Abstract
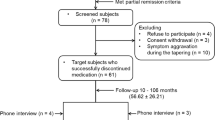
Although some studies have suggested that relapse may be associated with antipsychotic treatment resistance in schizophrenia, the number and quality of studies is limited. The current analysis included patients with a diagnosis of first-episode schizophrenia or schizoaffective disorder who met the following criteria: (1) referral to the First-Episode Psychosis Program between 2003 and 2013; (2) treatment with an oral second-generation antipsychotic according to a standardized treatment algorithm; (3) positive symptom remission; (4) subsequent relapse (i.e., second episode) in association with non-adherence; and (5) reintroduction of antipsychotic treatment with the same agent used to achieve response in the first episode. The following outcomes were used as an index of antipsychotic treatment response: changes in the brief psychiatric rating scale (BPRS) total and positive symptom scores and number of patients who achieved positive symptom remission and 20 and 50% response. A total of 130 patients were included in the analyses. Although all patients took the same antipsychotic in both episodes, there were significant episode-by-time interactions for all outcomes of antipsychotic treatment response over 1 year in favor of the first episode compared to the second episode (50% response rate: 48.7 vs. 10.4% at week 7; 88.2 vs. 27.8% at week 27, respectively). Although antipsychotic doses in the second episode were significantly higher than those in the first episode, results remained unchanged after adjusting for antipsychotic dose. The present findings suggest that antipsychotic treatment response is reduced or delayed in the face of relapse following effective treatment of the first episode of schizophrenia.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Pennington M, McCrone P. The cost of relapse in schizophrenia. Pharmacoeconomics. 2017;35:921–36.
Leucht S, Tardy M, Komossa K, Heres S, Kissling W, Salanti G, et al. Antipsychotic drugs versus placebo for relapse prevention in schizophrenia: a systematic review and meta-analysis. Lancet. 2012;379:2063–71.
Sendt K-V, Tracy DK, Bhattacharyya S. A systematic review of factors influencing adherence to antipsychotic medication in schizophrenia-spectrum disorders. Psychiatry Res. 2015;225:14–30.
Mojtabai R, Lavelle J, Gibson PJ, Sohler NL, Craig TJ, Carlson GA, et al. Gaps in use of antipsychotics after discharge by first-admission patients with schizophrenia, 1989 to 1996. Psychiatr Serv. 2002;53:337–9.
Higashi K, Medic G, Littlewood KJ, Diez T, Granström O, Hert M, De. Medication adherence in schizophrenia: factors influencing adherence and consequences of nonadherence, a systematic literature review. Ther Adv Psychopharmacol. 2013;3:200–18.
Leucht S, Leucht C, Huhn M, Chaimani A, Mavridis D, Helfer B, et al. Sixty years of placebo-controlled antipsychotic drug trials in acute schizophrenia: systematic review, bayesian meta-analysis, and meta-regression of efficacy predictors. Am J Psychiatry. 2017;174:927–42.
Zhu Y, Li C, Huhn M, Rothe P, Krause M, Bighelli I, et al. How well do patients with a first episode of schizophrenia respond to antipsychotics: a systematic review and meta-analysis. Eur Neuropsychopharmacol. 2017;27:835–44.
Keating D, McWilliams S, Schneider I, Hynes C, Cousins G, Strawbridge J, et al. Pharmacological guidelines for schizophrenia: a systematic review and comparison of recommendations for the first episode. BMJ Open. 2017;7:e013881.
Wiersma D, Nienhuis FJ, Slooff CJ, Giel R. Natural course of schizophrenic disorders: a 15-year followup of a Dutch incidence cohort. Schizophr Bull. 1998;24:75–85.
Emsley R, Chiliza B, Asmal L. The evidence for illness progression after relapse in schizophrenia. Schizophr Res. 2013a;148:117–21.
Lieberman J, Alvir JM, Koreen A, Geisler S, Chakos M, Sheitman B, et al. Psychobiologic correlates of treatment response in schizophrenia. Neuropsychopharmacology. 1996;14:13S–21S.
Emsley R, Oosthuizen P, Koen L, Niehaus D, Martinez L. Comparison of treatment response in second-episode versus first-episode schizophrenia. J Clin Psychopharmacol. 2013b;33:80–3.
Emsley R, Nuamah I, Hough D, Gopal S. Treatment response after relapse in a placebo-controlled maintenance trial in schizophrenia. Schizophr Res. 2012;138:29–34.
American Psychiatric Association. DSM-IV-TR. Diagnostic Stat Man Ment Disord 4th Ed TR. 2000
Guy W. ECDEU Assessment Manual for Psychopharmacology. US Dep Heal Educ Welf Publ ADM 76-338. Rockville, MD: National Institute of Mental Health; 1976.
Overall JE, Gorham DR. The brief psychiatric rating scale. Psychol Rep. 1962;10:799–812.
Leucht S, Kissling W, Davis JM. The PANSS should be rescaled. Schizophr Bull. 2010;36:461–2.
Obermeier M, Mayr A, Schennach-Wolff R, Seemüller F, Möller H-J, Riedel M. Should the PANSS be rescaled? Schizophr Bull. 2010;36:455–60.
Leucht S, Kane JM, Kissling W, Hamann J, Etschel E, Engel RR. What does the PANSS mean? Schizophr Res. 2005;79:231–8.
Leucht S, Samara M, Heres S, Patel MX, Woods SW, Davis JM. Dose equivalents for second-generation antipsychotics: the minimum effective dose method. Schizophr Bull. 2014;40:314–26.
Lally J, Ajnakina O, Di Forti M, Trotta A, Demjaha A, Kolliakou A, et al. Two distinct patterns of treatment resistance: clinical predictors of treatment resistance in first-episode schizophrenia spectrum psychoses. Psychol Med. 2016;46:3231–40.
Demjaha A, Lappin JM, Stahl D, Patel MX, MacCabe JH, Howes OD, et al. Antipsychotic treatment resistance in first-episode psychosis: prevalence, subtypes and predictors. Psychol Med. 2017;47:1981–9.
Mena C, Gonzalez-Valderrama A, Iruretagoyena B, Undurraga J, Crossley NA. Early treatment resistance in a Latin-American cohort of patients with schizophrenia. Schizophr Res. 2018;199:380–5.
Howes OD, McCutcheon R, Agid O, Bartolomeis A, de, Beveren NJM, van, Birnbaum ML, et al. Treatment-resistant schizophrenia: Treatment Response and Resistance in Psychosis (TRRIP) Working Group Consensus Guidelines on Diagnosis and Terminology. Am J Psychiatry. 2017;174:216–29.
Goff DC, Falkai P, Fleischhacker WW, Girgis RR, Kahn RM, Uchida H, et al. The long-term effects of antipsychotic medication on clinical course in schizophrenia. Am J Psychiatry. 2017;174:840–9.
Correll CU, Rubio JM, Kane JM. What is the risk-benefit ratio of long-term antipsychotic treatment in people with schizophrenia? World Psychiatry. 2018;17:149–60.
Kishimoto T, Robenzadeh A, Leucht C, Leucht S, Watanabe K, Mimura M, et al. Long-acting injectable vs oral antipsychotics for relapse prevention in schizophrenia: a meta-analysis of randomized. Trials . 2014;40:192–213.
Ostuzzi G, Bighelli I, So R, Furukawa TA, Barbui C. Does formulation matter? A systematic review and meta-analysis of oral versus long-acting antipsychotic studies. Schizophr Res. 2017;183:10–21.
Kishimoto T, Nitta M, Borenstein M, Kane JM, Correll CU. Long-acting injectable versus oral antipsychotics in schizophrenia: a systematic review and meta-analysis of mirror-image studies. J Clin Psychiatry. 2013;74:957–65.
Kishimoto T, Hagi K, Nitta M, Leucht S, Olfson M, Kane JM, et al. Effectiveness of long-acting injectable vs oral antipsychotics in patients with schizophrenia: a meta-analysis of prospective and retrospective cohort studies. Schizophr Bull. 2018;44:603–19.
Weiden PJ, Kim E, Bermak J, Turkoz I, Gopal S, Berwaerts J. Does half-life matter after antipsychotic discontinuation? A relapse comparison in schizophrenia with 3 different formulations of paliperidone. J Clin Psychiatry. 2017;78:e813–20.
Rund BR. Does active psychosis cause neurobiological pathology? A critical review of the neurotoxicity hypothesis. Psychol Med. 2014;44:1577–90.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Takeuchi, H., Siu, C., Remington, G. et al. Does relapse contribute to treatment resistance? Antipsychotic response in first- vs. second-episode schizophrenia. Neuropsychopharmacol. 44, 1036–1042 (2019). https://doi.org/10.1038/s41386-018-0278-3
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41386-018-0278-3
This article is cited by
-
Transdiagnostic stage-based monitoring of public mental health
Nature Reviews Psychology (2026)
-
Effects of Long-Term Treatment with TV-46000 on Symptom Improvement Over Time in Stabilized Patients with Schizophrenia
CNS Drugs (2026)
-
Relapse and associated factors among psychiatric patients in Africa: a systematic review and meta-analysis
BMC Psychiatry (2025)
-
Schizophrenia
Nature Reviews Disease Primers (2025)
-
Efficacy of identifying Treatment-Resistant and non-Treatment-Resistant Schizophrenia using niacin skin flushing response combined with clinical feature
Schizophrenia (2025)