Abstract
Prior observational studies have suggested that medications targeting the renin–angiotensin system, such as angiotensin-converting enzyme inhibitors (ACE-Is) and angiotensin receptor blockers (ARBs), may be associated with decreased PTSD symptoms. Given known sex differences in PTSD prevalence and cardiovascular disease, here we tested whether the effects of ACE-I/ARB status on PTSD differ by sex. We also expanded these observations with replication analyses in a large biorepository database. Participants in the initial sample included 840 trauma-exposed individuals recruited as part of the Grady Trauma Project. The Modified PTSD Symptom Scale (M-PSS) was administered and ACE-I/ARB status was determined by self-report. Replication analyses were conducted using a large biorepository database (Partners Healthcare Biobank, N = 116,389) with diagnoses and medication status based on available electronic health records. Among individuals treated with ACE-Is/ARBs in the initial sample, women had significantly higher M-PSS total and Re-experiencing severity compared to men (p’s < 0.05). Analyses with the large biorepository sample robustly replicated the overall effects of ACE-I/ARB medication associated with lower rate of PTSD diagnosis (p < 0.001). We also demonstrated that this effect may be specific to the renin–angiotensin system as it did not replicate for beta-blockers, calcium channel blockers, or diuretics. When we examined more specific drug classes, results indicated that the ACE-I/ARB effect on PTSD may be driven more by ARBs (e.g., Losartan) than by ACE-Is. Post-hoc analyses indicated that racial differences may exist in these effects. Overall, our results replicate and extend prior observations that the renin–angiotensin system is associated with PTSD. Medications targeting this system may be worthy of further investigation for PTSD treatment. Our findings suggest that sex and race effects should be considered in future treatment research.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52:1048–60.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington, VA: American Psychiatric Association; 2013.
Michopoulos V, Norrholm SD, Jovanovic T. Diagnostic biomarkers for posttraumatic stress disorder: promising horizons from translational neuroscience research. Biol Psychiatry. 2015;78:344–53.
Edmondson D, Kronish IM, Shaffer JA, Falzon L, Burg MM. Posttraumatic stress disorder and risk for coronary heart disease: a meta-analytic review. Am Heart J. 2013;166:806–14.
Edmondson D, von Känel R. Post-traumatic stress disorder and cardiovascular disease. Lancet Psychiatry. 2017;4:320–9.
Myers B. Corticolimbic regulation of cardiovascular responses to stress. Physiol Behav. 2017;172:49–59.
Spitzer C, Barnow S, Völzke H, John U, Freyberger HJ, Grabe HJ. Trauma, posttraumatic stress disorder, and physical illness: findings from the general population. Psychosom Med. 2009;71:1012–7.
Byku M, Macarthur H, Westfall TC. Nerve stimulation induced overflow of neuropeptide Y and modulation by angiotensin II in spontaneously hypertensive rats. Am J Physiol Heart Circ Physiol. 2008;295:H2188–97.
Mackins CJ, Kano S, Seyedi N, Schäfer U, Reid AC, Machida T, et al. Cardiac mast cell–derived renin promotes local angiotensin formation, norepinephrine release, and arrhythmias in ischemia/reperfusion. J Clin Investig. 2006;116:1063–70.
Osborn JW, Fink GD. Region-specific changes in sympathetic nerve activity in angiotensin II–salt hypertension in the rat. Exp Physiol. 2010;95:61–8.
Reid AC, Mackins CJ, Seyedi N, Levi R, Silver RB. Coupling of angiotensin II AT1 receptors to neuronal NHE activity and carrier-mediated norepinephrine release in myocardial ischemia. Am J Physiol Heart Circ Physiol. 2004;286:H1448–54.
Terock J, Hannemann A, Janowitz D, Freyberger HJ, Felix SB, Dörr M, et al. Associations of trauma exposure and post-traumatic stress disorder with the activity of the renin-angiotensin-aldosterone-system in the general population. Psychol Med. 2019;49:843–51.
Weber MA. Angiotensin-II receptor blockers for hypertension and heart failure: quality of life and outcomes. Manag Care Interface. 2005;18:47–54.
Zanchetti A, Elmfeldt D. Findings and implications of the Study on Cognition and Prognosis in the Elderly (SCOPE)—a review. Blood Press. 2006;15:71–79.
Khoury NM, Marvar PJ, Gillespie CF, Wingo A, Schwartz A, Bradley B, et al. The renin-angiotensin pathway in posttraumatic stress disorder: angiotensin-converting enzyme inhibitors and angiotensin receptor blockers are associated with fewer traumatic stress symptoms. J Clin Psychiatry. 2012;73:849–55.
Nylocks KM, Michopoulos V, Rothbaum AO, Almli L, Gillespie CF, Wingo A, et al. An angiotensin-converting enzyme (ACE) polymorphism may mitigate the effects of angiotensin-pathway medications on posttraumatic stress symptoms. Am J Med Genet B Neuropsychiatr Genet. 2015;168B:307–15.
Gillespie CF, Bradley B, Mercer K, Smith AK, Conneely K, Gapen M, et al. Trauma exposure and stress-related disorders in inner city primary care patients. Gen Hosp Psychiatry. 2009;31:505–14.
Schwartz AC, Bradley RL, Sexton M, Sherry A, Ressler KJ. Posttraumatic stress disorder among African Americans in an inner city mental health clinic. Psychiatr Serv. 2005;56:212–5.
Schwartz AC, Bradley R, Penza KM, Sexton M, Jay D, Haggard PJ, et al. Pain medication use among patients with posttraumatic stress disorder. Psychosomatics. 2006;47:136–42.
Bernstein DP, Fink L, Handelsman L, Foote J, Lovejoy M, Wenzel K, et al. Initial reliability and validity of a new retrospective measure of child abuse and neglect. Am J Psychiatry. 1994;151:1132–6.
Falsetti SA, Resnick HS, Resick PA, Kilpatrick DG. The Modified PTSD Symptom Scale: A brief self-report measure of posttraumatic stress disorder. Behav Ther. 1993;16:161–2.
Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. San Antonia, TX: Psychological Corporation; 1996.
Rytwinski NK, Scur MD, Feeny NC, Youngstrom EA. The co-occurrence of major depressive disorder among individuals with posttraumatic stress disorder: a meta-analysis. J Trauma Stress. 2013;26:299–309.
Vian J, Pereira C, Chavarria V, Köhler C, Stubbs B, Quevedo J, et al. The renin–angiotensin system: a possible new target for depression. BMC Med. 2017;15:144.
Jovanovic T, Norrholm SD, Fennell JE, Keyes M, Fiallos AM, Myers KM, et al. Posttraumatic stress disorder may be associated with impaired fear inhibition: relation to symptom severity. Psychiatry Res. 2009;167:151–60.
Glover EM, Jovanovic T, Mercer KB, Kerley K, Bradley B, Ressler KJ, et al. Estrogen levels are associated with extinction deficits in women with posttraumatic stress disorder. Biol Psychiatry. 2012;72:19–24.
Glover EM, Jovanovic T, Norrholm SD. Estrogen and extinction of fear memories: implications for posttraumatic stress disorder treatment. Biol Psychiatry. 2015;78:178–85.
Wegerer M, Kerschbaum H, Blechert J, Wilhelm FH. Low levels of estradiol are associated with elevated conditioned responding during fear extinction and with intrusive memories in daily life. Neurobiol Learn Mem. 2014;116:145–54.
Longcope C, Franz C, Morello C, Baker R, Johnston CC Jr. Steroid and gonadotropin levels in women during the peri-menopausal years. Maturitas. 1986;8:189–96.
Marvar PJ, Goodman J, Fuchs S, Choi DC, Banerjee S, Ressler KJ. Angiotensin type 1 receptor inhibition enhances the extinction of fear memory. Biol Psychiatry. 2014;75:864–72.
Hurt RC, Garrett JC, Keifer OP Jr, Linares A, Couling L, Speth RC, et al. Angiotensin type 1a receptors on corticotropin-releasing factor neurons contribute to the expression of conditioned fear. Genes Brain Behav. 2015;14:526–33.
Saavedra JM, Benicky J. Brain and peripheral angiotensin II play a major role in stress. Stress. 2007;10:185–93.
Author information
Authors and Affiliations
Contributions
AVS analyzed the data and wrote the manuscript. LAD analyzed the data and contributed to writing the manuscript. JBM, PJM, and MBS contributed to writing the manuscript. VM, CFG, and KJR conceived and executed the parent project, and contributed to editing the manuscript. All authors reviewed and edited the final manuscript.
Corresponding author
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Seligowski, A.V., Duffy, L.A., Merker, J.B. et al. The renin–angiotensin system in PTSD: a replication and extension. Neuropsychopharmacol. 46, 750–755 (2021). https://doi.org/10.1038/s41386-020-00923-1
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41386-020-00923-1
This article is cited by
-
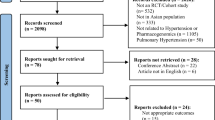
Use of renin-angiotensin system blockers and posttraumatic stress disorder risk in the UK Biobank: a retrospective cohort study
BMC Medicine (2024)
-
Psychological and biological mechanisms linking trauma with cardiovascular disease risk
Translational Psychiatry (2023)
-
Onset and recurrence of psychiatric disorders associated with anti-hypertensive drug classes
Translational Psychiatry (2021)