Abstract
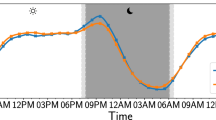
Attention deficit hyperactivity disorder (ADHD) is a common neuropsychiatric condition that has been strongly associated with changes in sleep and circadian rhythms. Circadian rhythms are near 24-h cycles that are primarily generated by an endogenous circadian timekeeping system, encoded at the molecular level by a panel of clock genes. Stimulant and non-stimulant medication used in the management of ADHD has been shown to potentially impact on circadian processes and their behavioral outputs. In the current study, we have analyzed circadian rhythms in daily activity and sleep, and the circadian gene expression in a cohort of healthy controls (N = 22), ADHD participants not using ADHD-medication (N = 17), and participants with ADHD and current use of ADHD medication (N = 17). Rhythms of sleep/wake behavior were assessed via wrist-worn actigraphy, whilst rhythms of circadian gene expression were assessed ex-vivo in primary human-derived dermal fibroblast cultures. Behavioral data indicate that patients with ADHD using ADHD-medication have lower relative amplitudes of diurnal activity rhythms, lower sleep efficiency, more nocturnal activity but not more nocturnal wakenings than both controls and ADHD participants without medication. At the molecular level, there were alterations in the expression of PER2 and CRY1 between ADHD individuals with no medication compared to medicated ADHD patients or controls, whilst CLOCK expression was altered in patients with ADHD and current medication. Analysis of fibroblasts transfected with a BMAL1:luc reporter showed changes in the timing of the peak expression across the three groups. Taken together, these data support the contention that both ADHD and medication status impact on circadian processes.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Willcutt EG. The prevalence of DSM-IV attention-deficit/hyperactivity disorder: a meta-analytic review. Neurotherapeutics. 2012;9:490–9. https://doi.org/10.1007/s13311-012-0135-8
Sibley MH, Mitchell JT, Becker SP. Method of adult diagnosis influences estimated persistence of childhood ADHD: a systematic review of longitudinal studies. Lancet Psychiatry. 2016;3:1157–65. https://doi.org/10.1016/S2215-0366(16)30190-0
Brevik EJ, Lundervold AJ, Halmøy A, Posserud M-B, Instanes JT, Bjorvatn B, et al. Prevalence and clinical correlates of insomnia in adults with attention-deficit hyperactivity disorder. Acta Psychiatr Scand. 2017;136:220–7. https://doi.org/10.1111/acps.12756
Hennig T, Krkovic K, Lincoln TM. What predicts inattention in adolescents? An experience-sampling study comparing chronotype, subjective, and objective sleep parameters. Sleep Med. 2017;38:58–63. https://doi.org/10.1016/j.sleep.2017.07.009
Logan RW, Hasler BP, Forbes EE, Franzen PL, Torregrossa MM, Huang YH, et al., et al. Impact of sleep and circadian rhythms on addiction vulnerability in adolescents. Biol Psychiatry. 2018;83:987–96. https://doi.org/10.1016/j.biopsych.2017.11.035
McGowan NM, Coogan AN. Sleep and circadian rhythm function and trait impulsivity: an actigraphy study. Psychiatry Res. 2018;268:251–6. https://doi.org/10.1016/j.psychres.2018.07.030
Wynchank D, Bijlenga D, Beekman AT, Kooij JJS, Penninx BW. Adult attention-deficit/hyperactivity disorder (ADHD) and insomnia: an update of the literature. Curr Psychiatry Rep. 2017;19:98 https://doi.org/10.1007/s11920-017-0860-0
Krause AJ, Simon EB, Mander BA, Greer SM, Saletin JM, Goldstein-Piekarski AN, et al. The sleep-deprived human brain. Nat Rev Neurosci. 2017;18:404 https://doi.org/10.1038/nrn.2017.55
Scammell TE, Arrigoni E, Lipton J. Neural circuitry of wakefulness and sleep. Neuron. 2017;93:747–65. https://doi.org/10.1016/j.neuron.2017.01.014
Borbély AA, Daan S, Wirz-Justice A, Deboer T. The two-process model of sleep regulation: a reappraisal. J Sleep Res. 2016;25:131–43. https://doi.org/10.1111/jsr.12371
Pilorz V, Helfrich-Förster C, Oster H. The role of the circadian clock system in physiology. Pflügers Arch. 2018;470:227–39. https://doi.org/10.1007/s00424-017-2103-y
Takahashi JS. Transcriptional architecture of the mammalian circadian clock. Nat Rev Genet. 2017;18:164–79. https://doi.org/10.1038/nrg.2016.150
Zhang R, Lahens NF, Ballance HI, Hughes ME, Hogenesch JB. A circadian gene expression atlas in mammals: implications for biology and medicine. Proc Natl Acad Sci USA. 2014;111:16219–24. https://doi.org/10.1073/pnas.1408886111.
Hughes S, Jagannath A, Hankins MW, Foster RG, Peirson SN. Chapter Six—photic regulation of clock systems. In: Sehgal A, editor. Methods in enzymology, vol. 552. Academic Press, London; 2015. p. 125–43. https://doi.org/10.1016/bs.mie.2014.10.018.
Zaki NFW, Spence DW, BaHammam AS, Pandi-Perumal SR, Cardinali DP, Brown GM. Chronobiological theories of mood disorder. Eur Arch Psychiatry Clin Neurosci. 2018;268:107–18. https://doi.org/10.1007/s00406-017-0835-5
Coogan AN, McGowan NM. A systematic review of circadian function, chronotype and chronotherapy in attention deficit hyperactivity disorder. Atten Defic Hyperact Disord. 2017;9:129–47. https://doi.org/10.1007/s12402-016-0214-5
Baird AL, Coogan AN, Siddiqui A, Donev RM, Thome J. Adult attention-deficit hyperactivity disorder is associated with alterations in circadian rhythms at the behavioural, endocrine and molecular levels. Mol Psychiatry. 2012;17:988–95. https://doi.org/10.1038/mp.2011.149
Rybak YE, McNeely HE, Mackenzie BE, Jain UR, Levitan RD. Seasonality and circadian preference in adult attention-deficit/hyperactivity disorder: clinical and neuropsychological correlates. Compr Psychiatry. 2007;48:562–71. https://doi.org/10.1016/j.comppsych.2007.05.008
Van Veen MM, Kooij JJS, Boonstra AM, Gordijn MCM, Van Someren EJW. Delayed circadian rhythm in adults with attention-deficit/hyperactivity disorder and chronic sleep-onset insomnia. Biol Psychiatry. 2010;67:1091–6. https://doi.org/10.1016/j.biopsych.2009.12.032
Santhi N, Lazar AS, McCabe PJ, Lo JC, Groeger JA, Dijk D-J. Sex differences in the circadian regulation of sleep and waking cognition in humans Proc Natl Acad Sci USA. 2016;113:E2730–9. https://doi.org/10.1073/pnas.1521637113.
Antle MC, van Diepen HC, Deboer T, Pedram P, Pereira RR, Meijer JH. Methylphenidate modifies the motion of the circadian clock. Neuropsychopharmacology. 2012;37:2446 https://doi.org/10.1038/npp.2012.103
O'Keeffe SM, Thome J, Coogan AN. The noradrenaline reuptake inhibitor atomoxetine phase-shifts the circadian clock in mice. Neuroscience. 2012;201:219–30. https://doi.org/10.1016/j.neuroscience.2011.11.002
Baird AL, Coogan AN, Kaufling J, Barrot M, Thome J. Daily methylphenidate and atomoxetine treatment impacts on clock gene protein expression in the mouse brain. Brain Res. 2013;1513:61–71. https://doi.org/10.1016/j.brainres.2013.03.038
Mendoza J, van Diepen HC, Pereira RR, Meijer JH. Time-shifting effects of methylphenidate on daily rhythms in the diurnal rodent Arvicanthis ansorgei. Psychopharmacology. 2018;235:2323–33. https://doi.org/10.1007/s00213-018-4928-2
Morash-Conway J, Gendron M, Corkum P. The role of sleep quality and quantity in moderating the effectiveness of medication in the treatment of children with ADHD. Atten Defic Hyperact Disord. 2017;9:31–8. https://doi.org/10.1007/s12402-016-0204-7
Takashima, A. Establishment of Fibroblast Cultures. Current Protocols, 1999;1:2.1.1–2.1.12
Kushida CA, Chang A, Gadkary C, Guilleminault C, Carrillo O, Dement WC. Comparison of actigraphic, polysomnographic, and subjective assessment of sleep parameters in sleep-disordered patients. Sleep Med. 2001;2:389–96. https://doi.org/10.1016/S1389-9457(00)00098-8
Tsang AH, Sanchez-Moreno C, Bode B, Rossner MJ, Garaulet M, Oster H. Tissue-specific interaction of Per1/2 and Dec2 in the regulation of fibroblast circadian rhythms. J Biol Rhythms. 2012;27:478–89. https://doi.org/10.1177/0748730412462838
Hida A, Ohsawa Y, Kitamura S, Nakazaki K, Ayabe N, Motomura Y, et al. Evaluation of circadian phenotypes utilizing fibroblasts from patients with circadian rhythm sleep disorders. Transl Psychiatry. 2017;7:e1106 https://doi.org/10.1038/tp.2017.75
O'Keeffe SM, Beynon AL, Davies J, Moynagh PN, Coogan AN. NF-kB signalling is involved in immune-modulation, but not basal functioning of the mouse suprachiasmatic circadian clock. Eur J Neurosci. 2017;45:1111–23.
Cohen J. Statistical power analysis for the behavioral sciences. Taylor and Francis, New York; 1988.
Boonstra AM, Kooij JJ, Oosterlaan J, Sergeant JA, Buitelaar JK, Van Someren EJ. Hyperactive night and day? Actigraphy studies in adult ADHD: a baseline comparison and the effect of methylphenidate. Sleep. 2007;30:433–42.
Trinh T, Kohllepin S, Yang PB, Burau KD, Dafny N. Adult female rats altered diurnal locomotor activity pattern following chronic methylphenidate treatment. J Neural Transm. 2013;120:1717–31. https://doi.org/10.1007/s00702-013-1063-4
McGowan NM, Brannigan R, Doyle D, Coogan AN. Diurnal preference, circadian phase of entrainment and time perspectives: just what are the relationships? Pers Indiv Differ. 2017;112:79–84. https://doi.org/10.1016/j.paid.2017.02.051
Brown SA, Fleury-Olela F, Nagoshi E, Hauser C, Juge C, Meier CA, et al. The period length of fibroblast circadian gene expression varies widely among human individuals. PLoS Biol. 2005;3:e338 https://doi.org/10.1371/journal.pbio.0030338
McCarthy MJ, Wei H, Marnoy Z, Darvish RM, McPhie DL, Cohen BM, et al. Genetic and clinical factors predict lithium's effects on PER2 gene expression rhythms in cells from bipolar disorder patients. Transl Psychiatry. 2013;3:e318 https://doi.org/10.1038/tp.2013.90
Johansson A-S, Owe-Larsson B, Hetta J, Lundkvist GB. Altered circadian clock gene expression in patients with schizophrenia. Schizophr Res. 2016;174:17–23. https://doi.org/10.1016/j.schres.2016.04.029
Johansson J, Landgren M, Fernell E, Vumma R, Åhlin A, Bjerkenstedt L, et al. Altered tryptophan and alanine transport in fibroblasts from boys with attention-deficit/hyperactivity disorder (ADHD): an in vitro study. Behav Brain Funct. 2011;7:40. https://doi.org/10.1186/1744-9081-7-40
Csoka AB, Szyf M. Epigenetic side-effects of common pharmaceuticals: a potential new field in medicine and pharmacology. Med Hypotheses. 2009;73:770–80. https://doi.org/10.1016/j.mehy.2008.10.039
Ding K, Yang J, Reynolds GP, Chen B, Shao J, Liu R, et al. DAT1 methylation is associated with methylphenidate response on oppositional and hyperactive-impulsive symptoms in children and adolescents with ADHD. World J Biol Psychiatry. 2017;18:291–9. https://doi.org/10.1080/15622975.2016.1224928
Ozburn AR, Purohit K, Parekh PK, Kaplan GN, Falcon E, Mukherjee S, et al. Functional implications of the CLOCK 3111T/C single-nucleotide polymorphism. Front Psychiatry. 2016;7:67 https://doi.org/10.3389/fpsyt.2016.00067
Kissling C, Retz W, Wiemann S, Coogan AN, Clement RM, Hünnerkopf R, et al. A polymorphism at the 3'-untranslated region of the CLOCK gene is associated with adult attention-deficit hyperactivity disorder. Am J Med Genet B Neuropsychiatr Genet. 2008;147:333–8. https://doi.org/10.1002/ajmg.b.30602
Xu X, Breen G, Chen C-K, Huang Y-S, Wu Y-Y, Asherson P. Association study between a polymorphism at the 3'-untranslated region of CLOCK gene and attention deficit hyperactivity disorder. Behav Brain Funct. 2010;6:48. https://doi.org/10.1186/1744-9081-6-48
Jeong SH, Yu J-C, Lee CH, Choi K-S, Choi J-E, Kim SH, et al. Human CLOCK gene-associated attention deficit hyperactivity disorder-related features in healthy adults: quantitative association study using Wender Utah Rating Scale. Eur Arch Psychiatry Clin Neurosci. 2014;264:71–81. https://doi.org/10.1007/s00406-013-0443-y
Mendoza J, Challet E. Circadian insights into dopamine mechanisms. Neuroscience. 2014;282:230–42. https://doi.org/10.1016/j.neuroscience.2014.07.081
Taneja R, Hunter K, Burakgazi-Dalkilic E, Carran M. Effect of sleep patterns on levetiracetam induced mood changes. Epilepsy Behav. 2017;75:237–40. https://doi.org/10.1016/j.yebeh.2017.07.038
Freeman D, Sheaves B, Goodwin GM, Yu LM, Nickless A, Harrison PJ. The effects of improving sleep on mental health (OASIS): a randomised controlled trial with mediation analysis. Lancet Psychiatry. 2017;4:749–58. https://doi.org/10.1016/S2215-0366(17)30328-0
Jansson-Fröjmark M, Norell-Clarke A. Cognitive behavioural therapy for insomnia in psychiatric disorders current. Sleep Med Rep. 2016;2:233–40. https://doi.org/10.1007/s40675-016-0055-y
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Coogan, A.N., Schenk, M., Palm, D. et al. Impact of adult attention deficit hyperactivity disorder and medication status on sleep/wake behavior and molecular circadian rhythms. Neuropsychopharmacol. 44, 1198–1206 (2019). https://doi.org/10.1038/s41386-019-0327-6
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41386-019-0327-6
This article is cited by
-
The link between Wnt-related, stress-related, and circadian genes in the dermal fibroblasts of individuals with attention-deficit hyperactivity disorder
Journal of Neural Transmission (2025)
-
Novel non-stimulants rescue hyperactive phenotype in an adgrl3.1 mutant zebrafish model of ADHD
Neuropsychopharmacology (2023)
-
Personalizing atomoxetine dosing in children with ADHD: what can we learn from current supporting evidence
European Journal of Clinical Pharmacology (2023)
-
Understanding the Impact of Stimulants on Sleep in ADHD: Evidence from Systematic Assessment of Sleep in Adults
CNS Drugs (2022)
-
Relevance of Objective Measures in Psychiatric Disorders—Rest-Activity Rhythm and Psychophysiological Measures
Current Psychiatry Reports (2021)