Abstract
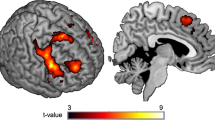
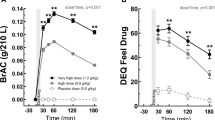
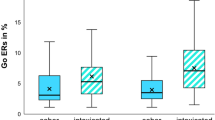
One well-known phenotypic risk factor for the development of alcohol use disorder is sensitivity to the rewarding effects of alcohol. In the present study, we examined whether individuals who are sensitive to alcohol reward are also sensitive to nondrug rewards, thereby reflecting a broader individual difference risk factor. Specifically, we tested the hypothesis that subjective response to acute rewarding effects of alcohol would be related to neural activation during monetary reward receipt relative to loss (in the absence of alcohol). Community-recruited healthy young social drinkers (N = 58) completed four laboratory sessions in which they received alcohol (0.8 g/kg) and placebo in alternating order under double-blind conditions, providing self-report measures of subjective response to alcohol at regular intervals. At a separate visit 1–3 weeks later, they completed a reward-guessing game, the ‘Doors’ task, during fMRI in a drug-free state. Participants who reported greater motivation (i.e., wanting) to consume more alcohol after a single moderate dose of alcohol also exhibited greater neural activation in the bilateral ventral caudate and the nucleus accumbens during reward receipt relative to loss. Striatal activation was not related to other subjective ratings including alcohol-induced sedation, stimulation, or pleasure (i.e., feeling, liking). Our study is the first to show that measures of alcohol reward are related to neural indices of monetary reward in humans. These results support growing evidence that individual differences in responses to drug and nondrug reward are linked and together form a risk profile for drug use or abuse, particularly in young adults.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Room R, Babor T, Rehm J. Alcohol and public health. Lancet. 2005;365:519–30.
Dawson DA, Grant BF. The “Gray area” of consumption between moderate and risk drinking. J Stud Alcohol Drugs. 2011;72:453–8.
Sudhinaraset M, Wigglesworth C, Takeuchi DT. Social and cultural contexts of alcohol use: Influences in a social–ecological framework. Alcohol Res Curr Rev. 2016;38:35–45.
Morean ME, Corbin WR. Subjective response to alcohol: a critical review of the literature. Alcohol Clin Exp Res. 2010;34:385–95.
Ray LA, MacKillop J, Monti PM. Subjective responses to alcohol consumption as endophenotypes: advancing behavioral genetics in etiological and treatment models of alcoholism. Subst Use Misuse. 2010;45:1742–65.
King AC, McNamara PJ, Hasin DS, Cao D. Alcohol challenge responses predict future alcohol use disorder symptoms: a 6-year prospective study. Biol Psychiatry. 2014;75:798–806.
Schuckit MA. Low level of response to alcohol as a predictor of future alcoholism. Am J Psychiatry. 1994;151:184–9.
King AC, De Wit H, McNamara PJ, Cao D. Rewarding, stimulant, and sedative alcohol responses and relationship to future binge drinking. Arch Gen Psychiatry. 2011;68:389–99.
Koob GF, Volkow ND. Neurocircuitry of addiction. Neuropsychopharmacology. 2010;35:217–38.
Koob GF, Volkow ND. Neurobiology of addiction: a neurocircuitry analysis. Lancet Psychiatry. 2016;3:760–73.
Lüscher C, Malenka RC. Drug-evoked synaptic plasticity in addiction: from molecular changes to circuit remodeling. Neuron.2011;69:650–63.
Di Chiara G. Alcohol and dopamine. Alcohol Health Res World. 1997;21:108–14.
Clarke R, Adermark L. Dopaminergic regulation of striatal interneurons in reward and addiction: focus on alcohol. Neural Plast. 2015;2015:1–11.
Charlet K, Beck A, Heinz A. The dopamine system in mediating alcohol effects in humans. Curr Top Behav Neurosci. 2011;13:461–88.
Tupala E, Tiihonen J. Dopamine and alcoholism: neurobiological basis of ethanol abuse. Prog Neuro-Psychopharmacol Biol Psychiatry. 2004;28:1221–47.
Ramchandani VA, Umhau J, Pavon FJ, Ruiz-Velasco V, Margas W, Sun H, et al. A genetic determinant of the striatal dopamine response to alcohol in men. Mol Psychiatry. 2011;16:809–17.
Urban NBL, Kegeles LS, Slifstein M, Xu X, Martinez D, Sakr E, et al. Sex differences in striatal dopamine release in young adults after oral alcohol challenge: a positron emission tomography imaging study with [11C]raclopride. Biol Psychiatry. 2010;68:689–96.
Boileau I, Assaad JM, Pihl RO, Benkelfat C, Leyton M, Diksic M, et al. Alcohol promotes dopamine release in the human nucleus accumbens. Synapse. 2003;49:226–31.
Setiawan E, Pihl RO, Dagher A, Schlagintweit H, Casey KF, Benkelfat C, et al. Differential striatal dopamine responses following oral alcohol in individuals at varying risk for dependence. Alcohol Clin Exp Res. 2014;38:126–34.
Yoder KK, Albrecht DS, Dzemidzic M, Normandin MD, Federici LM, Graves T, et al. Differences in IV alcohol-induced dopamine release in the ventral striatum of social drinkers and nontreatment-seeking alcoholics. Drug Alcohol Depend. 2016;160:163–9.
Kegeles LS, Horga G, Ghazzaoui R, Rosengard R, Ojeil N, Xu X, et al. Enhanced striatal dopamine release to expectation of alcohol: a potential risk factor for alcohol use disorder. Biol Psychiatry Cognit Neurosci Neuroimaging. 2018;3:591–8.
Yoder KK, Constantinescu CC, Kareken DA, Normandin MD, Cheng T-E, O’Connor SJ, et al. Heterogeneous effects of alcohol on dopamine release in the striatum: a PET study. Alcohol Clin Exp Res. 2007;31:965–73.
Yoder KK, Kareken DA, Seyoum RA, O’Connor SJ, Wang C, Zheng Q-H, et al. Dopamine D2 receptor availability is associated with subjective responses to alcohol. Alcohol Clin Exp Res. 2005;29:965–70.
Gilman JM, Ramchandani VA, Davis MB, Bjork JM, Hommer DW. Why we like to drink: a functional magnetic resonance imaging study of the rewarding and anxiolytic effects of alcohol. J Neurosci. 2008;28:4583–91.
Gilman JM, Ramchandani VA, Crouss T, Hommer DW. Subjective and neural responses to intravenous alcohol in young adults with light and heavy drinking patterns. Neuropsychopharmacology. 2012;37:467–77.
Weafer J, Ross TJ, O’Connor S, Stein EA, de Wit H, Childs E. Striatal activity correlates with stimulant-like effects of alcohol in healthy volunteers. Neuropsychopharmacology. 2018;43:2532–8.
Sescousse G, Caldú X, Segura B, Dreher JC. Processing of primary and secondary rewards: a quantitative meta-analysis and review of human functional neuroimaging studies. Neurosci Biobehav Rev. 2013;37:681–96.
Olsen CM. Natural rewards, neuroplasticity, and non-drug addictions. Neuropharmacology. 2011;61:1109–22.
McCabe C, Mishor Z, Cowen PJ, Harmer CJ. Diminished neural processing of aversive and rewarding stimuli during selective serotonin reuptake inhibitor treatment. Biol Psychiatry. 2010;67:439–45.
Berns GS, McClure SM, Pagnoni G, Montague PR. Predictability modulates human brain response to reward. J Neurosci. 2001;21:2793–8.
McClure SM, Berns GS, Montague PR. Temporal prediction errors in a passive learning task activate human striatum. Neuron. 2003;38:339–46.
Pagnoni G, Zink CF, Montague PR, Berns GS. Activity in human ventral striatum locked to errors of reward prediction. Nat Neurosci. 2002;5:97–8.
Arnow BA, Desmond JE, Banner LL, Glover GH, Solomon A, Polan ML, et al. Brain activation and sexual arousal in healthy, heterosexual males. Brain. 2002;125:1014–23.
Breiter HC, Aharon I, Kahneman D, Dale A, Shizgal P. Functional imaging of neural responses to expectancy and experience of monetary gains and losses. Neuron. 2001;30:619–39.
Delgado MR, Stenger VA, Fiez JA. Motivation-dependent responses in the human caudate nucleus. Cereb Cortex. 2004;14:1022–30.
Delgado MR, Nystrom LE, Fissell C, Noll DC, Fiez JA. Tracking the hemodynamic responses to reward and punishment in the striatum. J Neurophysiol. 2000;84:3072–7.
Elliott R, Friston KJ, Dolan RJ. Dissociable neural responses in human reward systems. J Neurosci. 2000;20:6159–65.
Izuma K, Saito DN, Sadato N. Processing of social and monetary rewards in the human striatum. Neuron. 2008;58:284–94.
Knutson B, Westdorp A, Kaiser E, Hommer D. FMRI visualization of brain activity during a monetary incentive delay task. Neuroimage. 2000;12:20–7.
Nieuwenhuis S, Heslenfeld DJ, von Geusau NJA, Mars RB, Holroyd CB, Yeung N. Activity in human reward-sensitive brain areas is strongly context dependent. Neuroimage. 2005;25:1302–9.
Thut G, Schultz W, Roelcke U, Nienhusmeier M, Missimer J, Maguire RP, et al. Activation of the human brain by monetary reward. Neuroreport. 1997;8:1225–8.
Zald DH, Boileau I, El-Dearedy W, Gunn R, McGlone F, Dichter GS, et al. Dopamine transmission in the human striatum during monetary reward tasks. J Neurosci. 2004;24:4105–12.
Berridge KC, Robinson TE. Liking, wanting, and the incentive-sensitization theory of addiction. Am Psychol. 2016;71:670–9.
Kelley AE, Berridge KC. The neuroscience of natural rewards: relevance to addictive drugs. J Neurosci. 2002;22:3306–11.
Goldstein RZ, Woicik PA, Moeller SJ, Telang F, Jayne M, Wong C, et al. Liking and wanting of drug and non-drug rewards in active cocaine users: the STRAP-R questionnaire. J Psychopharmacol. 2010;24:257–66.
Bustamante J-C, Barrós-Loscertales A, Costumero V, Fuentes-Claramonte P, Rosell-Negre P, Ventura-Campos N, et al. Abstinence duration modulates striatal functioning during monetary reward processing in cocaine patients. Addict Biol. 2014;19:885–94.
Jia Z, Worhunsky PD, Carroll KM, Rounsaville BJ, Stevens MC, Pearlson GD, et al. An initial study of neural responses to monetary incentives as related to treatment outcome in cocaine dependence. Biol Psychiatry. 2011;70:553–60.
Bühler M, Vollstädt-Klein S, Kobiella A, Budde H, Reed LJ, Braus DF, et al. Nicotine dependence is characterized by disordered reward processing in a network driving motivation. Biol Psychiatry. 2010;67:745–52.
Wrase J, Schlagenhauf F, Kienast T, Wüstenberg T, Bermpohl F, Kahnt T, et al. Dysfunction of reward processing correlates with alcohol craving in detoxified alcoholics. Neuroimage.2007;35:787–94.
Heather Nick, Segal G. Addiction & choice: rethinking the relationship. 1st ed. New York, NY: Oxford University Press; 2016
Crane NA, Gorka SM, Weafer J, Langenecker SA, De Wit H, Phan KL. Neural activation to monetary reward is associated with amphetamine reward sensitivity. Neuropsychopharmacology. 2018;43:1738–44.
Langenecker SA, Kling LR, Crane NA, Gorka SM, Nusslock R, Damme KSF, et al. Anticipation of monetary reward in amygdala, insula, caudate are predictors of pleasure sensitivity to d-Amphetamine administration. Drug Alcohol Depend. 2020;206:107725.
Liu X, Hairston J, Schrier M, Fan J. Common and distinct networks underlying reward valence and processing stages: a meta-analysis of functional neuroimaging studies. Neurosci Biobehav Rev. 2011;35:1219–36.
Kirkpatrick MG, De Wit H. In the company of others: social factors alter acute alcohol effects. Psychopharmacol. 2013;230:215–26.
Weafer J, Gallo DA, de Wit H. Effect of alcohol on encoding and consolidation of memory for alcohol-related images. Alcohol Clin Exp Res. 2016;40:1540–7.
First MB, Williams JBW, Karg RSSR. Structured clinical interview for DSM-5-research version (SCID-5 for DSM-5, Research Version; SCID-5-RV). Arlington, VA: American Psychiatric Association; 2015.
Weafer J, de Wit H, Weafer J, Phan KL. Poor inhibitory control is associated with greater stimulation and less sedation following alcohol. Psychopharmacology. 2019:1–8.
Rhodes JD, Hawk LW. Smoke and mirrors: the overnight abstinence paradigm as an index of disrupted cognitive function. Psychopharmacol. 2016;233:1395–404.
Murray CH, Weafer J, de Wit H. Stability of acute responses to drugs in humans across repeated testing: findings with alcohol and amphetamine. Drug Alcohol Depend. 2020:107989. (in press).
Sutker PB, Tabakoff B, Goist KC, Randall CL. Acute alcohol intoxication, mood states and alcohol metabolism in women and men. Pharmacol Biochem Behav. 1983;18:349–54.
Fillmore MT. Cognitive preoccupation with alcohol and binge drinking in college students: alcohol-induced priming of the motivation to drink. Psychol Addict Behav. 2001;15:325–32.
Doty P, de Wit H. Effect of setting on the reinforcing and subjective effects of ethanol in social drinkers. Psychopharmacol. 1995;118:19–27.
Martin CS, Earleywine M, Musty RE, Perrine MW, Swift RM. Development and validation of the biphasic alcohol effects scale. Alcohol Clin Exp Res. 1993;17:140–6.
Morean ME, de Wit H, King AC, Sofuoglu M, Rueger SY, O’Malley SS. The drug effects questionnaire: psychometric support across three drug types. Psychopharmacol. 2013;227:177–92.
Crane NA, Gorka SM, Weafer J, Langenecker SA, de Wit H, Phan KL. Preliminary evidence for disrupted nucleus accumbens reactivity and connectivity to reward in binge drinkers. Alcohol Alcohol. 2017;52:647–54.
Hajcak G, Moser JS, Holroyd CB, Simons RF. The feedback-related negativity reflects the binary evaluation of good versus bad outcomes. Biol Psychol. 2006;71:148–54.
Foti D, Hajcak G. Depression and reduced sensitivity to non-rewards versus rewards: evidence from event-related potentials. Biol Psychol. 2009;81:1–8.
Carlson JM, Foti D, Mujica-Parodi LR, Harmon-Jones E, Hajcak G. Ventral striatal and medial prefrontal BOLD activation is correlated with reward-related electrocortical activity: a combined ERP and fMRI study. Neuroimage. 2011;57:1608–16.
Power JD, Barnes KA, Snyder AZ, Schlaggar BL, Petersen SE. Spurious but systematic correlations in functional connectivity MRI networks arise from subject motion. Neuroimage. 2012;59:2142–54.
Yarkoni T, Poldrack RA, Nichols TE, Van Essen DC, Wager TD. Large-scale automated synthesis of human functional neuroimaging data. Nat Methods. 2011;8:665–70.
Cox RW. AFNI: software for analysis and visualization of functional magnetic resonance neuroimages. Comput Biomed Res. 1996;29:162–73.
Lüdecke D. sjplot: Data visualization for statistics in social science. 2018.
Wickham H. Ggplot2: elegrant graphics for data analysis. 2016.
Molochnikov I, Cohen D. Hemispheric differences in the mesostriatal dopaminergic system. Front Syst Neurosci. 2014;8:1–14.
De Wit H. Priming effects with drugs and other reinforcers. Exp Clin Psychopharmacol. 1996;4:5–10.
de Wit H, Chutuape MA. Increased ethanol choice in social drinkers following ethanol preload. Behav Pharmacol. 1993;4:29–36.
Kirk JM, De Wit H. Individual differences in the priming effect of ethanol in social drinkers. J Stud Alcohol. 2000;61:64–71.
Pool E, Sennwald V, Delplanque S, Brosch T, Sander D. Measuring wanting and liking from animals to humans: a systematic review. Neurosci Biobehav Rev. 2016;63:124–42.
Robinson MJF, Fischer AM, Ahuja A, Lesser EN, Maniates H. Roles of “wanting” and “liking” in motivating behavior: gambling, food, and drug addictions. Curr Top Behav Neurosci. 2016;27:105–36.
Zink CF, Pagnoni G, Martin-Skurski ME, Chappelow JC, Berns GS. Human striatal responses to monetary reward depend on saliency. Neuron.2004;42:509–17.
Berridge KC, Robinson TE, Aldridge JW. Dissecting components of reward: ‘liking’, ‘wanting’, and learning. Curr Opin Pharmacol. 2009;9:65–73.
Zink CF, Pagnoni G, Martin ME, Dhamala M, Berns GS. Human striatal response to salient nonrewarding stimuli. J Neurosci. 2003;23:8092–7.
Leyton M, Casey KF, Delaney JS, Kolivakis T, Benkelfat C. Cocaine craving, euphoria, and self-administration: a preliminary study of the effect of catecholamine precursor depletion. Behav Neurosci. 2005;119:1619–27.
Hardman CA, Herbert VMB, Brunstrom JM, Munafò MR, Rogers PJ. Dopamine and food reward: effects of acute tyrosine/phenylalanine depletion on appetite. Physiol Behav. 2012;105:1202–7.
Evans AH, Pavese N, Lawrence AD, Tai YF, Appel S, Doder M, et al. Compulsive drug use linked to sensitized ventral striatal dopamine transmission. Ann Neurol. 2006;59:852–8.
Smith CT, Dang LC, Cowan RL, Kessler RM, Zald DH. Variability in paralimbic dopamine signaling correlates with subjective responses to d-amphetamine. Neuropharmacology. 2016;108:394–402.
Volkow ND, Wang GJ, Fowler JS, Logan J, Jayne M, Franceschi D, et al. ‘Nonhedonic’ food motivation in humans involves dopamine in the dorsal striatum and methylphenidate amplifies this effect. Synapse. 2002;44:175–80.
Leyton M, Boileau I, Benkelfat C, Diksic M, Baker G, Dagher A. Amphetamine-induced increases in extracellular dopamine, drug wanting, and novelty seeking: a PET/[11C]raclopride study in healthy men. Neuropsychopharmacology. 2002;27:1027–35.
Luijten M, Schellekens AF, Kühn S, MacHielse MWJ, Sescousse G. Disruption of reward processing in addiction: an image-based meta-analysis of functional magnetic resonance imaging studies. JAMA Psychiatry. 2017;74:387–98.
Author information
Authors and Affiliations
Contributions
HdW and KLP were the principal investigators of the study. HdW, KLP, and SAL contributed to the conceptual design of the study, made important contributions to the editing of the paper and assisted in data analysis and interpretation. MR conducted the statistical analyses, interpreted the data, and wrote the initial draft of the paper. NAC, SMG, and JW assisted in paper preparation.
Corresponding author
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Radoman, M., Crane, N.A., Gorka, S.M. et al. Striatal activation to monetary reward is associated with alcohol reward sensitivity. Neuropsychopharmacol. 46, 343–350 (2021). https://doi.org/10.1038/s41386-020-0728-6
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41386-020-0728-6
This article is cited by
-
Methamphetamine alters nucleus accumbens neural activation to monetary loss in healthy young adults
Psychopharmacology (2023)
-
Acute orexin antagonism selectively modulates anticipatory anxiety in humans: implications for addiction and anxiety
Translational Psychiatry (2022)
-
Neural correlates of inhibitory control are associated with stimulant-like effects of alcohol
Neuropsychopharmacology (2021)