Giglia L, et al. Neonatal outcomes in women with untreated antenatal depression compared with women without depression: a systematic review and meta-analysis. JAMA Psychiatry. 2016;73:826–37.
Uguz F. Neonatal and childhood outcomes in offspring of oregnant women using antidepressant medications: a critical review of current meta-analyses. J Clin Pharmacol. 2021;61:146–58.
Dragioti E, Solmi M, Favaro A, Fusar-Poli P, Dazzan P, Thompson T, et al. Association of antidepressant use with adverse health outcomes: a systematic umbrella review. JAMA Psychiatry. 2019;76:1241–55.
Ankarfeldt MZ, Petersen J, Andersen JT, Fernandes MFS, Li H, Motsko SP, et al. Duloxetine exposure during pregnancy and the risk of spontaneous and elective abortion: a Danish Nationwide Observational study. Drugs Real World Outcomes. 2021;8:289–99.
Berard A, Zhao JP, Sheehy O. Antidepressant use during pregnancy and the risk of major congenital malformations in a cohort of depressed pregnant women: an updated analysis of the Quebec Pregnancy Cohort. BMJ Open. 2017;7:e013372.
Reis M, Kallen B. Delivery outcome after maternal use of antidepressant drugs in pregnancy: an update using Swedish data. Psychol Med. 2010;40:1723–33.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–5.
Adeoye IA, Unogu CO, Adediran K, Gbadebo BM. Determinants of adverse perinatal outcomes in Ibadan, Nigeria: the influence of maternal lifestyle. PLOS Glob Public Health. 2025;5:e0004199.
Al Rawahi A, Al Kiyumi MH, Al Kimyani R, Al-Lawati I, Murthi S, Davidson R, et al. The effect of antepartum depression on the outcomes of pregnancy and development of postpartum depression: a Prospective Cohort study of Omani women. Sultan Qaboos Univ Med J. 2020;20:e179–86.
Avalos LA, Chandran A, Churchill ML, Gao X, Ames JL, Nozadi SS, et al. Prenatal depression and risk of child autism-related traits among participants in the Environmental influences on Child Health Outcomes program. Autism Res. 2023;16:1825–35.
Beyene GM, Azale T, Gelaye KA, Ayele TA. The effect of antenatal depression on birth weight among newborns in South Gondar zone, Northwest Ethiopia: a Population-Based Prospective Cohort study. Arch Public Health. 2021;79:121.
Bindt C, Guo N, Bonle MT, Appiah-Poku J, Hinz R, Barthel D, et al. No association between antenatal common mental disorders in low-obstetric risk women and adverse birth outcomes in their offspring: results from the CDS study in Ghana and Cote D’Ivoire. PloS one. 2013;8:e80711.
Bitew T, Hanlon C, Kebede E, Honikman S, Fekadu A. Antenatal depressive symptoms and perinatal complications: a Prospective study in rural Ethiopia. BMC psychiatry. 2017;17:301.
Björvang RD, Liakea I, Carpentsier B, Kozinszky Z, Skalkidou A, Fransson E. Association of diabetes mellitus in pregnancy and perinatal depression. Psychosom Med. 2024;86:52–8.
Chang HY, Keyes KM, Lee KS, Choi IA, Kim SJ, Kim KW, et al. Prenatal maternal depression is associated with low birth weight through shorter gestational age in term infants in Korea. Early Hum Dev. 2014;90:15–20.
Chen XN, Hu Y, Hu WH, Xia X, Li XT. Risk of adverse perinatal outcomes and antenatal depression based on the zung self-rating depression scale. Rep Dev Med. 2021;5:23–9.
Chung TK, Lau TK, Yip AS, Chiu HF, Lee DT. Antepartum depressive symptomatology is associated with adverse obstetric and neonatal outcomes. Psychosom Med. 2001;63:830–4.
Dadi AF, Miller ER, Woodman RJ, Azale T, Mwanri L. Effect of antenatal depression on adverse birth outcomes in Gondar town, Ethiopia: a Community-Based Cohort study. PloS one. 2020;15:e0234728.
Dahlen HG, Barnett B, Kohlhoff J, Drum ME, Munoz AM, Thornton C. Obstetric and psychosocial risk factors for Australian-born and non-Australian born women and associated pregnancy and birth outcomes: a Population Based Cohort study. BMC Pregnancy Childbirth. 2015;15:292.
Dayan J, Creveuil C, Marks MN, Conroy S, Herlicoviez M, Dreyfus M, et al. Prenatal depression, prenatal anxiety, and spontaneous preterm birth: a Prospective Cohort study among women with early and regular care. Psychosom Med. 2006;68:938–46.
Diego MA, Field T, Hernandez-Reif M, Schanberg S, Kuhn C, Gonzalez-Quintero VH. Prenatal depression restricts fetal growth. Early Hum Dev. 2009;85:65–70.
Dole N, Savitz DA, Hertz-Picciotto I, Siega-Riz AM, McMahon MJ, Buekens P. Maternal stress and preterm birth. Am J Epidemiol. 2003;157:14–24.
Dowse E, Chan S, Ebert L, Wynne O, Thomas S, Jones D, et al. Impact of perinatal depression and anxiety on birth outcomes: a retrospective data analysis. Matern Child Health J. 2020;24:718–26.
Evans J, Heron J, Patel RR, Wiles N. Depressive symptoms during pregnancy and low birth weight at term: Longitudinal study. Br J Psychiatry. 2007;191:84–5.
Fransson E, Ortenstrand A, Hjelmstedt A. Antenatal depressive symptoms and preterm birth: a Prospective study of a Swedish national sample. Birth. 2011;38:10–6.
Gavin AR, Holzman C, Siefert K, Tian Y. Maternal depressive symptoms, depression, and psychiatric medication use in relation to risk of preterm delivery. Womens Health Issues. 2009;19:325–34.
Giurgescu C, Engeland CG, Templin TN. Symptoms of depression predict negative birth outcomes in African American women: a Pilot Study. J Midwifery Womens Health. 2015;60:570–7.
Giurgescu C, Fahmy L, Slaughter-Acey J, Nowak A, Caldwell C, Misra DP. Can support from the father of the baby buffer the adverse effects of depressive symptoms on risk of Preterm birth in black families? AIMS Public Health. 2018;5:89–98.
Goedhart G, Snijders AC, Hesselink AE, van Poppel MN, Bonsel GJ, Vrijkotte TG. Maternal depressive symptoms in relation to perinatal mortality and morbidity: results from a Large Multiethnic Cohort study. Psychosom Med. 2010;72:769–76.
Hemavathy S, Deepa M, Uma R, Gowri R, Pradeepa R, Hannah W, et al. Prevalence of depression and anxiety among pregnant women with gestational diabetes mellitus in South Asia. Prim Care Diabetes. 2025;19:322–8.
Ibanez G, Charles MA, Forhan A, Magnin G, Thiebaugeorges O, Kaminski M, et al. Depression and anxiety in women during pregnancy and neonatal outcome: data from the EDEN mother-child cohort. Early Hum Dev. 2012;88:643–9.
Kabir K, Sheeder J, Stevens-Simon C. Depression, weight gain, and low birth weight adolescent delivery: do somatic symptoms strengthen or weaken the relationship? J Pediatr Adolesc Gynecol. 2008;21:335–42.
Karim S, Cai B, Merchant AT, Wilcox S, Zhao X, Alston K, et al. Antenatal depressive symptoms and adverse birth outcomes in healthy start participants: the modifying role of utilization of mental health services. Midwifery. 2024;132:103985.
Khanam R, Applegate J, Nisar I, Dutta A, Rahman S, Nizar A, et al. Burden and risk factors for antenatal depression and its effect on preterm birth in South Asia: a Population-Based Cohort study. PloS one. 2022;17:e0263091.
Kim DR, Sockol LE, Sammel MD, Kelly C, Moseley M, Epperson CN. Elevated risk of adverse obstetric outcomes in pregnant women with depression. Arch Womens Ment Health. 2013;16:475–82.
Kurki T, Hiilesmaa V, Raitasalo R, Mattila H, Ylikorkala O. Depression and anxiety in early pregnancy and risk for preeclampsia. Obstet Gynecol. 2000;95:487–90.
Lalani S, Premji SS, Shaikh K, Sulaiman S, Yim IS, Forcheh N, et al. Individual and collective contribution of antenatal psychosocial distress conditions and preterm birth in Pakistani women. PLoS One. 2023;18:e0282582.
Larsen A, Pintye J, Abuna F, Bhat A, Dettinger JC, Gomez L, et al. Risks of adverse perinatal outcomes in relation to maternal depressive symptoms: a Prospective Cohort study in Kenya. Paediatr Perinat Epidemiol. 2023;37:489–504.
Li D, Liu L, Odouli R. Presence of depressive symptoms during early pregnancy and the risk of preterm delivery: a Prospective Cohort study. Hum Reprod. 2009;24:146–53.
Li J, Fan W, Wang X, Hou X, Chen Z, Lv M. Mental health in early pregnancy and spontaneous abortion risk: a Prospective Cohort Study. Alpha Psychiatry. 2024;25:648–55.
Li X, Gao R, Dai X, Liu H, Zhang J, Liu X, et al. The association between symptoms of depression during pregnancy and low birth weight: a Prospective study. BMC Pregnancy Childbirth. 2020;20:147.
Li Y, Chang JJ, Zuo R, Xian H, Scharff D. The moderating role of depression in the association between hypertension during pregnancy and birth outcomes. Hypertens Pregnancy. 2023;42:2226703.
Liu Y, Murphy SK, Murtha AP, Fuemmeler BF, Schildkraut J, Huang Z, et al. Depression in pregnancy, infant birth weight and DNA methylation of imprint regulatory elements. Epigenetics. 2012;7:735–46.
López DP, Serna LG, Arnáiz MCS, Ruiz MO, Viladegut JS, Sol J, et al. Outcomes of antenatal depression in women and the new-born: a Retrospective Cohort study. Family Practice. 2024;41:925–31.
Luciano M, Di Vincenzo M, Brandi C, Tretola L, Toricco R, Perris F, et al. Does antenatal depression predict post-partum depression and obstetric complications? Results from a Longitudinal, Long-term, Real-world study. Front Psychiatry. 2022;13:1082762.
Misra D, Strobino D, Trabert B. Effects of social and psychosocial factors on risk of preterm birth in black women. Paediatr Perinat Epidemiol. 2010;24:546–54.
Mochache K, Mathai M, Gachuno O, Vander Stoep A, Kumar M. Depression during pregnancy and preterm delivery: a Prospective Cohort study among women attending antenatal clinic at Pumwani Maternity Hospital. Ann Gen Psychiatry. 2018;17:31.
Morrison C, McCook JG, Bailey BA. First trimester depression scores predict development of gestational diabetes mellitus in pregnant rural Appalachian women. J Psychosom Obstet Gynaecol. 2016;37:21–5.
Nasreen HE, Pasi HB, Rifin SM, Aris MAM, Rahman JA, Rus RM, et al. Impact of maternal antepartum depressive and anxiety symptoms on birth outcomes and mode of delivery: a Prospective Cohort study in east and west coasts of Malaysia. BMC Pregnancy Childbirth. 2019;19:201.
Navaratne P, Foo XY, Kumar S. Impact of a high Edinburgh Postnatal Depression Scale score on obstetric and perinatal outcomes. Sci Rep. 2016;6:33544.
Ncube CN, Enquobahrie DA, Gavin AR. Racial differences in the association between maternal antenatal depression and Preterm birth risk: a Prospective Cohort study. J Womens Health (Larchmt). 2017;26:1312–8.
Netsi E, Coll CVN, Stein A, Silveira MF, Bertoldi AD, Bassani DG, et al. Female infants are more susceptible to the effects of maternal antenatal depression; findings from the Pelotas (Brazil) Birth Cohort study. J Affect Disord. 2020;267:315–24.
Nidey NL, Momany AM, Strathearn L, Carter KD, Wehby GL, Bao W, et al. Association between perinatal depression and risk of attention deficit hyperactivity disorder among children: a retrospective cohort study. Ann Epidemio. 2021;63:1–6.
Pan J, Zhu X, Xu L, Zhou L, Yin S, Qi X, et al. Effects of sleep quality, anxiety, and depression on miscarriage among pregnant women: a multi-center prospective observational study. Transl Psychiatry. 2025;15:131.
Pathirana MM, Andraweera PH, Leemaqz S, Aldridge E, Arstall MA, Dekker GA, et al. Anxiety and depression in early gestation and the association with subsequent gestational diabetes mellitus in a disadvantaged population. Matern Child Health J. 2023;27:2185–93.
Pawlby S, Hay DF, Sharp D, Waters CS, O’Keane V. Antenatal depression predicts depression in adolescent offspring: prospective Longitudinal Community-Based study. J Affect Disord. 2009;113:236–43.
Pearson RM, Evans J, Kounali D, Lewis G, Heron J, Ramchandani PG, et al. Maternal depression during pregnancy and the postnatal period: risks and possible mechanisms for offspring depression at age 18 years. JAMA Psychiatry. 2013;70:1312–9.
Rahman A, Bunn J, Lovel H, Creed F. Association between antenatal depression and low birthweight in a developing country. Acta Psychiatr Scand. 2007;115:481–6.
Roy U, Swain D. A prospective cohort study to assess the prevalence and risk factors of antepartum depression and its effect on maternal and fetal outcome. Asian J Psychiatr. 2024;91:103873.
Saeed A, Raana T, Saeed AM, Humayun A. Effect of antenatal depression on maternal dietary intake and neonatal outcome: a prospective cohort. Nutr J. 2016;15:64.
Shuffrey LC, Lucchini M, Morales S, Sania A, Hockett C, Barrett E, et al. Gestational diabetes mellitus, prenatal maternal depression, and risk for postpartum depression: an Environmental influences on Child Health Outcomes (ECHO) study. BMC Pregnancy Childbirth. 2022;22:758.
Stark EL, Shim J, Ross CM, Miller ES. The association between positive antenatal depression screening and breastfeeding initiation and continuation. Am J Perinatol. 2021;38:171–5.
Steer RA, Scholl TO, Hediger ML, Fischer RL. Self-reported depression and negative pregnancy outcomes. J Clin Epidemiol. 1992;45:1093–9.
Straub H, Adams M, Kim JJ, Silver RK. Antenatal depressive symptoms increase the likelihood of preterm birth. Am J Obstet Gynecol. 2012;207:329.e1–4.
Thombre MK, Talge NM, Holzman C. Association between pre-pregnancy depression/anxiety symptoms and hypertensive disorders of pregnancy. J Womens Health (Larchmt). 2015;24:228–36.
Van Ngo T, Gammeltoft T, Nguyen HTT, Meyrowitsch DW, Rasch V. Antenatal depressive symptoms and adverse birth outcomes in Hanoi, Vietnam. PLoS One. 2018;13:e0206650.
Venkataraman R, Yadav SK, Pukale RS. Factors affecting the depression and impact of depression on maternal outcomes: a Prospective Observational study from a rural tertiary care South Indian Hospital. Ital J Gynaecol Obstet. 2023;35:406–14.
Venkatesh KK, Riley L, Castro VM, Perlis RH, Kaimal AJ. Association of antenatal depression symptoms and antidepressant treatment with Preterm birth. Obstet Gynecol. 2016;127:926–33.
Versteegen M, Bozlak CT, Larkin H, Appleton AA. Maternal depression, adverse childhood experiences, and social support in relation to gestational diabetes risk: results from the Albany Infant and Mother Study (AIMS). BMC Pregnancy Childbirth. 2021;21:335.
Wado YD, Afework MF, Hindin MJ. Effects of maternal pregnancy intention, depressive symptoms and social support on risk of low birth weight: a Prospective study from southwestern Ethiopia. PLoS One. 2014;9:e96304.
Weobong B, ten Asbroek AH, Soremekun S, Manu AA, Owusu-Agyei S, Prince M, et al. Association of antenatal depression with adverse consequences for the mother and newborn in rural Ghana: findings from the DON Population-Based Cohort study. PLoS One. 2014;9:e116333.
Yang J, Xu A, Zhang Y, Deng J, Lin X, Xie L, et al. Promoter methylation changes in the placenta involved in the relationship between prenatal depression and small for gestational age. BMC Pregnancy Childbirth. 2022;22:741.
Zhang ZY, Yu JJ, Zeng WT, Zhou MC, Duan CC, Zhu LL. Association between antenatal depression and adverse perinatal outcomes: a Prospective Cohort study. J Affect Disord. 2023;323:490–5.
Aliaga A, Cunillera O, Amador MDC, Aliaga M, Arquerons M, Almeda J. Association between affective disorders presenting before and during pregnancy and pre-term birth, considering socio-demographic factors, obstetric factors, health conditions, and use of medication. Aten Primaria. 2019;51:626–36.
Andersen JT, Andersen NL, Horwitz H, Poulsen HE, Jimenez-Solem E. Exposure to selective serotonin reuptake inhibitors in early pregnancy and the risk of miscarriage. Obstet Gynecol. 2014;124:655–61.
Andrade SE, McPhillips H, Loren D, Raebel MA, Lane K, Livingston J, et al. Antidepressant medication use and risk of persistent pulmonary hypertension of the newborn. Pharmacoepidemiol Drug Saf. 2009;18:246–52.
Ankarfeldt MZ, Petersen J, Andersen JT, Li H, Motsko SP, Fast T, et al. Exposure to duloxetine during pregnancy and risk of congenital malformations and stillbirth: a Nationwide Cohort study in Denmark and Sweden. PLoS Med. 2021;18:e1003851.
Ankarfeldt MZ, Petersen J, Andersen JT, Fernandes MFS, Li H, Motsko SP, et al. Duloxetine exposure during pregnancy and the risk of offspring being born small for gestational age or prematurely: a Nationwide Danish and Swedish Safety study. Drugs - Real World Outcomes. 2023;10:69–81.
Berard A, Sheehy O, Zhao JP, Vinet E, Bernatsky S, Abrahamowicz M. SSRI and SNRI use during pregnancy and the risk of persistent pulmonary hypertension of the newborn. B J Clin Pharmacol. 2017;83:1126–33.
Bliddal M, Wesselhoeft R, Strandberg-Larsen K, Ernst MT, Weissman MM, Gingrich JA, et al. Prenatal antidepressant exposure and emotional disorders until age 22: a Danish Register study. Child Adolesc Psychiatry Ment Health. 2023;17:73.
Boukhris T, Sheehy O, Berard A. Antidepressant use in pregnancy and the risk of attention deficit with or without hyperactivity disorder in children. Paediatr Perinat Epidemiol. 2017;31:363–73.
Boukhris T, Sheehy O, Mottron L, Berard A. Antidepressant use during pregnancy and the risk of autism spectrum disorder in children. JAMA Pediatr. 2016;170:117–24.
Brown HK, Ray JG, Wilton AS, Lunsky Y, Gomes T, Vigod SN. Association between serotonergic antidepressant use during pregnancy and autism spectrum disorder in children. JAMA. 2017;317:1544–52.
Calderon-Margalit R, Qiu C, Ornoy A, Siscovick DS, Williams MA. Risk of preterm delivery and other adverse perinatal outcomes in relation to maternal use of psychotropic medications during pregnancy. Am J Obstet Gynecol. 2009;201:579.e1–8.
Cantarutti A, Merlino L, Monzani E, Giaquinto C, Corrao G. Is the risk of preterm birth and low birth weight affected by the use of antidepressant agents during pregnancy? A population-based investigation. PLoS One. 2016;11:e0168115.
Chan JKN, Lee KCK, Wong CSM, Chang WC. Prenatal antidepressant use and risk of congenital malformations: a Population-Based Cohort study. Psychiatry Res. 2024;339:116038.
Chen LF, Lin CE, Chung CH, Lai CH, Chien WC. Association between the use of antidepressants and the risk of preterm birth among pregnant women with depression: a Retrospective Cohort study in Taiwan. J Investig Med. 2021;69:999–1007.
Colvin L, Slack-Smith L, Stanley FJ, Bower C. Dispensing patterns and pregnancy outcomes for women dispensed selective serotonin reuptake inhibitors in pregnancy. Birth Defects Res A Clin Mol Teratol. 2011;91:142–52.
Davis RL, Rubanowice D, McPhillips H, Raebel MA, Andrade SE, Smith D, et al. Risks of congenital malformations and perinatal events among infants exposed to antidepressant medications during pregnancy. Pharmacoepidemiol Drug Saf. 2007;16:1086–94.
Esen BO, Ehrenstein V, Sørensen HT, Laugesen K, Pedersen L. Prenatal antidepressant exposure and the risk of attention-deficit/hyperactivity disorder in childhood: a Cohort study with triangulation. Epidemiology. 2022;33:581–92.
Furu K, Kieler H, Haglund B, Engeland A, Selmer R, Stephansson O, et al. Selective serotonin reuptake inhibitors and venlafaxine in early pregnancy and risk of birth defects: Population Based Cohort study and sibling design. BMJ. 2015;350:h1798.
Grzeskowiak LE, Gilbert AL, Morrison JL. Neonatal outcomes after late-gestation exposure to selective serotonin reuptake inhibitors. J Clin Psychopharmacol. 2012;32:615–21.
Grzeskowiak LE, McBain R, Dekker GA, Clifton VL. Antidepressant use in late gestation and risk of postpartum haemorrhage: a Retrospective Cohort study. BJOG. 2016;123:1929–36.
Hanley GE, Smolina K, Mintzes B, Oberlander TF, Morgan SG. Postpartum hemorrhage and use of serotonin reuptake inhibitor antidepressants in pregnancy. Obstet Gynecol. 2016;27:553–61.
Heller HM, Ravelli ACJ, Bruning AHL, de Groot CJM, Scheele F, van Pampus MG, et al. Increased postpartum haemorrhage, the possible relation with serotonergic and other psychopharmacological drugs: a Matched Cohort study. BMC Pregnancy Childbirth. 2017;17:166.
Heuvelman H, Davies NM, Ben-Shlomo Y, Emond A, Evans J, Gunnell D, et al. Antidepressants in pregnancy: applying causal epidemiological methods to understand service-use outcomes in women and long-term neurodevelopmental outcomes in exposed children. Health Technol Assess. 2023;27:1–83.
Hutchison SM, Brain U, Grunau RE, Kuzeljevic B, Irvine M, Mâsse LC, et al. Associations between maternal depressive symptoms and selective serotonin reuptake inhibitor antidepressant treatment on internalising and anxiety behaviours in children: 12-year Longitudinal study. BJPsych Open. 2023;9:e26.
Huybrechts KF, Bateman BT, Palmsten K, Desai RJ, Patorno E, Gopalakrishnan C, et al. Antidepressant use late in pregnancy and risk of persistent pulmonary hypertension of the newborn. JAMA. 2015;313:2142–51.
Huybrechts KF, Bateman BT, Pawar A, Bessette LG, Mogun H, Levin R, et al. Maternal and fetal outcomes following exposure to duloxetine in pregnancy: Cohort study. BMJ. 2020;368:m237.
Hwang YM, Roper RT, Piekos SN, Enquobahrie DA, Hebert MF, Paquette AG, et al. Timing of selective serotonin reuptake inhibitor use and risk for preterm birth and related adverse events: with a consideration of the COVID-19 pandemic period. J Matern Fetal Neonatal Med. 2024;37:2313364.
Jimenez-Solem E, Andersen JT, Petersen M, Broedbaek K, Lander AR, Afzal S, et al. SSRI use during pregnancy and risk of stillbirth and neonatal mortality. Am J Psychiatry. 2013;170:299–304.
Jordan S, Morris JK, Davies GI, Tucker D, Thayer DS, Luteijn JM, et al. Selective Serotonin Reuptake Inhibitor (SSRI) antidepressants in pregnancy and congenital anomalies: analysis of linked databases in wales, Norway and Funen, Denmark. PLoS One. 2016;11:e0165122.
Kieler H, Artama M, Engeland A, Ericsson O, Furu K, Gissler M, et al. Selective serotonin reuptake inhibitors during pregnancy and risk of persistent pulmonary hypertension in the newborn: Population Based Cohort study from the five Nordic countries. BMJ. 2012;344:d8012.
Kim DR, Pinheiro E, Luther JF, Eng HF, Dills JL, Wisniewski SR, et al. Is third trimester serotonin reuptake inhibitor use associated with postpartum hemorrhage? J Psychiatr Res. 2016;73:79–85.
Kivisto J, Lehto SM, Halonen K, Georgiadis L, Heinonen S. Maternal use of selective serotonin reuptake inhibitors and lengthening of the umbilical cord: indirect evidence of increased foetal activity-a Retrospective Cohort study. PLoS One. 2016;11:e0154628.
Kolding L, Ehrenstein V, Pedersen L, Sandager P, Petersen OB, Uldbjerg N, et al. Antidepressant use in pregnancy and severe cardiac malformations: Danish register-based study. BJOG. 2021;128:1949–57.
Laine MK, Masalin S, Rono K, Kautiainen H, Gissler M, Pennanen P, et al. Risk of preterm birth in primiparous women with exposure to antidepressant medication before pregnancy and/or during pregnancy - impact of body mass index. Ann Med. 2019;51:51–7.
Laugesen K, Olsen MS, Telen Andersen AB, Froslev T, Sorensen HT. In utero exposure to antidepressant drugs and risk of attention deficit hyperactivity disorder: a nationwide Danish Cohort study. BMJ Open. 2013;3:e003507.
Lee KCK, Fung VSC, Chan JKN, Wong CSM, Cheung KW, Seto MTY, et al. Antidepressant use during pregnancy and risk of obstetrics and neonatal outcomes: a Propensity Score-Weighted Population-Based Cohort study in 2003–2018. Eur Neuropsychopharmacol. 2025;96:36–45.
Lee MJ, Chen YL, Wu SI, Huang CW, Dewey ME, Chen VC. Association between maternal antidepressant use during pregnancy and the risk of autism spectrum disorder and attention deficit hyperactivity disorder in offspring. Eur Child Adolesc Psychiatry. 2024;33:4273–83.
Leibovitch L, Rymer-Haskel N, Schushan-Eisen I, Kuint J, Strauss T, Maayan-Metzger A. Short-term neonatal outcome among term infants after in utero exposure to serotonin reuptake inhibitors. Neonatology. 2013;104:65–70.
Lindqvist PG, Nasiell J, Gustafsson LL, Nordstrom L. Selective serotonin reuptake inhibitor use during pregnancy increases the risk of postpartum hemorrhage and anemia: a Hospital-Based Cohort study. J Thromb Haemost. 2014;12:1986–92.
Lund N, Pedersen LH, Henriksen TB. Selective serotonin reuptake inhibitor exposure in utero and pregnancy outcomes. Arch Pediatr Adolesc Med. 2009;163:949–54.
Lupattelli A, Barone-Adesi F, Nordeng H. Association between antidepressant use in pregnancy and gestational diabetes mellitus: results from the Norwegian Mother, Father and Child Cohort study. Pharmacoepidemiol Drug Saf. 2022;31:247–56.
Lupattelli A, Wood M, Lapane K, Spigset O, Nordeng H. Risk of preeclampsia after gestational exposure to selective serotonin reuptake inhibitors and other antidepressants: a study from The Norwegian Mother and Child Cohort study. Pharmacoepidemiol Drug Saf. 2017;26:1266–76.
Malm H, Artama M, Gissler M, Ritvanen A. Selective serotonin reuptake inhibitors and risk for major congenital anomalies. Obstet Gynecol. 2011;118:111–20.
Malm H, Brown AS, Gissler M, Gyllenberg D, Hinkka-Yli-Salomaki S, McKeague IW, et al. Gestational exposure to selective serotonin reuptake inhibitors and offspring psychiatric disorders: a National Register-Based study. J Am Acad Child Adolesc Psychiatry. 2016;55:359–66.
Malm H, Sourander A, Gissler M, Gyllenberg D, Hinkka-Yli-Salomäki S, McKeague IW, et al. Pregnancy complications following prenatal exposure to SSRIs or maternal psychiatric disorders: results from Population-Based National Register data. Am J Psychiatry. 2015;172:1224–32.
Man KKC, Chan EW, Ip P, Coghill D, Simonoff E, Chan PKL, et al. Prenatal antidepressant use and risk of attention-deficit/hyperactivity disorder in offspring: Population Based Cohort study. BMJ. 2017;357:j2350.
Mao Y, Pedersen LH, Christensen J, Vestergaard M, Zhou W, Olsen J, et al. Prenatal exposure to antidepressants and risk of epilepsy in childhood. Pharmacoepidemiol Drug Saf. 2016;25:1320–30.
Nishigori H, Obara T, Nishigori T, Mizuno S, Metoki H, Hoshiai T, et al. Selective serotonin reuptake inhibitors and risk of major congenital anomalies for pregnancies in Japan: a Nationwide Birth Cohort study of the Japan Environment and Children’s study. Congenit Anom (Kyoto). 2017;57:72–8.
Norby U, Forsberg L, Wide K, Sjors G, Winbladh B, Kallen K. Neonatal morbidity after maternal use of antidepressant drugs during pregnancy. Pediatrics. 2016;138:e20160181.
Nordeng H, van Gelder MM, Spigset O, Koren G, Einarson A, Eberhard-Gran M. Pregnancy outcome after exposure to antidepressants and the role of maternal depression: results from the Norwegian Mother and Child Cohort study. J Clin psychopharmacol. 2012;32:186–94.
Oberlander TF, Warburton W, Misri S, Riggs W, Aghajanian J, Hertzman C. Major congenital malformations following prenatal exposure to serotonin reuptake inhibitors and benzodiazepines using population-based health data. Birth Defects Res B Dev Reprod Toxicol. 2008;83:68–76.
Öndemark M, Nordström L, Lindqvist PG. Dose-dependent increase in risk of bleeding and bleeding complications in relation to SSRI use at delivery. Eur J Obstet Gynecol Reprod Biol. 2024;296:265–9.
Ostenfeld A, Petersen TS, Pedersen LH, Westergaard HB, Løkkegaard ECL, Andersen JT. Mirtazapine exposure in pregnancy and fetal safety: a Nationwide Cohort study. Acta Psychiatr Scand. 2022;145:557–67.
Palmsten K, Chambers CD, Wells A, Bandoli G. Patterns of prenatal antidepressant exposure and risk of preeclampsia and postpartum haemorrhage. Paediatr Perinat Epidemiol. 2020;34:597–606.
Palmsten K, Hernández-Díaz S, Huybrechts KF, Williams PL, Michels KB, Achtyes ED, et al. Use of antidepressants near delivery and risk of postpartum hemorrhage: Cohort study of low income women in the United States. BMJ. 2013;347:f4877.
Palmsten K, Huybrechts KF, Michels KB, Williams PL, Mogun H, Setoguchi S, et al. Antidepressant use and risk for preeclampsia. Epidemiology. 2013;24:682–91.
Palmsten K, Setoguchi S, Margulis AV, Patrick AR, Hernandez-Diaz S. Elevated risk of preeclampsia in pregnant women with depression: depression or antidepressants? Am J Epidemiol. 2012;175:988–97.
Rai D, Lee BK, Dalman C, Newschaffer C, Lewis G, Magnusson C. Antidepressants during pregnancy and autism in offspring: population Based Cohort study. BMJ. 2017;358:j2811.
Skalkidou A, Sundström-Poromaa I, Wikman A, Hesselman S, Wikström AK, Elenis E. SSRI use during pregnancy and risk for postpartum haemorrhage: a National Register-Based Cohort study in Sweden. BJOG. 2020;127:1366–73.
Skurtveit S, Selmer R, Tverdal A, Furu K, Nystad W, Handal M. Drug exposure: inclusion of dispensed drugs before pregnancy may lead to underestimation of risk associations. J Clin Epidemiol. 2013;66:964–72.
Sørensen MJ, Grønborg TK, Christensen J, Parner ET, Vestergaard M, Schendel D, et al. Antidepressant exposure in pregnancy and risk of autism spectrum disorders. Clin Epidemiol. 2013;5:449–59.
Stephansson O, Kieler H, Haglund B, Artama M, Engeland A, Furu K, et al. Selective serotonin reuptake inhibitors during pregnancy and risk of stillbirth and infant mortality. JAMA. 2013;309:48–54.
Suarez EA, Bateman BT, Hernández-Díaz S, Straub L, Wisner KL, Gray KJ, et al. Association of antidepressant use during pregnancy with risk of neurodevelopmental disorders in children. JAMA Intern Med. 2022;182:1149–60.
Sujan AC, Rickert ME, Oberg AS, Quinn PD, Hernandez-Diaz S, Almqvist C, et al. Associations of maternal antidepressant use during the first trimester of pregnancy with Preterm birth, small for gestational age, autism spectrum disorder, and attention-deficit/hyperactivity disorder in offspring. JAMA. 2017;317:1553–62.
Toh S, Mitchell AA, Louik C, Werler MM, Chambers CD, Hernandez-Diaz S. Selective serotonin reuptake inhibitor use and risk of gestational hypertension. Am J Psychiatry. 2009;166:320–8.
Tran YH, Huynh HK, Faas MM, de Vos S, Groen H. Antidepressant use during pregnancy and development of preeclampsia: a focus on classes of action and specific transporters/receptors targeted by antidepressants. J Psychiatr Res. 2022;146:92–101.
Ulbrich KA, Zumpf K, Ciolino JD, Shah M, Miller ES, Wisner KL. Acute delivery room resuscitation of neonates exposed to selective serotonin reuptake inhibitors. J Pediatr. 2021;232:103–8.
Vasilakis-Scaramozza C, Aschengrau A, Cabral H, Jick SS. Antidepressant use during early pregnancy and the risk of congenital anomalies. Pharmacotherapy. 2013;33:693–700.
Vignato JA, Gumusoglu SB, Davis HA, Scroggins SM, Hamilton WS, Brandt DS, et al. Selective serotonin reuptake inhibitor use in pregnancy and protective mechanisms in preeclampsia. Reprod Sci. 2023;30:701–12.
Wen SW, Yang Q, Garner P, Fraser W, Olatunbosun O, Nimrod C, et al. Selective serotonin reuptake inhibitors and adverse pregnancy outcomes. Am J Obstet Gynecol. 2006;194:961–6.
Wichman CL, Moore KM, Lang TR, St Sauver JL, Heise RH Jr, Watson WJ. Congenital heart disease associated with selective serotonin reuptake inhibitor use during pregnancy. Mayo Clin Proc. 2009;84:23–7.
Wiggs KK, Sujan AC, Rickert ME, Quinn PD, Larsson H, Lichtenstein P, et al. Maternal serotonergic antidepressant use in pregnancy and risk of seizures in children. Neurology. 2022;98:e2329–36.
Wu P, Velez Edwards DR, Gorrindo P, Sundermann AC, Torstenson ES, Jones SH, et al. Association between first trimester antidepressant use and risk of spontaneous abortion. Pharmacotherapy. 2019;39:889–98.
Yamamoto-Sasaki M, Yoshida S, Takeuchi M, Tanaka-Mizuno S, Ogawa Y, Furukawa TA, et al. Association between antidepressant use during pregnancy and autism spectrum disorder in children: a Retrospective Cohort study based on Japanese claims data. Matern Health Neonatol Perinatol. 2019;5:1.
Zakiyah N, Ter Heijne LF, Bos JH, Hak E, Postma MJ, Schuiling-Veninga CCM. Antidepressant use during pregnancy and the risk of developing gestational hypertension: a Retrospective Cohort study. BMC Pregnancy Childbirth. 2018;18:187.
Zeskind PS, Stephens LE. Maternal selective serotonin reuptake inhibitor use during pregnancy and newborn neurobehavior. Pediatrics. 2004;113:368–75.
Adhikari K, Patten SB, Lee S, Metcalfe A. Risk of adverse perinatal outcomes among women with pharmacologically treated and untreated depression during pregnancy: a Retrospective Cohort study. Paediatr Perinat Epidemiol. 2019;33:323–31.
Avalos LA, Chen H, Li DK. Antidepressant medication use, depression, and the risk of preeclampsia. CNS Spectr. 2015;20:39–47.
Ban L, Gibson JE, West J, Fiaschi L, Sokal R, Smeeth L, et al. Maternal depression, antidepressant prescriptions, and congenital anomaly risk in offspring: a Population-Based Cohort study. BJOG. 2014;121:1471–81.
Beck-Pancer D, Aghaee S, Swint A, Acker J, Deardorff J, Kubo A. Maternal depression and antidepressant use during pregnancy and associations with depressive symptoms and suicidality in adolescent children. Clin Epidemiol. 2023;15:613–28.
Cheng CC, Siong K, Lee HC, Kau Y. Effect of depressive disorders and other psychiatric disorders on pregnancy and perinatal outcomes in a Hong Kong obstetrics unit. Hong Kong J Gynaecol Obstet Midwifery. 2020;20:22–6.
El Marroun H, Jaddoe VW, Hudziak JJ, Roza SJ, Steegers EA, Hofman A, et al. Maternal use of selective serotonin reuptake inhibitors, fetal growth, and risk of adverse birth outcomes. Arch Gen Psychiatry. 2012;69:706–14.
Engelstad HJ, Roghair RD, Calarge CA, Colaizy TT, Stuart S, Haskell SE. Perinatal outcomes of pregnancies complicated by maternal depression with or without selective serotonin reuptake inhibitor therapy. Neonatology. 2014;105:149–54.
Hagberg KW, Robijn AL, Jick S. Maternal depression and antidepressant use during pregnancy and the risk of autism spectrum disorder in offspring. Clin Epidemiol. 2018;10:1599–612.
Herrero T, Driebe A, Fratto V, Hamlin A, Lacoursiere DY, Ramos GA. Positive antenatal Edinburgh Depression Scale: examining behavioral and pharmacological therapy on maternal and neonatal outcomes. J Matern Fetal Neonatal Med. 2020;33:212–6.
Huang HC, Sung FC, Chen PC, Chang CY, Muo CH, Shiue HS, et al. Obstetric outcomes in pregnant women with and without depression: population-based comparison. Sci Rep. 2017;7:13937.
Jensen HM, Gron R, Lidegaard O, Pedersen LH, Andersen PK, Kessing LV. Maternal depression, antidepressant use in pregnancy and Apgar scores in infants. Br J Psychiatry. 2013;202:347–51.
Jensen HM, Gron R, Lidegaard O, Pedersen LH, Andersen PK, Kessing LV. The effects of maternal depression and use of antidepressants during pregnancy on risk of a child small for gestational age. Psychopharmacology (Berl). 2013;228:199–205.
Jordan S, Davies GI, Thayer DS, Tucker D, Humphreys I. Antidepressant prescriptions, discontinuation, depression and perinatal outcomes, including breastfeeding: a population cohort analysis. PLoS One. 2019;14:e0225133.
Kjaersgaard MI, Parner ET, Vestergaard M, Sorensen MJ, Olsen J, Christensen J, et al. Prenatal antidepressant exposure and risk of spontaneous abortion - a Population-Based study. PLoS One. 2013;8:e72095.
Michihata N, Shigemi D, Yamana H, Matsui H, Jo T, Yasunaga H. Safety of Japanese herbal Kampo medicines for the treatment of depression during pregnancy. Int J Gynaecol Obstet. 2022;159:865–9.
Oberlander TF, Warburton W, Misri S, Aghajanian J, Hertzman C. Neonatal outcomes after prenatal exposure to selective serotonin reuptake inhibitor antidepressants and maternal depression using population-based linked health data. Arch Gen Psychiatry. 2006;63:898–906.
Sahingoz M, Yuksel G, Karsidag C, Uguz F, Sonmez EO, Annagur BB, et al. Birth weight and preterm birth in babies of pregnant women with major depression in relation to treatment with antidepressants. J Clin Psychopharmacol. 2014;34:226–9.
Seebeck J, Sznajder KK, Kjerulff KH. The association between prenatal psychosocial factors and autism spectrum disorder in offspring at 3 years: a Prospective Cohort study. Soc Psychiatry Psychiatr Epidemiol. 2024;59:1639–49.
Suri R, Altshuler L, Hellemann G, Burt VK, Aquino A, Mintz J. Effects of antenatal depression and antidepressant treatment on gestational age at birth and risk of preterm birth. Am J Psychiatry. 2007;164:1206–13.
Watson SJ, Spigset O. Depression and antidepressant treatment in the development of hypertensive disorders of pregnancy: results from a Prospective Cohort study. Aust N Z J Psychiatry. 2023;57:520–7.
Wisner KL, Sit DK, Hanusa BH, Moses-Kolko EL, Bogen DL, Hunker DF, et al. Major depression and antidepressant treatment: impact on pregnancy and neonatal outcomes. Am J Psychiatry. 2009;166:557–66.
Kautzky A, Slamanig R, Unger A, Höflich A. Neonatal outcome and adaption after in utero exposure to antidepressants: a systematic review and meta-analysis. Acta Psychiatr Scand. 2022;145:6–28.
Cornet MC, Wu YW, Forquer H, Avalos LA, Sriram A, Scheffler AW, et al. Maternal treatment with selective serotonin reuptake inhibitors during pregnancy and delayed neonatal adaptation: a Population-Based Cohort study. Arch Dis Child Fetal Neonatal Ed. 2024;109:294–300.
MacQueen GM, Frey BN, Ismail Z, Jaworska N, Steiner M, Lieshout RJ, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) 2016 clinical guidelines for the management of adults with major depressive disorder: section 6. Special Populations: Youth, Women, and the Elderly. Can J Psychiatry. 2016;61:588–603.
Eke AC, Saccone G, Berghella V. Selective serotonin reuptake inhibitor (SSRI) use during pregnancy and risk of preterm birth: a systematic review and meta-analysis. BJOG. 2016;123:1900–7.
Roubinov D, Don B, Blades R, Epel E. Is it me or my child? The association between maternal depression and children’s behavior problems in mothers and their children with or without autism. Fam Process. 2023;62:737–53.
Glover V. Maternal depression, anxiety and stress during pregnancy and child outcome; what needs to be done. Best Pract Res Clin Obstet Gynaecol. 2014;28:25–35.
Hu R, Li Y, Zhang Z, Yan W. Antenatal depressive symptoms and the risk of preeclampsia or operative deliveries: a meta-analysis. PLoS One. 2015;10:e0119018.
Liu M. Potenitial risk factors of cardiovascular diseases and mental disorders. Heart Mind. 2023;7:55–6.
Clark H, Khosla R. The partnership for maternal, newborn, and child health: 2026–30 strategy. Lancet. 2025;406:596–7.
Carlini SV, Deligiannidis KM. Poor neonatal adaptation syndrome: toward a clinical consensus to guide research and counseling. Acta Psychiatr Scand. 2022;145:3–5.
Acknowledgements
This study was supported by a grant from the National Programs for Brain Science and Brain-like Intelligence Technology of China (STI2030-Major Projects, 2021ZD0200800, 2021ZD0200700, 2021ZD0202100), and the National Natural Science Foundation of China (no. 82288101, 82171514, 82471550), the Natural Science Foundation of Beijing Municipality of China (M23013), and National Key Research and Development Program of China (2024YFC2707801). The authors declare that the research was conducted in the absence of any commercial or financial relationship that could be constructed as a potential conflict of interests.
Author contributors
Liu T, Zeng N, and Xu Y contributed equally to this article. Lu L, BaoY and Shi J proposed the topic and main idea. Liu T, Zeng N, and Xu Y were responsible for the literature search and study selection. Liu TT, Zeng N, Xu Y, Fan T, Wang F, Liu C, Zhao Y, Ni S, Mei H, Wu S were responsible for the data extraction and quality assessment. Liu T and Xu Y wrote the initial draft. Liu T, Zeng N, Xu Y, Zhang X, Wang YX, Wang YM, Li S, Shi J, Lu L and Bao Y commented on and revised the manuscript. Lu L, Shi J, and Bao Y made the final version. All authors contributed to the final draft of the manuscript.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Comprting interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, T., Zeng, N., Xu, Y. et al. Depression and antidepressant use in pregnancy and adverse maternal and offspring outcomes: a systematic review and meta-analysis. Mol Psychiatry 30, 6033–6044 (2025). https://doi.org/10.1038/s41380-025-03263-y
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41380-025-03263-y
This article is cited by
-
Comprehensive clinical outcomes of TiRobot-assisted minimally invasive surgery for pelvic fractures: a meta-analysis
Journal of Robotic Surgery (2026)