Abstract
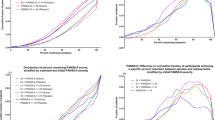
Differences in efficacy between antipsychotics and placebo in schizophrenia trials have decreased over the past decades. Previous studies have tried to identify potential explanatory factors focusing on response to placebo; however, it is still not clear which factors, if any, specifically moderate drug-response, as they may be different from those moderating placebo-response. Therefore, in this meta-regression analysis we explore whether there is an interaction between drug-response and placebo-response in terms of effect size. We systematically searched multiple electronic databases, ClinicalTrials.gov, and the US Food and Drug Administration website for randomized, placebo-controlled trials investigating the efficacy of antipsychotics in patients with acute schizophrenia (last update: October 2016). The main outcome was the change on the Brief Psychiatric Rating Scale or the Positive and Negative Syndrome Scale score from baseline to endpoint after at least 3 weeks of treatment. Multiple patient-, design-, and drug-related potential predictors of response were analyzed by meta-regressions, as predefined in the study protocol. Overall, 167 trials with 28,102 participants were included. Publication year, the number of participants and sites, mean dose, minimum severity threshold as an inclusion criterion, chronicity, industry sponsorship, type of rating scale, diagnostic criteria, and number of medications had a different impact on drug and placebo response. By contrast, baseline severity, duration of wash-out, study duration, and study region affected drug and placebo response in a similar way without a net effect on effect sizes. No other factors had a significant effect on either drug-response or placebo-response. In conclusion, as individual moderators may have different impact on placebo-response and drug-response, it is important to consider also the specific factors influencing drug-response in order to fully understand the difference between antipsychotics and placebo. These results shed further light on the phenomenon of decreasing effect size of antipsychotics for schizophrenia over time and should help design future randomized controlled trials in the field (Prospero registration number CRD42013003342).
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Leucht S, Leucht C, Huhn M, Chaimani A, Mavridis D, Helfer B, et al. Sixty years of placebo-controlled antipsychotic drug trials in acute schizophrenia: systematic review, bayesian meta-analysis, and meta-regression of efficacy predictors. Am J Psychiatry. 2017;174:appiajp201716121358.
Study 049. A 6-week, double-blind, randomized, fixed dose, parallel-group study of the efficacy and safety of three dose levels of SM-13496 (lurasidone) compared to placebo and haloperidol in patients with schizophrenia who are experiencing an acute exacerbation of symptoms. Center for drug evaluation and research. Application number 200603 Medical review(s) http://www.fgagov. 2010.
Leucht S, Chaimani A, Leucht C, Huhn M, Mavridis D, Helfer B, et al. 60years of placebo-controlled antipsychotic drug trials in acute schizophrenia: Meta-regression of predictors of placebo response. Schizophr Res. 2018;201:315–23.
Mallinckrodt CH, Zhang L, Prucka WR, Millen BA. Signal detection and placebo response in schizophrenia: parallels with depression. Psychopharmacol Bull. 2010;43:53–74.
Agid O, Siu CO, Potkin SG, Kapur S, Watsky E, Vanderburg D, et al. Meta-regression analysis of placebo response in antipsychotic trials, 1970-2010. Am J Psychiatry. 2013;170:1335–44.
Rutherford BR, Pott E, Tandler JM, Wall MM, Roose SP, Lieberman JA. Placebo response in antipsychotic clinical trials: a meta-analysis. JAMA psychiatry. 2014;71:1409–21.
Kirsch I. Are drug and placebo effects in depression additive? Biol Psychiatry. 2000;47:733–5.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6:e1000100.
Carpenter WT, Buchanan RW. Schizophrenia. N Eng J Med. 1994;330:681–90.
Leucht S, Tardy M, Komossa K, Heres S, Kissling W, Salanti G, et al. Antipsychotic drugs versus placebo for relapse prevention in schizophrenia: a systematic review and meta-analysis. Lancet. 2012;379:2063–71.
Leucht S, Cipriani A, Spineli L, Mavridis D, Orey D, Richter F, et al. Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: a multiple-treatments meta-analysis. Lancet. 2013;382:951–62.
Honigfeld G. Clozapine: antipsychotic activity in treatment-resistant schizophrenics. Adv Ther. 1984;1:77–97.
Samara MT, Cao H, Helfer B, Davis JM, Leucht S. Chlorpromazine versus every other antipsychotic for schizophrenia: a systematic review and meta-analysis challenging the dogma of equal efficacy of antipsychotic drugs. Eur Neuropsychopharmacol: J Eur Coll Neuropsychopharmacol. 2014;24:1046–55.
Hartling L, Abou-Setta AM, Dursun S, Mousavi SS, Pasichnyk D, Newton AS. Antipsychotics in adults with schizophrenia: comparative effectiveness of first-generation versus second-generation medications: a systematic review and meta-analysis. Ann Intern Med. 2012;157:498–511.
Dold M, Samara MT, Li C, Tardy M, Leucht S. Haloperidol versus first-generation antipsychotics for the treatment of schizophrenia and other psychotic disorders. Cochrane Database Syst Rev. 2015;1:CD009831.
McMahon RP, Kelly DL, Boggs DL, Li L, Hu Q, Davis JM, et al. Feasibility of reducing the duration of placebo-controlled trials in schizophrenia research. Schizophr Bull. 2008;34:292–301.
Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions version 5.1.0 [updated March 2011]. Chichester, UK: Wiley and Sons; 2011.
Wu TX, Li YP, Liu GJ, Bian Z, Li J, Zhang J, et al. Investigation of authenticity of ‘claimed’ randomized controlled trials (RCTs) and quality assessment of RCT reports published in China. Presented at the XIV Cochrane Colloquium, Dublin, Ireland, October 23–26; 2006.
Woodhead M. 80% of China’s clinical trial data are fraudulent, investigation finds. BMJ. 2016;355:i5396.
Adams CE, Coutinho E, Davis JM, Duggan L, Essali A, Fenton M, et al. The cochrane library. Chichester, UK: John Wiley & Sons Ltd; 2011.
Klein DF, Davis JM. Diagnosis and drug treatment of psychiatric disorders. Baltimore: Williams and Wilkins; 1969.
Adams CE, Awad G, Rathbone J. Chlorpromazine versus placebo for schizophrenia. Cochrane Database Syst Rev. 2007;Art. No.: CD000284.
Joy CB, Adams CE, Laurie S. Haloperidol versus placebo for schizophrenia. Cochrane Database Syst Rev. 2007;Art. No.: CD003082.
Shen X, Xia J, Adams CE. Flupenthixol versus placebo for schizophrenia. Cochrane Database Syst Rev. 2012;11:CD009777.
Matar HE, Almerie MQ. Oral fluphenazine versus placebo for schizophrenia. Cochrane Database Syst Rev. 2007;24:CD006352.
Hartung B, Wada M, Laux G, Leucht S. Perphenazine for schizophrenia. Cochrane Database Syst Rev. 2005:CD003443.
Omori IM, Wang J. Sulpiride versus placebo for schizophrenia. Cochrane Database Syst Rev. 2009:CD007811.
Fenton M, Rathbone J, Reilly J, Sultana A. Thioridazine for schizophrenia. Cochrane Database Syst Rev. 2007;6:CD001944.
Leucht S, Arbter D, Engel RR, Kissling W, Davis JM. How effective are second-generation antipsychotic drugs? A meta-analysis of placebo-controlled trials. MolPsychiatry. 2009;14:429–47.
Kay SR, Fiszbein A. The positive and negative symptome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13:261–75.
Overall JE, Gorham DR. The brief psychiatric rating scale. Psychol Rep. 1962;10:790–812.
Leucht S, Rothe P, Davis JM, Engel RR. Equipercentile linking of the BPRS and the PANSS. Eur Neuropsychopharmacol: J Eur Coll Neuropsychopharmacol. 2013;23:956–9.
Leon AC, Mallinckrodt CH, Chuang-Stein C, Archibald DG, Archer GE, Chartier K. Attrition in randomized controlled clinical trials: methodological issues in psychopharmacology. Biol Psychiatry. 2006;59:1001–5.
Furukawa TA, Barbui C, Cipriani A, Brambilla P, Watanabe N. Imputing missing standard deviations in meta-analyses can provide accurate results. J Clin Epidemiol. 2006;59:7–10.
Salanti G, Higgins JP, White IR. Bayesian synthesis of epidemiological evidence with different combinations of exposure groups: application to a gene-gene-environment interaction. Stat Med. 2006;25:4147–63.
Furukawa TA, Levine SZ, Tanaka S, Goldberg Y, Samara M, Davis JM, et al. Initial severity of schizophrenia and efficacy of antipsychotics: participant-level meta-analysis of 6 placebo-controlled studies. JAMA Psychiatry. 2015;72:14–21.
Rabinowitz J, Werbeloff N, Caers I, Mandel FS, Stauffer V, Menard F, et al. Determinants of antipsychotic response in schizophrenia: implications for practice and future clinical trials. J Clin Psychiatry. 2014;75:e308–16.
Mattila T, Wohlfarth T, Koeter M, Storosum J, van den Brink W, de Haan L, et al. Geographic variation in efficacy of atypical antipsychotics for the acute treatment of schizophrenia-an individual patient data meta-analysis. Eur Neuropsychopharmacol: J Eur Coll Neuropsychopharmacol. 2014;24:1067–77.
Rabinowitz J, Levine SZ, Barkai O, Davidov O. Dropout rates in randomized clinical trials of antipsychotics: a meta-analysis comparing first- and second-generation drugs and an examination of the role of trial design features. Schizophr Bull. 2009;35:775–88.
Levine SZ, Goldberg Y, Samara M, Davis JM, Leucht S. Joint modeling of dropout and outcome in three pivotal clinical trials of schizophrenia. Schizophr Res. 2015;164:122–6.
Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias: dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA. 1995;273:408–12.
Wood L, Egger M, Gluud LL, Schulz KF, Juni P, Altman DG, et al. Empirical evidence of bias in treatment effect estimates in controlled trials with different interventions and outcomes: meta-epidemiological study. BMJ. 2008;336:601–5.
Porta N, Bonet C, Cobo E. Discordance between reported intention-to-treat and per protocol analyses. J Clin Epidemiol. 2007;60:663–9.
Egger M, Davey mG, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34.
Heres S, Davis J, Maino K, Jetzinger E, Kissling W, Leucht S. Why olanzapine beats risperidone, risperidone beats quetiapine, and quetiapine beats olanzapine: an exploratory analysis of head-to-head comparison studies of second-generation antipsychotics. Am J Psychiatry. 2006;163:185–94.
Zohar J, Stahl S, Moller HJ, Blier P, Kupfer D, Yamawaki S, et al. A review of the current nomenclature for psychotropic agents and an introduction to the Neuroscience-based Nomenclature. Eur Neuropsychopharmacol. 2015;25:2318–25.
Gardner DM, Murphy AL, O’Donnell H, Centorrino F, Baldessarini RJ. International consensus study of antipsychotic dosing. Am J Psychiatry. 2010;167:686–93.
Simmonds MC, Higgin JP. Covariate heterogeneity in meta-analysis: criteria for deciding between meta-regression and individual patient data. Stat Med. 2007;26:2982–99.
Tzimos A, Samokhvalov V, Kramer M, Ford L, Gassmann-Mayer C, Lim P, et al. Safety and Tolerability of Oral Paliperidone Extended-Release Tablets in Elderly Patients With Schizophrenia: A Double-Blind, Placebo-Controlled Study With Six-Month Open-Label Extension Am J Geriatr Psychiatry. 2008;16:31–43.
Acknowledgements
We thank Georgia Salanti for her initial help in developing the statistical method, Samantha Roberts for her help in the literature search, Magdolna Tardy, M.Sc, for her help in study selection and Marc Krause, Philipp Rothe, MD, Thomas Arndt and Matteo Rabaioli, Susanne Bächer, Natalie Peter for help in data extraction. Ole Andreassen, Guy Chouinard, Michael Jann, Herbert Meltzer, Ofer Agid, Bret Rutherford, Merck, Dainippon Sumitomo, Novartis, Sunovion, EliLilly, Johnson&Johnson and Pfizer have replied to our requests for explanations or data. We could also again use the data that authors had sent us for requests in the context of previous meta-analyses of our group.
Author information
Authors and Affiliations
Contributions
SL, A Chaimani, DM, and JMD were involved in designing the review. MH, MT, and SL identified and acquired reports of trials. CL, MH, BH, MS, MR, SB, MK, PR, TA, NP, and SL extracted data. SL and CL contacted authors of trials and pharmaceutical industries for additional information. SL, A Chaimani, and DM analyzed and interpreted the data. A Chaimani and JRG contributed to the interpretation of the data. SL, A Chaimani, A Cipriani, and BH drafted the manuscript and all other authors critically reviewed the manuscript for important intellectual content. All authors approved the final version.
Corresponding author
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Leucht, S., Chaimani, A., Mavridis, D. et al. Disconnection of drug-response and placebo-response in acute-phase antipsychotic drug trials on schizophrenia? Meta-regression analysis. Neuropsychopharmacol. 44, 1955–1966 (2019). https://doi.org/10.1038/s41386-019-0440-6
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41386-019-0440-6
This article is cited by
-
Negative Symptoms in Schizophrenia: An Update on Research Assessment and the Current and Upcoming Treatment Landscape
CNS Drugs (2025)
-
Knowing is Half the Battle: The Factors Leading to Efficient Recruitment of Representative Samples in Schizophrenia Research
Pharmaceutical Medicine (2025)
-
Finding new and better treatments for psychiatric disorders
Neuropsychopharmacology (2024)
-
Placebo effects in randomized trials of pharmacological and neurostimulation interventions for mental disorders: An umbrella review
Molecular Psychiatry (2024)
-
Placebo response in pharmacological and dietary supplement trials of autism spectrum disorder (ASD): systematic review and meta-regression analysis
Molecular Autism (2020)